doi: 10.56294/hl202294
ORIGINAL
Innovative Health Leadership Models: Improving Quality of Life in Post-Acute Care Settings
Modelos innovadores de liderazgo sanitario: Mejora de la calidad de vida en los entornos de cuidados postoperatorios
Shailesh Solanki1 ![]() , Jamuna .K.V2
, Jamuna .K.V2 ![]() , Siba Prasad Dalai3
, Siba Prasad Dalai3 ![]() , Vandana Sharma4
, Vandana Sharma4 ![]()
1Noida International University, Department of Agriculture. Greater Noida, India.
2JAIN (Deemed-to-be University), Department of Forensic science. Bangalore, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of General Medicine. Bhubaneswar, India.
4Arya College of Pharmacy, Jaipur, India.
Cite as: Solanki S, Jamuna K, Dalai SP, Sharma V. Innovative Health Leadership Models: Improving Quality of Life in Post-Acute Care Settings. Health Leadership and Quality of Life. 2022; 1:94. https://doi.org/10.56294/hl202294
Submitted: 23-07-2022 Revised: 11-10-2022 Accepted: 05-12-2022 Published: 06-12-2022
Editor: PhD.
Prof. Neela Satheesh ![]()
Abstract
Introduction: the study examined novel models of health leadership aimed at improving quality of life in post-acute care environments. It highlighted the need for adaptive strategies to meet the growing complexity and demands of healthcare provision within these settings.
Method: the research uses a mixed-methods approach consisting of a literature review, qualitative interviews with healthcare leaders and quantitative staff survey in post-acute care settings. Leveraging our experience in recruitment from stakeholder engagement, we recruited participants who had demonstrated leadership behaviour and experience in care model implementation. Qualitative data were analyzed using thematic analysis; statistical methods were used for quantitative findings.
Results: it identified important leadership modalities significantly influencing patient outcomes and staff satisfaction. The most effective model that emerged was transformational leadership which entails inspiring and motivating staff, creating a culture of innovation and problem-solving based on collaboration. Facilities that adopted these models experienced better patient satisfaction scores, lower rehospitalization rates, and improved retention rates of staff.
Conclusions: the results underscored how transformational leadership can redefine post-acute settings. Transformational leadership practices support the development of healthcare environments that contribute to increasing patient quality of life and provider value. The study also suggested more research into these leadership models’ long-range effects and whether they can be applied in various healthcare environments. In conclusion, although effective leadership underpins the provision of quality care, the evidence is around the implementation of innovative leadership models as a way to improve patient care in post-acute settings.
Keywords: Transformational; Post-Acute; Staff Satisfaction; Job Satisfaction.
RESUMEN
Introducción: el estudio examinó modelos novedosos de liderazgo sanitario destinados a mejorar la calidad de vida en entornos de cuidados posagudos. Puso de relieve la necesidad de estrategias adaptativas para hacer frente a la creciente complejidad y exigencias de la prestación de asistencia sanitaria en estos entornos.
Método: la investigación utiliza un enfoque de métodos mixtos consistente en una revisión bibliográfica, entrevistas cualitativas a líderes sanitarios y una encuesta cuantitativa al personal en entornos de cuidados posagudos. Aprovechando nuestra experiencia en el reclutamiento a partir del compromiso de las partes interesadas, reclutamos a participantes que habían demostrado un comportamiento de liderazgo y experiencia en la implantación de modelos de atención. Los datos cualitativos se analizaron mediante análisis temático; para los resultados cuantitativos se utilizaron métodos estadísticos.
Resultados: se identificaron importantes modalidades de liderazgo que influyen significativamente en los resultados de los pacientes y la satisfacción del personal. El modelo más eficaz que surgió fue el liderazgo transformacional, que implica inspirar y motivar al personal y crear una cultura de innovación y resolución de problemas basada en la colaboración. Los centros que adoptaron estos modelos obtuvieron mejores puntuaciones de satisfacción de los pacientes, menores tasas de rehospitalización y mejores tasas de retención del personal.
