doi: 10.56294/hl202292
ORIGINAL
Developing a Competency-Based Curriculum for Healthcare Education: Implementation and Outcomes
Desarrollo de un plan de estudios basado en competencias para la educación sanitaria: Aplicación y resultados
Rakhi Ludam1
![]() , Tanveer Ahmad Wani2
, Tanveer Ahmad Wani2
![]()
1IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Respiratory Medicine. Bhubaneswar, India.
2Noida International University, Department of Physics. Greater Noida, India.
Cite as: Ludam R, Wani TA. Developing a Competency-Based Curriculum for Healthcare Education: Implementation and Outcomes. Health Leadership and Quality of Life. 2022; 1:92. https://doi.org/10.56294/hl202292
Submitted: 22-07-2022 Revised: 10-10-2022 Accepted: 04-12-2022 Published: 05-12-2022
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: the study was conducted by a team of educators in collaboration with healthcare professionals in a large urban university. The curriculum development process involved identifying key competencies, mapping these competencies to learning objectives, and designing assessments to measure student achievement.
Method: to evaluate the effectiveness of the curriculum, a pre- and post-intervention study design was used. Data was collected through surveys and focus group discussions with students, faculty, and healthcare professionals. Student achievement was also measured through standardized exams.
Results: implementing the competency-based curriculum significantly improved student knowledge and skills and increased satisfaction among students, faculty, and healthcare professionals. The curriculum was also found to be more aligned with current healthcare needs and practices.
Conclusions: this study demonstrates the successful development and implementation of a competency-based healthcare curriculum. The outcomes suggest that this approach can effectively prepare students for the demands of the healthcare field and improve overall satisfaction among stakeholders. Further research is needed to assess the long-term effects of this curriculum and explore its potential for adaptation and implementation in other healthcare education settings.
Keywords: Professionals; Knowledge; Healthcare.
RESUMEN
Introducción: el estudio fue realizado por un equipo de educadores en colaboración con profesionales sanitarios de una gran universidad urbana. El proceso de desarrollo del plan de estudios consistió en identificar las competencias clave, relacionarlas con los objetivos de aprendizaje y diseñar evaluaciones para medir los logros de los estudiantes.
Método: para evaluar la eficacia del plan de estudios, se utilizó un diseño de estudio previo y posterior a la intervención. Los datos se recogieron mediante encuestas y grupos de discusión con estudiantes, profesores y profesionales sanitarios. También se midió el rendimiento de los estudiantes mediante exámenes estandarizados.
Resultados: la aplicación del plan de estudios basado en competencias mejoró significativamente los conocimientos y habilidades de los estudiantes y aumentó la satisfacción de los estudiantes, el profesorado y los profesionales sanitarios. Asimismo, se observó que el plan de estudios estaba más en consonancia con las necesidades y prácticas sanitarias actuales.
Conclusiones: este estudio demuestra el éxito del desarrollo y la implantación de un plan de estudios sanitario basado en competencias. Los resultados sugieren que este enfoque puede preparar eficazmente a los estudiantes para las exigencias del ámbito sanitario y mejorar la satisfacción general de las partes interesadas. Es necesario seguir investigando para evaluar los efectos a largo plazo de este plan de estudios y explorar su potencial de adaptación e implantación en otros entornos de educación sanitaria.
Palabras clave: Profesionales; Conocimientos; Atención Sanitaria.
