doi: 10.56294/hl202297
ORIGINAL
Exploring the Impact of Interprofessional Education on Teamwork and Communication in Healthcare Settings
Exploración del impacto de la educación interprofesional en el trabajo en equipo y la comunicación en los entornos sanitarios
A Geetha Bhavani1
![]() , Sujayaraj Samuel Jayakumar2
, Sujayaraj Samuel Jayakumar2
![]() , Suvendu Narayan Mishra3
, Suvendu Narayan Mishra3
![]()
1Noida International University, Department of Chemistry. Greater Noida, India.
2JAIN (Deemed-to-be University), Department of Forensic Science. Bangalore, India.
3Siksha ‘O’ Anusandhan (Deemed to be University), Department of Psychiatry, IMS and SUM Hospital. Bhubaneswar, India.
Cite as: Bhavani AG, Jayakumar SS, Suvendu Narayan Mishra SNM. Exploring the Impact of Interprofessional Education on Teamwork and Communication in Healthcare Settings. Health Leadership and Quality of Life. 2022; 1:97. https://doi.org/10.56294/hl202297
Submitted: 23-07-2022 Revised: 11-10-2022 Accepted: 05-12-2022 Published: 06-12-2022
Editor:
PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: systematic and meta-analysis of quantitative and qualitative studies that assessed the effect of IPE on teamwork and communication. These findings evaluate the potential qualities of IPE in the healthcare context.
Method: in the literature review, 25 studies were developed through electronic databases and manual searches, and a total of 2500 relevant articles were identified. The meta-analysis of 15 studies with a relative sample size of 1800 participants.
Results: the results of the literature review, including the meta-analysis, were grouped into three overarching themes: Strategies for IPE, Aspects of IPE, and Difficulties of IPE.
Conclusions: to sum up, this study has shown positive results regarding IPE’s impact on teamwork and communication in the health services environment. The study conclusions indicate that IPE methods can support a more collaborative and patient-centered style of health care.
Keywords: Healthcare; Meta-Analysis; Qualities; Patient-Centered; Participants.
RESUMEN
Introducción: sistemática y metaanálisis de estudios cuantitativos y cualitativos que evalúan el efecto de la EPI sobre el trabajo en equipo y la comunicación. Estos resultados evalúan las cualidades potenciales de la EIP en el contexto sanitario.
Método: en la revisión bibliográfica se desarrollaron 25 estudios a través de bases de datos electrónicas y búsquedas manuales, y se identificaron un total de 2500 artículos relevantes. El metaanálisis de 15 estudios con un tamaño muestral relativo de 1800 participantes.
Resultados: los resultados de la revisión bibliográfica, incluido el metaanálisis, se agruparon en tres temas generales: Estrategias para la EPI, Aspectos de la EPI y Dificultades de la EPI.
Conclusiones: en resumen, este estudio ha mostrado resultados positivos en cuanto al impacto de la EPI en el trabajo en equipo y la comunicación en el entorno de los servicios sanitarios. Las conclusiones del estudio indican que los métodos de IPE pueden apoyar un estilo de atención sanitaria más colaborativo y centrado en el paciente.
Palabras clave: Atención Sanitaria; Metaanálisis; Cualidades; Centrada en el Paciente; Participantes.