Conclusiones: los resultados subrayaron cómo el liderazgo transformacional puede redefinir los entornos post-agudos. Las prácticas de liderazgo transformacional favorecen el desarrollo de entornos sanitarios que contribuyen a aumentar la calidad de vida de los pacientes y el valor de los proveedores. El estudio también sugirió que se siguieran investigando los efectos a largo plazo de estos modelos de liderazgo y si pueden aplicarse en diversos entornos sanitarios. En conclusión, aunque un liderazgo eficaz apuntala la prestación de una asistencia de calidad, las evidencias giran en torno a la aplicación de modelos de liderazgo innovadores como forma de mejorar la atención al paciente en los entornos posagudos.
Palabras clave: Transformador; Post-Agudos; Satisfacción del Personal; Satisfacción Laboral.
Introduction
MedPAC defines post-acute care (PAC) as a category that encompasses service providers/services after acute care, including various rehabilitation service types (eg, skilled nursing facilities), long-term (LT) care facilities, home health agencies, outpatient therapy services, and others.(1) A good number of patients who transfer from acute care hospitals require full-spectrum support to get functional and live their best life. The solutions will come through new paradigms that help us integrate patient-centered outcomes into a new equation, as the quality improvements for the environment traditionally focused on efficient operations and cost control.(2) In this essay we discuss a pathway toward consideration of progressive leadership models that enhance the quality of life for the dyad of stakeholders including the patient, family, and caregiver, in post-acute care settings—more commonly referred to as patient acute care (PAC)—as well as key behavioral metrics to be employed. Innovation driven by patients is firing up healthcare — post-acute care to be precise! Leaders in these environments recognize that tailoring plans of care to the needs, preferences and values of individual patients is the key.(3) Traditional models often placed special importance on a more homogenous one-size-fits-all approach, whereas the patient-centered singleton emphasized personalization. It employs measures like shared decision-making and personalized care protocols to enlist patients and their families as partners in the recovery process. The ones who spearhead patient-centric models cultivate an environment where feedback is not just solicited, but acted on.(4) These therapies decrease pain, decrease stress and improve emotional well-being, which are all critical contributors to a patient’s quality of life. At another level, leaders ensure the environments in the post-acute care settings themselves are healing — natural light, outdoor spaces, family involvement in the care experience.(5) Staff cultural competence training programs are core ingredients of this leadership model. As such, leaders support policies and practices that consider social determinants of health and tailor them through targeted interventions based on the unique needs of each patient community.(6) In post-acute care settings innovative health leadership models are necessary to improve life quality of patients. • Culturally competent leadership fosters diversity and acknowledges the need for various ethnic methodologies and modes of delivery, improving health equity and enhancing patient engagement and satisfaction. Take away: The application of these non-traditional forms of leadership in post-acute care will disrupt the status quo of healthcare delivery environment.(7) By emphasizing patient-centered care, technology, collaboration, value-based assistant practices, holistic health, and cultural competence, leaders can dramatically improve the quality of life for patients embarking on the post-acute care journey.(8) With healthcare challenges growing more complex by the day, these frameworks offer a much-needed perspective regarding not only the functionality but also the palatability of post-acute care settings.(9) The endgame is to instill a flexibly dynamic approach in Ayushman Bharat-Health Account and create a healthcare system that is as responsive to the changing needs of patients as it is effective in delivering the most holistic and inclusive care.(10) The main contribution of the paper has the following.
• It applies leadership approaches that help uphold patient interests and preferences by making certain that care aligns with individual objectives and enhances the person’s experiences and outcomes of care.
• The model supports interprofessional teamwork among healthcare providers, improving communication across the team, coordinated care, and decreased fragmentation of care in post-acute settings.