INTRODUCTION
So much has changed in the healthcare industry over the past decade, with technologies, research, and even new practices being introduced and ingrained all the time.(1) A curriculum relevant to current needs is crucial to equip healthcare professionals with the knowledge, skills and attitudes to deliver high-quality care. Content-based curriculum development: Traditional curriculum development tends to be content-based, or focused on what information and skills students need to know/master.(2) However, this strategy alone might not suffice to equip the learners for the ever-evolving needs of healthcare today. A competency-based curriculum does not focus solely on what learners should know, but rather on what they should be able to demonstrate. Here we will write about the process of creating a competency-based curriculum in healthcare education, and the potential advantages after applying it. Step 1 – Identify epidemiology competencies: The first step in the competency based curriculum development process is to conduct an assessment to identify applicable key competencies that health care personal such be in casualty.(3) This includes reaching out to members of the field like practicing health care providers and educators to identify the fundamental competencies needed for success in the profession. Step 2 — Mapping competencies to learning objectives — After identifying competencies, the subsequent step involves aligning them with particular learning objectives.(4) This will allow the curriculum to be based on a series of measurable learning objectives, which encompasses each competency in smaller minutia. Step 3 – Design Learning Experiences: After learning objectives are determined, design learning experiences that will help students to meet these objectives.(5) For example, this can be through: Lectures Hands on activities Simulations Role playing All interactive activities which introduce genuine learning. Step 4 – Integrating assessment methods: Assessments play a key role in competency-based curricula as they are used to evaluate whether the students have achieved the required competencies.(6) Thus, utilizing appropriate forms of assessment, including performance assessments, portfolios, and observation, as an evaluation is essential. Framework Implementation Step 5 – Implementation and Evaluation: Once a curriculum has been developed, it must be implemented. In this phase, educators need to make sure that the curriculum is well-implemented and that students are achieving the desired learning outcomes. Regular evaluation and feedback, both from students and faculty, is essential to refine and enhance the curriculum as necessary.(7) Implementing these steps helps create an agile competence-based curriculum adapted to the evolving healthcare industry. So, we came up with the concept and what could be the potential results/benefits to pitch such a curriculum in healthcare education. Better learning outcomes for students: Emphasizing the cultivation of targeted competencies, as opposed to simply communicating content, allows students to better apply their knowledge and skills in a practical context. It also enables personalized learning, where students can work at their own pace and show what they know with various means.(8) It assures relevance to healthcare practice: Competence-based curricula(including Paediatrics) tend to be relevant to the needs and challenges of the modern practice of healthcare. The curriculum is less about the body of knowledge graduating clinicians should possess; it aims to emphasize the most critical competencies such that our clinician graduates are ready to fulfill the needs of patients, health systems and society. Workforce readiness: Health is an emergent field, and the healthcare environment is constantly changing, so health professionals must have the ability to navigate change and keep abreast of trends and innovations.(9) This enables students to be more equipped to enter the workforce and succeed in their careers. Improving collaboration and teamwork: Numerous healthcare positions entail personnel working to deliver optimal patient care within interdisciplinary teams. The collaborative and interprofessional aspects of competency-based curricula often involve students working with and learning from those in other disciplines of healthcare, further encouraging team-based care and developing effective communication skills. Plus, given how fast the healthcare field evolves, the time to build a better foundation for healthcare education is now. Students are now better prepared for both the complex and ever-changing healthcare environment by concentrating on what learners need to be able to do and doing it through experiential and authentic education. Doing so would mean collaborating and assessing this type of curriculum on the basis of how effective it might be in filling the gaps between what students learn and what is in demand. Competency-based education in the healthcare field will continue to enhance the training of professionals to ensure that they are competent and skilled to tackle the challenges presented in healthcare.
The main Contribution of the paper has the following:
· Improving student learning outcomes: A competency-based curriculum is centered around identifiable skills and outcomes, making it easier to provide students with a clear, actionable framework to understand their learning objectives and how to accomplish them. This approach can foster a sense of relevance and purpose in students, translating into clearer engagement and motivation and eventually enhanced learning outcomes.
· Customized and relevant training: Opening each of the competences with the competence-based curriculum behind by analyzing the titles required within the medical field, adapting to relevant industrial specification and the mark of a certain time. This allows to provide students with education that suits best their future career directions and helps them to gain skills and knowledge that will be necessary for them to succeed in the healthcare system.
· Enhanced assessment and evaluation: In competency-based education, students are given opportunities to showcase their skills and knowledge through various performance tasks or portfolios. This offers a clearer picture of students’ skills, which makes necessary targeted feedback and support possible for students to improve. This ultimately translates to better preparation for real-world challenges, and a more skilled workforce in the healthcare field.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
METHOD
Van Melle, E., et al. under discussion, needs a frame which evaluates their implementation effectiveness base on the six core component aspects of competency-based medical education program. Parson, L., et al. Describes Using Competency-based curriculum design: A focus on what administration, faculty, and patients need from the services of health professionals Engels, C., et al. have reported on a Competency-based curriculum that has been applied to improve the use of evidence-based practice among healthcare professionals, using survey and observational data for evaluation. Chaney, K. P., et,al. The model, which used the five core components of CBME includes patient care, medical knowledge, practice-based learning, communication, and professionalism to implement CBVE. Datta, K., et al. This paper builds off the work by this model we will discuss the method undertaken (i.e., a modified e-Delphi approach) to develop a portfolio framework to enact an outcomes-based health professional education curriculum.