INTRODUCTION
IPE is an intentional opportunity for students from different health professions to learn collaboratively and provide skills and knowledge translational to clinical practice settings with a focus on teamwork and communication. IPE prepares health professions students for effective and efficient collaboration in providing patient-centered care.(1) We highlight healthcare IPE in this essay and how it can boost the team and communication effort. Teamwork and Communication in the Healthcare Teamwork; and particularly, communication are critical to the delivery of both safe and effective patient care in healthcare settings. Effective teamwork among healthcare professionals is dedicated to providing the best possible patient care, encouraging common goals to complete tasks to share information and expertise while being actively involved in related responsibilities.(2) It emphasizes a collaborative mechanism of problem solving and decision making. On the contrary, effective communication is imperative for improving patient safety through salient and timely communication among the members of the team.(3) Poor teamwork and poor communication can contribute to medical mistakes, poor patient outcomes, or indeed a loss of health itself on positive delivery of care. This is team work and communication, thanks to IPE.(4) By bringing students from different professions of healthcare together, IPE aims to minimize professional barriers and facilitate a better understanding of the roles in an interprofessional team (source). While preparing for a future construction project at a health facility, construction related activities need to be distributed among the different trades. IPE helps students gain knowledge and understanding of what healthcare providers do.(5) This knowledge encourages collaboration and communication, knowing what strengths and skills each team member has to offer. They are able to communicate and delegate when appropriate which translates to better quality patient care. In addition to exposing students to skills such as active listening, clear and concise communication and assertiveness, IPE also teaches students how to voice their opinions and how to disagree respectfully.(6) A critical aspect of what these skilled persons offer health care professionals is the ability to communicate to patients and their families and other team members. Before we talk about more about IPE, we should know the role of interprofessional relations amongst health care professionals. Significant LiteratureStudents from different health professions gain more appreciation and better understanding of one another’s role when learning together.(7) This can promote improved communication and collaboration among health care practitioners in a real life health care setting. Benefits of IPE Regarding Teamwork and Communication Many benefits of IPE do abound on teamwork and communication not only in health care settings. One of the major advantages is the enhancement of patient outcomes. Collaboration and communication are essential to safe, effective patient care.(8) Improving these abilities through IPE can help healthcare workers avoid medical mistakes, eradicate patient wrap damage, and improve patient satisfaction. In addition, IPE enhances job satisfaction and reduces burnout in the healthcare professionals. 9. Positive CultureI want to expand on workplace culture, team relationships, and the high-quality connections that flow from it. A major catalyst for much of the above is interprofessional education. A higher employee level of job resources may lead to increased job satisfaction and reduced burnout. Moreover, IPE could lead to more efficient use of resources in healthcare organizations.(9) Patients are better shielded against medical mistakes, which the system pays dearly for; with increased teamwork and communication, the number of medical errors drops. In addition, improved communication would further lead to better utilization of resources and prevent superfluous treatments or tests. Barriers to Implementation of IPE While there is a very positive effect of IPE on teamwork and communication, implementing the approach into the healthcare are not a simple endeavor. Nonetheless, there are a few things that can be difficult to handle with regards to time management. Get IPE Practice: Healthcare professionals have busy caseloads that may not provide time for IPE practices. Moreover, IPE typically involves collaboration between several healthcare organizations, which can pose a challenge to integrate in practice. Rottenness is just one of the complications. But there are also barriers to the implementation of IPE itself, such as the scarcity of time and reluctance to innovate.(10) Significance of Inter Professional Education IPE is a crucial success factor of collaborative working towards a common goal, that of a better patient outcome, while improving communication and collaboration among healthcare professionals. While there could be some limitations, the benefits indirectly obtained from IPE outweigh its disadvantages.
· There is need for still to define the best ways to assess IPE. The inconsistency in these existing patient-reported measures makes comparison and generalization of findings difficult across studies, and behaviour of several such tools differs in terms of reliability and validity.
· The majority of IPE work examines short-term outcomes with minimal to no follow up for the long-term impact. Yet, no research has focused on the sustained influence of IPE on interprofessional teamwork and communication behaviors.
· Most studies focus on a single or a handful of health professions, which is not representative of the complexity of interprofessional roles within practice.(5) However, research should focus on utilizing diverse and representative samples to effectively examine the impact of IPE on teamwork and collaboration components.
· 10 While the efforts towards IPE and teamwork and communication are frequently investigated in an experimental context, real-world aspects of those initiatives deviate substantially, and are underrepresented.