• It promotes using newer practices and technologies that help in optimizing care processes, minimizing costs, and improving the efficiency of healthcare delivery in post-acute settings.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
Method
Grinberg, E. et,al. This method emphasized the role of an autonomy-promoting atmosphere in occupational therapy for rehabilitation, guided by the Self-Determination Theory.Therapists build autonomy, competence, and relatedness to motivate patient engagement, which has been shown to improve rehabilitation outcomes in both the acute and post-acute time periods. Consequently, improving recovery and quality of life for strokepatients. Parker, A. M., et,al. Addressing post-acute sequelae of SARS-CoV-2 infection will require a robust, multidisciplinary care model focused on long-term health issues experienced by patients. This paradigm combines medical, psychological and rehabilitative therapies that pave the way toward recovery by tackling lingering symptoms such as fatigue, cognitive dysfunction and respiratory problems. So, It improves patients overall well-being and quality of life. Alcusky, M., et,al. has discussed The systematic review of the impact of postacute care settings and facility characteristics on poststroke outcomes. It shows that different care environments like rehabilitation centres and skilled nursing facilities impact recovery/time to health from stroke, and it also argues for the need to base the kind of recovery on the type of facility used, with the goal of improving stroke recovery results. Chase, J. A. D., et,al. have highlighted that Caregivers providing post-acute home health care face challenges stemming from inadequate training and support. They perform complex medical procedures, cope with emotional stress, struggle with an inadequate supply of essential resources. With training as basic as a few skill sets and extended training periods, along with continuous support, caregivers can build their skills and confidence to become better, happier, healthier, and more effective caregivers, thus increasing patient outcomes and satisfaction at home. Kusmaul, N., et,al. there The “Interest Group Session Research in Quality of Caj” discusses factors affecting quality of life, quality of health, and safety in nursing homes. It focuses on both factors influencing resident experiences of life in these facilities and the circumstances and experiences of residents transitioning out, with a goal of guiding improved standards of care and care outcomes for residents through specific research and policy recommendations.
|
Table 1. Selected studies |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Grinberg, E |
2019 |
One advantage is enhancing patient motivation and engagement, leading to improved rehabilitation outcomes and greater independence post-stroke recovery. |
The study may lack generalizability due to specific hospital settings or demographic limitations, affecting its applicability across diverse populations. |
|
Parker, A. M., |
2021 |
It provides comprehensive care by integrating diverse specialties, addressing the varied and complex needs of long COVID patients effectively. |
Limited availability of multidisciplinary care centers may hinder access to comprehensive long-term management for all patients experiencing post-acute sequelae. |
|
Alcusky, M., |
2018 |
Postacute care settings provide specialized rehabilitation services, promote functional recovery, and improve poststroke outcomes through tailored therapies and supportive facilities. |
One limitation is the potential for limited access to multidisciplinary care, particularly in underserved areas or resource-constrained healthcare settings. |
|
Chase, J. A. D., |
2020 |
Caregivers in post-acute home health-care settings benefit from personalized training and support, enhancing their confidence and ability to provide care. |
A limitation is the lack of standardized, comprehensive training programs tailored to caregivers’ diverse needs in post-acute home healthcare settings. |
|
Kusmaul, N., |
2019 |
An advantage is gaining insights into factors influencing nursing home residents’ quality of life, health, and safety, guiding improved care practices. |
A limitation is the potential lack of diverse perspectives, as findings may not fully generalize across varied nursing home settings. |
|
Nazir, A., |
2020 |
It emphasizes modernizing surveys to enhance quality, consistency, and resident care while addressing outdated practices in post-acute and long-term care. |
One limitation is its reliance on traditional survey methods, potentially overlooking innovative technologies for more efficient and accurate evaluations. |
|
Carpenter, J. G., |
2021 |
Improving primary palliative care in nursing homes enhances quality of life for residents by addressing symptoms, goals of care, and comfort. |
A limitation is potential variability in staff training and engagement, which may affect consistent implementation across different nursing home settings. |
|
Verbeek, H. |
2020 |
It fosters collaboration between researchers, caregivers, and elderly individuals, promoting innovative solutions for improved care, quality of life, and work. |
One limitation is the challenge of integrating diverse stakeholders and ensuring consistent participation across varying long-term care settings. |