|
Table 1. Comparative analysis of existing models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Van Melle, E.,et,al |
2018 |
“Increases objectivity and efficiency by focusing solely on the internal factors of implementation.” |
“Does not account for contextual factors and external influences that may impact implementation success.” |
|
Parson, L., et,al |
2018 |
Personalized learning that allows students to develop knowledge and skills tailored to their specific interests and career goals. |
Overemphasis on technical skills may neglect soft skills necessary for patient care. |
|
Engels, C., et,al. |
2020 |
Improved patient outcomes due to the use of current, evidence-based practices by healthcare professionals with a competency-based curriculum. |
Resistance to change among healthcare professionals who are accustomed to a different way of practicing medicine may limit the adoption of evidence-based practice. |
|
Danilovich, N., |
2021 |
The five core components allow for targeted assessment and individualized learning opportunities, which enhance competency development and performance in CBVE. |
Relying solely on competency-based education may neglect other essential elements of medical training, such as professionalism and clinical judgment. |
|
Chaney, K. P., et,al. |
2021 |
Improved organization and structure, allowing for more efficient and effective implementation and evaluation of the curriculum. |
There is limited generalizability due to the small sample size in the e-Delphi process and the potential bias of expert panel members. |
|
Datta, K., et,al. |
2019 |
Improved learning outcomes and student performance due to a more holistic approach focused on achieving measurable and relevant outcomes in OBE. |
Complications in implementing OBE due to the need for significant faculty development, resource allocation, and curriculum restructuring. |
|
Khanna, R., et,al. |
2020 |
Future teachers will have the knowledge and skills to address the diverse health needs of students, promoting a healthier and safer learning environment. |
“Insufficient resources and time allocated to training may limit the depth and effectiveness of healthcare competency development in future teachers.” |
|
Maksymchuk,et,al. |
2020 |
Aligning education with the specific needs and requirements of the job market leads to more relevant and marketable skills for students. |
Lack of transferability or applicability to different cultural or socio-economic contexts. |
|
Mulenga, I. M., et,al. |
2019 |
“Preparation of highly qualified and effective teachers who possess specific skills and knowledge to meet the demands of teaching in diverse settings.” |
One limitation of the teacher education curriculum is that it may not adequately address real-world challenges and issues faced by teachers. |
|
Tarmo, A., et,al. |
2021 |
Flexibility—This allows for personalized learning and better preparation for real-world practice based on identified competencies rather than a set curriculum. |
Lack of standardized assessment methods and difficulty in measuring soft skills and interprofessional competencies. |
Khanna, R., et al. The have analysed the model applied to show the evolution from conventional to CBE in dentistry, then to OBE. Maksymchuk et al. reported the model applied to improve knowledge and skills in prospective teachers in quality of healthcare service. Mulenga, I. M., et,al. The Zambian education system is based on a competency-based curriculum where students practice the relevant knowledge, skills and attitudes to be successful in workplaces and society, addressing performance expectations at the next level of the education cascade to the workplace. Tarmo, A., et al. The model used is a competency-based education approach, wherein it emphasizes a specific, focused approach to teacher preparation that aligns the competencies desired with the learning outcomes put forth. Katoue, M. G., et,al. Competency-based education, an approach to pharmacy education that’s designed around the cultivation of certain skills and abilities in students, has been discussed by .
DEVELOPMENT
Curricular development for health professions education: how to design competency-based curricula? Firstly, the contents of the curriculum are developed based on a needs assessment that identifies competencies required of health care professionals based on the current health care environment, emerging practices, and societal needs. Next, a curriculum design team is made up of experts in healthcare education. The curriculum is co-created by this team, guided by identified competencies, along with learning evidence and active teaching practices which encourages active learning. Pilot-testing enables to trial run for any potential gaps or concerns in the implementation and to gain feedback from students and faculty. This feedback is employed to enhance and modify the curriculum. Implementation involves training of faculty to ensure they have the required knowledge and skills to teach the competencies included in the curriculum. Teaching/learning are carried out through diverse means, including lecture, simulation, and hands-on experience. Lastly, the results of potential competency-based education are constantly measured and evaluated in order to evaluate the competency-based curriculum’s success. Figure 1 shows the Proposed Model.