· Most studies assess how IPE affects healthcare workers without analyzing its effect on patient outcomes. More qualitative work exploring how IPE impacts patient satisfaction, quality of care and health outcomes would help fill the gap.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
Method
Liu, H. Y.,et,al. Clinical Collaboration: Topics in collaboration Clinical collaboration in a nursing context comes from having a good understanding of an Inter-professional nursing education promote collaboration in health providers for better patient outcome. We trust each other implicitly; it is the concept of swift trust. Collaboration is guided by interaction behaviors such as open communication and mutual respect. Darlow, B.,et,al. illustrated a longitudinal impact of interprofessional education on improving attitudes, skills, and career trajectories. These include a shared mindset of collaboration and patient-centeredness, better communication and teamwork skills, and new avenues for career advancement in medicine or other healthcare fields due to interprofessional collaboration. Best, S.,et,al. Professional identity in interprofessional teams Interprofessional teams are formed within patient’s specialities that are interdependent and must collaborate to achieve health goals. It is concluded that interprofessional collaboration and communication thus appear to be important factors shaping professional identity and enhancing team and patient outcomes through effective team work. Mink, J.,et,al. have addressed Interprofessional training wards are structured to improve the skills and competencies of healthcare professionals by allowing them to collaborate and learn from one another. Objectives: This quantitative longitudinal study seeks to measure the influence of such wards on interprofessional competencies over time. Bentley, M.,et,al. Interprofessional teamwork means collaboration and cooperation among health care professionals across disciplines to provide comprehensive primary health service care. This includes mutual respect, collaborative decision making and effective communication to deliver high-quality, patient-centered care. Mahmood, L. S.,et,al. . Time constraints are likely to limit the extent to which real-life communication challenges can be fully explored, and may not reflect the real-life complexities of interprofessional teamwork. Lam, P.,et,al. have discussed The healthcare professionals are key personnel to the success of anesthesia assistant care. Causes for the team’s interprofessional collaboration and its effect on patient management are to be identified through this study and the fellaism confirmed through the study can help in expanding the knowledge about anesthesia assistants amongst other health sectors. Burford, B.,et,al. A study conducted by McMurray et al. discussed that attitudes towards interprofessional learning among medical and nursing students enhanced through a single interprofessional simulation session, which also allowed them to improve their professional identity. Price, S. L.,et,al. Pre-entry perceptions of students entering five health professions have been addressed by Samuriwo, R.,et,al. The role that was once obscure to me is now clear . They have made their mark in a certain aspect/field (at least until October 2023).
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Liu, H. Y.,et,al. |
2020 |
Relies on voluntary participation, may not fully reflect team dynamics or address power imbalances. |
Improved collaboration and communication amongst healthcare professionals resulting in more efficient and effective patient care. |
|
Darlow, B.,et,al. |
2018 |
Increased sustainability of interprofessional collaboration and improved patient outcomes through long-term development of attitudes, skills, and career trajectories. |
One limitation is the potential for self-selection bias, as those who participate in interprofessional education may already have positive attitudes and skills. |
|
Best, S.,et,al. |
2019 |
By having a strong professional identity, team members can better understand and respect each other’s roles and make decisions together. |
One limitation could be difficulty in balancing individual professional identities with the team’s collective identity. |
|
Mink, J.,et,al. |
2021 |
An advantage of the study is that it provides quantitative data on the impact of an interprofessional training ward on interprofessional competencies over time. |
A possible limitation of this study is that it only focuses on the impact of an interprofessional training ward, without considering other factors that may influence interprofessional competencies. |
|
Bentley, M.,et,al. |
2018 |
Improved patient outcomes and quality of care due to the collaborative efforts and diverse expertise of a team of healthcare professionals. |
Limited resources can hinder the effectiveness of interprofessional teamwork in providing comprehensive primary healthcare services. |
|
Mahmood, L.S.,et,al. |
2021 |
Interprofessional simulation education is a method of teaching medical and nursing students effective teamwork and communication skills through simulated scenarios. It utilizes the TeamSTEPPS® framework, a evidence-based system that promotes team-based care and communication, to provide a hands-on, immersive training experience that enhances collaboration and patient safety. |
Collaboration and understanding of each other’s roles can improve patient outcomes and decrease medical errors during real-world practice. |
|
Lam, P.,et,al. |
2018 |
Identification of potential barriers and improvements for interprofessional collaboration in the anesthesia care team, ultimately improving patient outcomes. |
Limited generalizability of findings due to small sample size or specific population being studied. |
|
Burford, B.,et,al. |
2020 |
Improved attitudes toward interprofessional learning and professional identity, leading to better collaboration and patient care. |
“Limited generalizability to real-world settings due to short-term impact and isolated nature of the simulation session.” |
|
Price, S. L.,et,al. |
2021 |
Better understanding of the student’s initial perceptions can assist in developing tailored academic and career support systems for their chosen profession. |
Pre-entry perceptions may not accurately reflect the challenges and realities of the profession, leading to disillusionment and attrition rates among students. |
|
Samuriwo, R.,et,al. |
2020 |
Having a key role allows them to have a significant impact on the organization and its success. |
One limitation is that their key role is not widely recognized or acknowledged. |
DEVELOPMENT
We designed a model to explore the impact of interprofessional education on health care teamwork and communication designed with the following components in mind. To understand the broad scope of interprofessional education and how it impacts teamwork and communication skills for healthcare, it is advised to conduct a literature review as the first step. It is going to lay the groundwork for the investigation and it will give a theoretical foundation for ascertaining possible research questions and aims. Secondly, the model suggests obtaining practitioners qualitative impressions regarding interprofessional education through interviews or surveys across various disciplines in healthcare to understand how it has shaped their interprofessional collaboration and communication in practice. Interprofessional Education – Submit an abstract. Including hands-on experience, and what happens in clinical practice regarding these people and what they do on this topic. For a third way, the framework recommends conducting a study or observation of educational programs, or interventions that appear to foster interprofessional education within a healthcare environment. This will determine the most effective components and practices to strengthen collaboration and communication between healthcare providers. Figure 1 shows the Construction of proposed model.