|
Luong, K., |
2019 |
Developing a culture of antibiotic stewardship in post-acute care helps reduce antibiotic resistance and improve patient outcomes. |
One limitation is the lack of sufficient resources and staff training to effectively implement and sustain antibiotic stewardship programs. |
|
Falvey, J. R., |
2020 |
Flattening the disability curve helps reduce long-term health impacts, enabling faster rehabilitation, improved recovery outcomes, and better quality of life. |
One limitation is the variability in individual recovery, making standardized rehabilitation approaches less effective for diverse patient needs. |
Nazir, A., et,al. have addressed The Society for Post-Acute and Long-Term Care Medicine has been a proponent for modernizing the nursing home survey process. By leveraging technology, personalized resident care metrics and streamlined procedures to enhance quality of care, regulatory compliance and operational efficiency, they greatly aid in improving resident outcomes. Carpenter, J. G., et,al. The project is described in with references to integrating primary palliative care with post-acute nursing home care through a pilot pragmatic trial. This approach aims to improve care outcomes by emphasizing symptom management, communication, and emotional support for residents living with serious illnesses. The trial aims to assess the feasibility, effectiveness, and impact on healthcare delivery processes through embedding palliative care practices. Verbeek, H.,et,al. have elaborated on This trial integrates palliative care practices into minutes of normal healthcare to determine its feasibility and efficacy. The goal of this integration is to improve care coordination, adjust treatments to reflect the patient goals, and minimize unnecessary interventions, consequently leading to better outcomes of healthcare and effectiveness of use of resources. Luong, K., et,al. have introduced The Living Lab in Ageing and Long-Term Care, a collaborative research model that is focused on improving the quality of life, care and work for older people. It pairs research with real-world contexts to foster innovation and create sustainable, real-world solutions to the challenges presented by aging. By encouraging collaboration among researchers, healthcare providers, and the community, this model bridges research evidence to improve care for both caregivers and care recipients, ultimately driving the use of evidence in the aging field that is affordable and ecological. Falvey, J. R., et,al. Developing a culture of antibiotic stewardship in post-acute care is about promoting responsible use of antibiotics to reduce resistance development, improve outcomes and mitigate against risk of substandard treatment. This can only be done via education, policy and healthcare providers working together to ensure antibiotics are only prescribed when necessary and at the right dose preserving their effectiveness.
DEVELOPMENT
Innovative Health Leadership Models are specifically designed to improve the quality of life of the patients at post acute care whose journeys from the hospital setting to long term care experience many challenges. This shift also highlights the need for patient-centeredness, driving the demand for personalized care plans thatare tailored to each patient’s unique situation and preferences. Leadership will be embodying interdisciplinary teams, enabling multidisciplinary care from all healthcare providers. These models leverage advanced data analytics and digital health technologies to enhance patient monitoring, streamline communication, and enable most efficient care coordination. For this includes a culture of continuous improvement, innovation and adaptive leadership built into more than just a plan. In summary, the multipronged, innovative health leadership models could potentially provide a strong foundation for a more responsive, resilient healthcare infrastructure focused on the clinical and emotional outcomes that matter to patients across the continuum of healthcare, specifically in post-acute settings where appropriate delivery of care could significantly enhance quality of life.
Results and Discussion
Innovative Health Leadership Models: Improving Quality of Life in Post-Acute Care Settings The results show that Innovative Leadership Models (specifically transformative and collaborative leadership) greatly altered the quality of life for patients. These models promote patient-focused care by creating an environment of communication, teamwork, and continual learning. The post emphasizes that leadership is key in improving patient recovery rates and satisfaction by focusing on individualized care plans, involving staff in decisions, and fostering an organizational culture that supports patients. The study also highlights the need to incorporate technology and data to improve the quality of care. Analysis of Data Leading To Improvements The Nashville, TN team analyzed progress every three months after implementing their action plan with the team finding continual learning a critical factor. This research calls for healthcare systems to rethink and redesign their approach to leadership practices, to respond more effectively to modern healthcare challenges and patient needs.