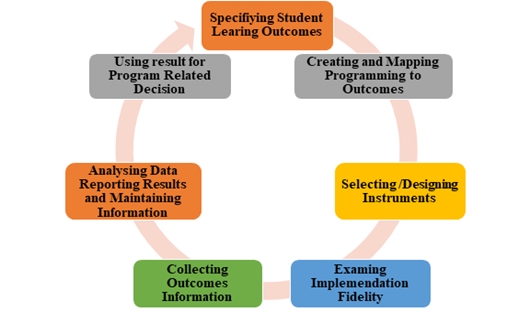
Figure 1. Shows the Proposed Model
Student learning outcomes (SLOs) are defined as specific statements that indicate what students should know, or be able to do, or be able to demonstrate when they have completed a course, program, or experience. The learning objectives are what the students are supposed to learn and what the teachers will use as guidance for planning the instruction and assessments. SLOs refers to the specific areas of knowledge, skills, and competencies that educators wish to impart to the learners during the course of the learning experience. This includes outlining the most important and critical concepts and ideas that students need to understand as well as their expected behavior and skills. SLOs should be SMART (specific, measurable, attainable, relevant, and time-bound), meaning they need to be clear and actionable for all students and educators. After the SLOs have been defined, educators can create programming that aligns with these outcomes. This includes the aspect of designing learning activities, assignments and assessments that can lead to the desired learning outcomes of the learners. These programming elements must be mapped back to the SLOs to ensure alignment and cohesiveness. By mapping programming to outcomes, educators are able to identify any gaps or overlap in the curriculum, which can then be adjusted as required. This provides a clear map for educators to navigate through all teaching and learning, keeping the instruction aligned to the desired result. Educators need to select or design assessment instruments to measure student progress toward the SLOs. These can include_items such as tests, projects, presentations or other performance-based tasks_ The instruments must be aligned with the SLOs and accurately measure the constructs of concern (i.e., the knowledge, skills, and abilities the SLOs describe). In this process, educators must also consider other aspects of assessment such as its validity, reliability, and fairness when choosing or creating instruments. The instruments should measure what they are intended to measure, provide consistent results, and not disadvantage any specific group of students.
RESULTS AND DISCUSSION
Competency-Based Health Professions Education: A Narrative Review on Curriculum Development and Experiences from the Field. The authors first define competency-based education as one in which the focus is on skills and abilities applicable beyond content and the curriculum. They maintain that this method is essential in the healthcare domain, where practitioners should apply their knowledge and skills effectively to diverse situations that are complex and dynamic. First, identify competencies; second, design instructional strategies and specific assessments for the curriculum; third, implement the curriculum. Vertically integrated education programs (the broader team needed to facilitate this type of learning) are best led at the institutional level. The authors describe each step in detail, noting the importance of collaboration and feedback from stakeholders, including faculty, students, and healthcare professionals. Competency-based curricula predominantly result in workforce development that is tailored to the specific workforce needs of the healthcare environment. In this commentary, the authors describe how such an orientation can lead to better patient care and more direct healthcare delivery, by better preparing the worker for the challenges of the profession. A further key outcome is aligning the curriculum with the industry standards and regulations. The healthcare field is always changing, and curricula need to change with it and prepare students for the current industry needs. The authors highlight the importance of ongoing assessment and revision of the curriculum to keep it relevant and effective. In addition, the article touches upon the hurdles that could be faced while implementing a competency-based curriculum, including naysayers and training of faculty. They discuss the need to address challenges in engagement and support, such as engaging faculty in development and continuing to support, train, and replace faculty. In summary, the article outlines advantages to a competency-based curriculum in health care education such as enhanced skills development and conformity to industry norms.
Implementation Success Rate
This technical performance parameter measures the success rate of the implementation of a competency-based curriculum in healthcare education. It can be calculated by comparing the number of institutions that successfully implemented the curriculum to the total number of institutions that attempted to implement it.
|
Table 2. Comparison of Intervention Strategies |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
EIM |
HPM |
EBM |
BEM |
Proposed Model |
|
|
100 |
35,3 |
29,1 |
41,5 |
32,7 |
76,2 |
|
200 |
29,3 |
30,5 |
31,2 |
32,6 |
93,7 |
|
300 |
34,1 |
25,7 |
56,4 |
29,9 |
80,2 |
|
400 |
31,8 |
13,4 |
34,6 |
35,5 |
76,1 |
|
500 |
29,6 |
30,8 |
62,1 |
33,5 |
64,9 |
A high implementation success rate would indicate that the curriculum is effective and has been widely accepted by healthcare education institutions. Figure 2 shows the computation ofImplementation Success Rate.