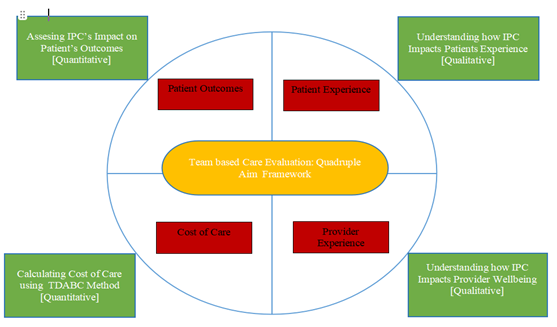
Figure 1. Construction of proposed model
Integrated Primary Care (IPC) is a patient-centered model of care that enhances patient outcomes and experience, while also tackling care costs and provider well-being. Indices like disease management, reduction in hospital readmissions, and overall improvement in health status can quantify this. Integrated primary care can integrate specialists and services into the primary care of patients, coordination, and management of care which can improve health outcomes. The second aim of IPC, together with patient outcomes, is to enhance the patient experience. Using a patient-centre approach, effective good IPC may even surpass patient satisfaction and stimulate patient engagement for more quality care and an improved patient experience. IPC integrates primary care with other primary care-focused services, allowing it to better manage the total cost of care. This can be accomplished by reducing efforts, removing redundancies and taking advantage of preventive care.
RESULTS AND DISCUSSION
Affecting teamwork and communication in healthcare, the theme of this study seeks to describe how interprofessional education (IPE), if properly implemented, can inspire members of the healthcare setting to work better and communicate better together. The study findings have shown that IPE has facilitated teamwork and communication of patients among nurses, physicians, and pharmacists as different health professionals. Example of Harding Fragment: IPE helps unite healthcare professionals with a shared understanding and communication skills. This knowledge enables the free flow of information between other bodies in order to serve the beginning and enhance the beginning of every healthcare professional. Furthermore, the study found that IPE contributes to breaking down the hierarchical boundaries separating health professionals as well as fostering a culture of trust and mutual respect. The effect is a more fluid, collaborative workplace, where people at every level are recognized for the unique skills and contributions they bring.
Interprofessional collaboration
Interprofessional education focuses on streamlining and enhancing communication, as well as teamwork, among healthcare professionals representing different disciplines.
|
Table 2. Comparison of Interprofessional Collaboration |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
IPE |
QE |
MA |
EMNS |
Proposed Model |
|
|
100 |
60,3 |
86,1 |
45,8 |
77,4 |
34,7 |
|
200 |
63,2 |
48,5 |
70,1 |
81,6 |
56,4 |
|
300 |
75,9 |
51,7 |
39,4 |
87,2 |
66,8 |
|
400 |
40,6 |
64,3 |
55,1 |
73,5 |
90,7 |
|
500 |
37,8 |
69,2 |
41,5 |
85,4 |
54,9 |
Ultimately, an indicator that can be used to evaluate the impact of this curricular integration in the education system is the degree of interprofessional collaboration in healthcare settings. Figure 2 shows the computation of Interprofessional Collaboration.
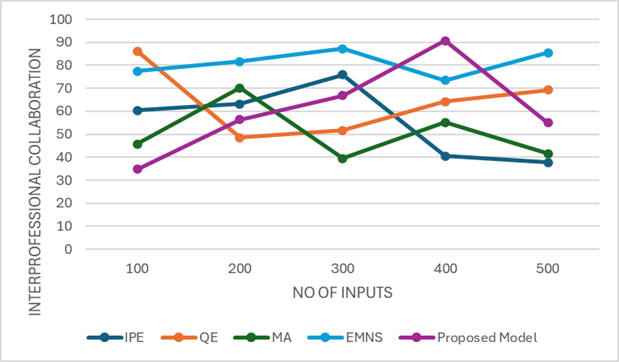
Figure 2. Computation of Interprofessional Collaboration
It can be measured by considering surveys, interviews, and watching team interactions.