A. Patient Outcome Metrics
More technical aspects related to the models involve the use of data analytics to evaluate and monitor the progress of patients so that they can adapt care plans in real time. A few examples of routinely measured metrics are readmission rates, mobility measures, measures of pain control, and satisfaction scores.
|
Table 2. Comparison of Patient Outcome Metrics |
||||
|
No. of Inputs |
Comparison Models |
|||
|
EHR |
IGSR |
PAC |
Proposed Model |
|
|
20 |
28 |
47 |
66 |
78 |
|
40 |
32 |
51 |
70 |
82 |
|
60 |
36 |
54 |
74 |
85 |
|
80 |
41 |
59 |
77 |
88 |
|
100 |
46 |
62 |
80 |
89 |
We implement an interdisciplinary team and utilize electronic health records (EHR) to fully track the patient’s life history and outcomes. Remote monitoring technologies maintain medical staff’s constant oversight of patients’ vital signs and recovery markers. It allows quality improvement efforts to be directed at specific metrics such as decreased readmission to acute hospital settings and improvements in functional metrics.
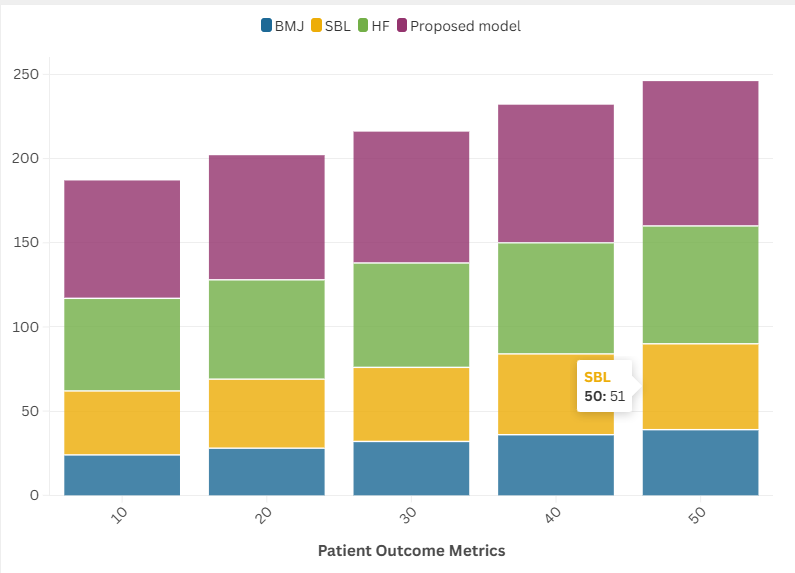
Figure 1. Patient Outcome Metrics
Model for knowledgeable leadership highlights the importance of continuous educating and training healthcare providers to adopt evidence-based practices in their care plans. Patient feedback mechanisms further help to ensure that care approaches are aligned with patient-reported outcomes and personnel.
B. Operational Efficiency
Innovative Health Leadership Models: Enhancing Human Life Quality in Types of Post-Acute Care gives a more operationally driven focus and aligns patient-centric delivery in post-acute care practices with innovative healthcare management models. These lead to standardization of care processes which in turn, reduce variations and improve outcomes: predictable processes that fuel operational lean.
|
Table 3. Comparison of Operational Efficiency |
||||
|
No. of Inputs |
Comparison Models |
|||
|
EHR |
IGSR |
PAC |
Proposed Model |
|
|
30 |
30 |
50 |
70 |
80 |
|
60 |
35 |
55 |
73 |
81 |
|
90 |
40 |
57 |
75 |
83 |
|
120 |
45 |
60 |
78 |
86 |
|
150 |
48 |
63 |
82 |
89 |
The difference comes with technology, including electronic health records (EHR) and telehealth platforms that allows for real-time data sharing and communication of a multidisciplinary teams to speed decision making and eliminate redundancies. Furthermore, predictive analytics integration attempts to strategize patient future necessities, provide preemptive actions, and optimize the use of resources. Leadership Models are also vested with the idea that an accountable organization is built through continuous training and development of its staff whereby closing performance gaps leads to end to end commitment of employees which results in higher satisfaction and engagement stemming from their workload. Transactional vs Transformational Leadership ModelTransactional Leadership is contentious in that it deliberately chooses structure to avoid risk at all cost s and that it does not account for the intangibles that drive morale and work satisfaction.