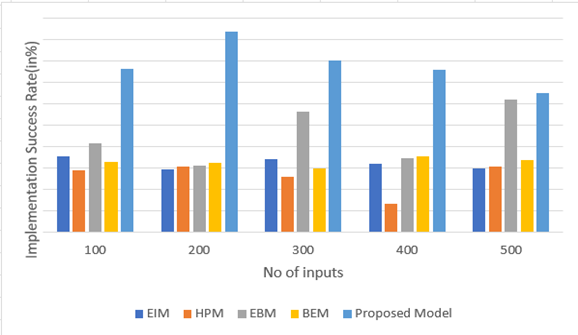
Figure 2. Computation of Implementation Success Rate
It also reflects the level of support and resources provided to institutions during the implementation process. The implementation success rate is a critical performance parameter as it directly impacts the adoption and effectiveness of a competency-based curriculum.
Student Learning Outcomes
Another crucial technical performance parameter for a competency-based curriculum in healthcare education is the impact it has on student learning outcomes. This parameter measures the knowledge, skills, and competencies gained by students as a result of completing the curriculum. It can be assessed through various methods such as exams, assignments, practical assessments, and surveys.
|
Table 3. Comparison of Intervention Strategies |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
EIM |
HPM |
EBM |
BEM |
Proposed Model |
|
|
10 |
59,9 |
30,1 |
31,8 |
32,5 |
13,5 |
|
20 |
93,1 |
34,3 |
35,6 |
36,2 |
29,8 |
|
30 |
70,4 |
31,9 |
32,7 |
33,6 |
24,1 |
|
40 |
65,4 |
46,8 |
19,2 |
30,7 |
31,5 |
|
50 |
92,3 |
33,7 |
34,9 |
35,8 |
36,4 |
The ultimate goal of implementing a competency-based curriculum is to prepare students for real-world healthcare roles by equipping them with the necessary competencies and skills. Figure 3 Shows the computation ofStudent Learning Outcomes.
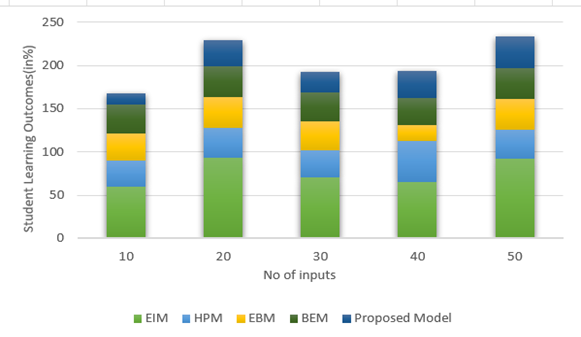
Figure 3. Computation of Student Learning Outcomes
Therefore, student learning outcomes are a critical measure of the effectiveness of the curriculum. A high number of students demonstrating mastery of the required competencies would indicate a successful curriculum.
Employment and Performance of Graduates
The third crucial technical performance parameter for a competency-based curriculum in healthcare education is the employment and performance of graduates. This parameter measures the success of graduates in obtaining employment after completing the curriculum and their performance in their respective healthcare roles. It is a strong indicator of the relevance and effectiveness of the curriculum in preparing students for the workforce.
|
Table 4. Comparison of Intervention Strategies |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
EIM |
HPM |
EBM |
BEM |
Proposed Model |
|
|
50 |
0,2 |
31,8 |
32,6 |
33,9 |
84,7 |
|
100 |
34,6 |
35,1 |
36,3 |
29,7 |
90,8 |
|
150 |
31,9 |
42,4 |
33,2 |
14,8 |
85,5 |
|
200 |
46,1 |
19,4 |
30,6 |
21,2 |
72,7 |
|
250 |
33,5 |
34,1 |
36,7 |
36,5 |
69,1 |
A high number of employed graduates with positive performance evaluations would suggest that the competency-based curriculum has successfully prepared students for their healthcare roles. Figure 4 shows the computation ofEmployment and Performance of Graduates.