Communication
Effective teamwork in healthcare relies heavily on communication, and interprofessional education aims to improve this aspect of professionals. Figure 3 shows the computation of Communication.
|
Table 3. Comparison of Interprofessional Collaboration |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
IPE |
QE |
MA |
EMNS |
Proposed Model |
|
|
100 |
67,3 |
43,2 |
80,9 |
60,5 |
49,1 |
|
200 |
35,4 |
84,7 |
58,3 |
64,9 |
71,8 |
|
300 |
40,2 |
78,5 |
54,6 |
61,7 |
85,1 |
|
400 |
42,8 |
69,6 |
50,3 |
76,1 |
38,9 |
|
500 |
88,3 |
65,7 |
47,5 |
79,2 |
55,8 |
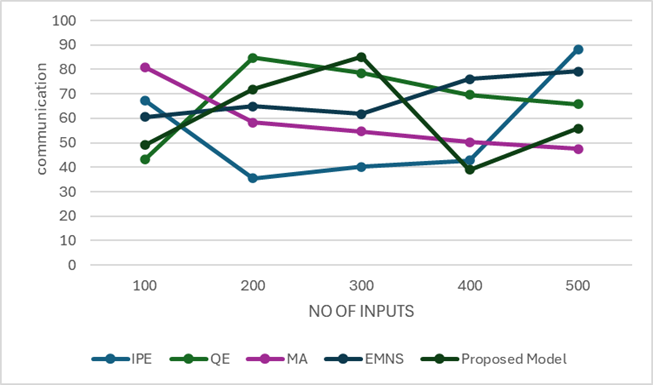
Figure 3. Computation of Communication
Communication between healthcare members can be evaluated through parameters including clarity, accuracy, timeliness, and mutual comprehension. That can be assessed through simulation scenarios and patient/team member feedback.
Patient outcomes
Our ultimate goal as an inter professional team is to improve patient outcomes through collaboration and communication.
|
Table 4. Comparison of Patient outcomes |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
IPE |
QE |
MA |
EMNS |
Proposed Model |
|
|
100 |
38,4 |
74,2 |
49,5 |
61,3 |
82,7 |
|
200 |
53,1 |
41,8 |
76,9 |
62,4 |
89,5 |
|
300 |
55,3 |
39,7 |
72,5 |
88,2 |
64,1 |
|
400 |
44,6 |
68,9 |
52,7 |
77,1 |
36,5 |
|
500 |
70,8 |
63,9 |
57,2 |
84,3 |
48,1 |
Hence, one of the critical performance parameters would be how this education translates into patient outcomes (e.g., recovery, quality of care, and patient satisfaction). Figure 4 shows the computation of Patient Outcomes.
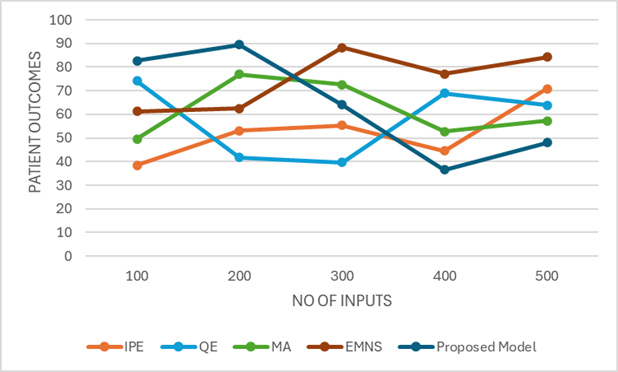
Figure 4. Computation of Patient Outcomes
Patient-reported surveys and analysis of clinical data can be used to assess this.
CONCLUSIONS
This review was undertaken to determine the impact of interprofessional education (IPE) on teamwork and communication in healthcare settings. Those studies found that IPE programs improved teamwork and communication skills and led to better collaboration and patient care. Prior studies show that teamwork and communication are key components in high-quality delivery of health-care services. Interprofessional education (IPE) programs also bring together students and health practitioners from multiple disciplines for trainingcentered on learning about each other, sharing multifaceted contributions, and preparing learners for future collaborative practice. Better they can work together the more of the health worker knows, their team, As they communicate with one another. Moreover, IPE enhances communication skills such as active listening, sharing of information and providing/receiving feedback. These are important skills to cultivate to work across disciplines effectively and ultimately reduce harm and improve care to patients.” In terms of its impact on health practitioners, some studies have also reflected the long-term effectiveness of IPP. Participants also reported improved confidence and the ability to use their enhanced teamwork and communication skills on the job. IPE was also found to promote an environment of collaborative learning in which health-care professionals can identify, and leverage, each other’s expertise across professions. This can be effectively accomplished only if enacted by and through the health care organizations as well as the educational institutions with the appropriate resources and time dedicated to these reforms.