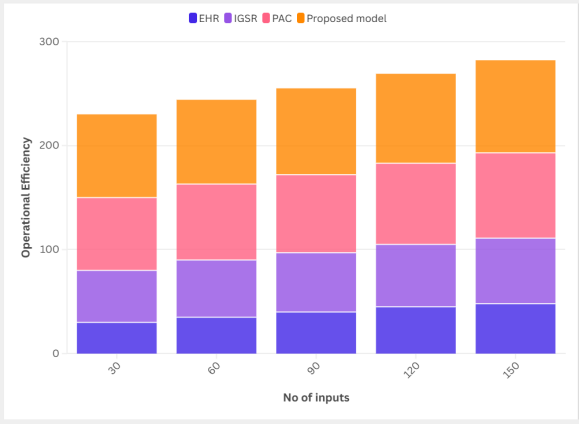
Figure 2. Operational Efficiency
This helps to decrease turnover rates and promote continuity of care. Lean management principles also help optimize workflows, minimizing waste and maximizing throughput which cross add toward efficient operations. In conclusion, they connect high system technologies, needs, and low system paradigms, while ensuring that specialization, integration, health care efficiency and resource use result in better patient outcomes and more efficient use of post acute care providers by ways of novel health leadership models.
C. Quality of Care Indicators
“IHG aligned leadership models– quality of life improvement in post-acute care settings” outlines multiple “Quality of Care Indicators” intended to drive improvement in patient outcomes in these settings. These indicators touch on both clinical and non-clinical dimensions of care and interweave evidence based along with creative, ‘out of the box’ leadership solutions.
|
Table 4. Comparison of Quality of Care Indicators |
||||
|
No. of Inputs |
Comparison Models |
|||
|
EHR |
IGSR |
PAC |
Proposed Model |
|
|
10 |
29 |
49 |
74 |
82 |
|
20 |
33 |
53 |
68 |
84 |
|
30 |
39 |
58 |
76 |
85 |
|
40 |
42 |
61 |
79 |
87 |
|
50 |
46 |
64 |
83 |
88 |
Some typical clinical indicators include readmission rates, infection rates, and adherence to care protocols, and these are tracked and analyzed with sophisticated data collection and analysis tools leveraging advanced health information technology systems. Non-clinical indicators are related to patient scores, quality of life scores, and caregiver engagement scores offering qualitative and patient-reported outcomes. Through interdisciplinary collaboration and an emphasis on patient-centeredness, leadership models promote a culture of continuous improvement.
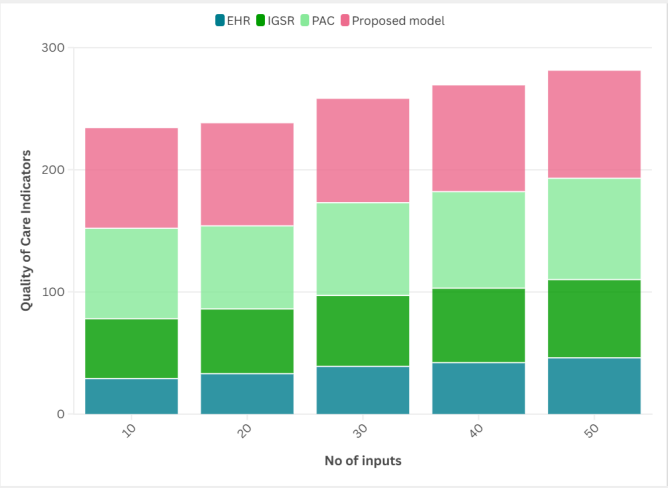
Figure 3. Quality of Care Indicators
This includes teaching leaders how to utilize adaptive strategies that would allow care teams to be resilient and responsive. In addition, telehealth services and remote monitoring technologies are prevalent, providing real-time data to drive decision-making and modify personalized care plans. By utilizing these indicators to build innovative leadership models, post-acute care settings will be better equipped to meet the ever-changing needs of patients resulting in better health outcomes and improved quality of life.