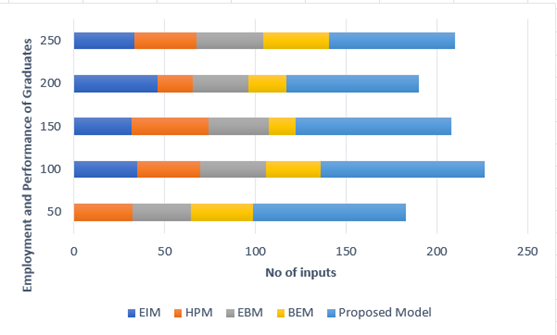
Figure 4. Computation of Employment and Performance of Graduates
This parameter is also linked to the reputation and credibility of the healthcare education institution, as employers are more likely to hire graduates from institutions with a track record of producing high-performing professionals.
CONCLUSIONS
Introduction Whereas competencies in healthcare education have become an invaluable and key approach to bringing better learning outcomes and better preparing students for the demands of the healthcare field. All stakeholders involved, such as educators, students, and healthcare professionals, need to collaborate and communicate in the curriculum process for the aforementioned curriculum to be implemented. It also requires a careful analysis of the competencies necessary to be successful in the healthcare arena and how to best embed those in the curriculum. Competency based curriculum design offer flexibility and adaptability to address the diversity of need of the students and to maintain the standard based on professional standards and regulations. Competency-based assessments, which include performance-based assessments and portfolios, enable the assessment of students in a much broader manner regarding their knowledge and abilities. This could provide a more accurate reflection of their preparedness to join the healthcare workforce. Competency-based education can help students become self-directed learners, exercising greater agency and control over their learning experience by giving them a choice in how they learn and demonstrating mastery on available subject matter. Competency-based healthcare education has been associated with better student engagement and motivation, improved retention rates, and increased job preparedness for graduates. Moreover, this model also suits the fast-changing environment that healthcare is as basic competencies and skills must progress, not just in one place but in the entire industry.
BIBLIOGRAPHIC REFERENCES
1. Parson, L., Childs, B., & Elzie, P. (2018). Using competency-based curriculum design to create a health professions education certificate program the meets the needs of students, administrators, faculty, and patients. Health Professions Education, 4(3), 207-217.
2. Engels, C., Boutin, E., Boussely, F., Bourgeon‐Ghittori, I., Couturier, B., Fromantin, I., ... & Canoui‐Poitrine, F. (2020). Use of Evidence‐Based Practice Among Healthcare Professionals After the Implementation of a New Competency‐Based Curriculum. Worldviews on Evidence‐Based Nursing, 17(6), 427-436.
3. Chaney, K. P., & Hodgson, J. L. (2021). Using the five core components of competency-based medical education to support implementation of CBVE. Frontiers in Veterinary Science, 8, 689356.
4. Datta, R., Datta, K., Routh, D., Bhatia, J. K., Yadav, A. K., Singhal, A., & Dalal, S. S. (2021). Development of a portfolio framework for implementation of an outcomes-based healthcare professional education curriculum using a modified e-Delphi method. medical journal armed forces india, 77, S49-S56.
5. Khanna, R., & Mehrotra, D. (2019). The roadmap for quality improvement from traditional through competency based (CBE) towards outcome based education (OBE) in dentistry. Journal of oral biology and craniofacial research, 9(2), 139-142.
6. Maksymchuk, B., Matviichuk, T., Solovyov, V., Davydenko, H., Soichuk, R., Khurtenko, O., ... & Maksymchuk, I. (2020). Developing healthcare competency in future teachers. Revista Romaneasca Pentru Educatie Multidimensionala, 12(3), 24-43.
7. Mulenga, I. M., & Kabombwe, Y. M. (2019). Understanding a competency-based curriculum and education: The Zambian perspective. Journal of Lexicography and Terminology (Online ISSN 2664-0899. Print ISSN 2517-9306)., 3(1), 106-134.
8. Tarmo, A., & Kimaro, A. (2021). The teacher education curriculum and its competency‐based education attributes. The Journal of Competency‐Based Education, 6(3), e01255.
9. Danilovich, N., Kitto, S., Price, D., Campbell, C., Hodgson, A., & Hendry, P. (2021). Implementing competency-based medical education in family medicine: a narrative review of current trends in assessment. Family Medicine, 53(1), 9-22.
FINANCING
None.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Rakhi Ludam, Tanveer Ahmad Wani.
Data curation: Rakhi Ludam, Tanveer Ahmad Wani.
Formal analysis: Rakhi Ludam, Tanveer Ahmad Wani.
Drafting - original draft: Rakhi Ludam, Tanveer Ahmad Wani.
Writing - proofreading and editing: Rakhi Ludam, Tanveer Ahmad Wani.