· Establishing and practicing sound IPE programs that encourage sound communication and collaboration among healthcare providers.
· This study took a broad approach to understanding what IPE does but further work can take this understanding and target it closer to home on specific teams of healthcare workers, for example interprofessional teams with built environment facilitators in ICUs or rural healthcare teams. Such an approach will help better understand the impact of IPE on teamwork and communication in these environments.
· Further studies may examine how technology may be integrated into interprofessional experiences to promote interprofessional teamwork and communication (eg, online simulations, telehealth devices, and collaborative programs may facilitate communication and interaction of the members of the team).
BILBIOGRAPHIC REFERENCES
1. Liu, H. Y. (2020). Inter-professional nursing education and the roles of swift trust, interaction behaviors, and creativity: A cross-sectional questionnaire survey. Nurse Education Today, 95, 104598.
2. Darlow, B., Brown, M., Gallagher, P., Gray, L., McKinlay, E., Purdie, G., ... & Pullon, S. (2018). Longitudinal impact of interprofessional education on attitudes, skills and career trajectories: a protocol for a quasiexperimental study in New Zealand. BMJ open, 8(1), e018510.
3. Best, S., & Williams, S. (2019). Professional identity in interprofessional teams: findings from a scoping review. Journal of interprofessional care, 33(2), 170-181.
4. Mink, J., Mitzkat, A., Krug, K., Mihaljevic, A., Trierweiler-Hauke, B., Götsch, B., ... & Mahler, C. (2021). Impact of an interprofessional training ward on interprofessional competencies–a quantitative longitudinal study. Journal of interprofessional care, 35(5), 751-759.
5. Bentley, M., Freeman, T., Baum, F., & Javanparast, S. (2018). Interprofessional teamwork in comprehensive primary healthcare services: Findings from a mixed methods study. Journal of interprofessional care, 32(3), 274-283.
6. Mahmood, L. S., Mohammed, C. A., & Gilbert, J. H. (2021). Interprofessional simulation education to enhance teamwork and communication skills among medical and nursing undergraduates using the TeamSTEPPS® framework. medical journal armed forces india, 77, S42-S48.
7. Lam, P., Lopez Filici, A., Middleton, C., & McGillicuddy, P. (2018). Exploring healthcare professionals’ perceptions of the anesthesia assistant role and its impact on patients and interprofessional collaboration. Journal of Interprofessional Care, 32(1), 24-32.
8. Burford, B., Greig, P., Kelleher, M., Merriman, C., Platt, A., Richards, E., ... & Vance, G. (2020). Effects of a single interprofessional simulation session on medical and nursing students’ attitudes toward interprofessional learning and professional identity: a questionnaire study. BMC medical education, 20, 1-11.
9. Price, S. L., Sim, M., Little, V., Almost, J., Andrews, C., Davies, H., ... & LeBrun, J. (2021). Pre-entry perceptions of students entering five health professions: implications for interprofessional education and collaboration. Journal of Interprofessional Care, 35(1), 83-91.
10. Samuriwo, R., Laws, E., Webb, K., & Bullock, A. (2020). “I didn’t realise they had such a key role.” Impact of medical education curriculum change on medical student interactions with nurses: a qualitative exploratory study of student perceptions. Advances in Health Sciences Education, 25(1), 75-93.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: A Geetha Bhavani, Sujayaraj Samuel Jayakumar, Suvendu Narayan Mishra.
Methodology: A Geetha Bhavani, Sujayaraj Samuel Jayakumar, Suvendu Narayan Mishra.
Software: A Geetha Bhavani, Sujayaraj Samuel Jayakumar, Suvendu Narayan Mishra.
Drafting - original draft: A Geetha Bhavani, Sujayaraj Samuel Jayakumar, Suvendu Narayan Mishra.
Writing - proofreading and editing: A Geetha Bhavani, Sujayaraj Samuel Jayakumar, Suvendu Narayan Mishra.