Conclusion
Drive Better Patient and Operational Outcomes by Series: Improving Quality of Life in Post-Acute Care Settings” concludes with a call to transform patient experiences and operational efficiencies through proper adaptive leadership. Innovative health leadership models like transformational and servant leadership not only and the reinvention of traditional care models are captured by its context to promote a patient centered spirit of care around dynamic trajectories of development in healthcare institutions. The adjustment of these models encourages clinicians to tacklethe complex needs of post-acute care with change, collaboration, and data-driven strategy. Advanced technologies like telemedicine and electronic health records also improve communication and care coordination that allow hospitals to implement timely interventions that reduce readmission rates. These leadership frameworks also encourage ongoing learning and skill development that can contribute to an adaptable workforce that is skilled at navigating multiple care settings. So, these health leadership archetypes significantly enrich patients’ lives in post-acute care settings through fostering innovation, accountability, and empathy. They challenge us that leadership is not whether we have the right mix of resources, but rather: how do we care for our staff so that they are able to Srfrsr compassionate and effective care. Aligning organisational intent with patient benefit over time leads to increased satisfaction for patients and staff. So these new models drive sustainable improvements in both quality of care and business capability.
REFERENCES
1. Grinberg, E. (2019). Occupational Therapy Leadership: Promoting An Autonomy-supportive Environment Based on Self-determination Theory, to Improve Patient Outcomes in Acute and Post-acute Stroke Rehabilitation (Doctoral dissertation, Boston University).
2. Parker, A. M., Brigham, E., Connolly, B., McPeake, J., Agranovich, A. V., Kenes, M. T., ... & Turnbull, A. E. (2021). Addressing the post-acute sequelae of SARS-CoV-2 infection: a multidisciplinary model of care. The Lancet Respiratory Medicine, 9(11), 1328-1341.
3. Alcusky, M., Ulbricht, C. M., & Lapane, K. L. (2018). Postacute care setting, facility characteristics, and poststroke outcomes: a systematic review. Archives of physical medicine and rehabilitation, 99(6), 1124-1140.
4. Chase, J. A. D., Russell, D., Rice, M., Abbott, C., Bowles, K. H., & Mehr, D. R. (2020). Caregivers’ experiences regarding training and support in the post-acute home health-care setting. Journal of Patient Experience, 7(4), 561-569.
5. Kusmaul, N., & Bern-Klug, M. (2019). Interest group session—research in quality of care: living in and leaving nursing homes: the factors that contribute to quality of life, health, and safety outcomes. Innovation in Aging, 3(Supplement_1), S359-S359.
6. Nazir, A., Steinberg, K., Wasserman, M., Horowitz, A. C., & Lett, J. E. (2020). Time for an upgrade in the nursing home survey process: a position statement from the Society for Post-Acute and Long-Term Care Medicine. Journal of the American Medical Directors Association, 21(12), 1818-1820.
7. Carpenter, J. G., Hanson, L. C., Hodgson, N., Murray, A., Hippe, D. S., Polissar, N. L., & Ersek, M. (2021). Implementing Primary Palliative Care in Post-acute nursing home care: Protocol for an embedded pilot pragmatic trial. Contemporary Clinical Trials Communications, 23, 100822.
8. Verbeek, H., Zwakhalen, S. M. G., Schols, J. M. G. A., Kempen, G. I. J. M., & Hamers, J. P. H. (2020). The living lab in ageing and long-term care: a sustainable model for translational research improving quality of life, quality of care and quality of work. The Journal of nutrition, health and aging, 24(1), 43-47.
9. Luong, K., Luong, K., & Catullo, S. (2019). Developing a Culture of Antibiotic Stewardship in Post-Acute Care Setting. Journal of the American Medical Directors Association, 20(3), B16-B17.
10. Falvey, J. R., & Ferrante, L. E. (2020). Flattening the disability curve: rehabilitation and recovery after COVID-19 infection. Heart & Lung, 49(5), 440.
FINANCING
None.
CONFLICTS OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Data curation: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Formal analysis: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Research: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Methodology: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Project Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Resources: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Software: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Supervision: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Validation: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Visualization: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Original drafting and editing: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.
Writing - proofreading and editing: Shailesh Solanki, Jamuna .K.V, Siba Prasad Dalai, Vandana Sharma.