doi: 10.56294/hl2024.404
ORIGINAL
Challenges and Resilience: Leadership, PQOL and Moral Distress Amidst The COVID-19 Crisis
Desafíos y resiliencia: Liderazgo, PQOL y angustia moral en medio de la crisis de COVID-19
Manashree Mane1
![]() , Swati Kemothi2
, Swati Kemothi2 ![]() , Vijay Jagdish Upadhye3
, Vijay Jagdish Upadhye3
![]() , Debasmita Rath4
, Debasmita Rath4 ![]() , Anubhav Bhalla5
, Anubhav Bhalla5 ![]() , Sidhant Das6
, Sidhant Das6 ![]() , A.R. Shinde7
, A.R. Shinde7 ![]()
1JAIN (Deemed-to-be University), Department of Forensic science. Bangalore, Karnataka, India.
2School of Allied Health Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
3Parul Institute of Applied Sciences (PIAS), Parul University, Dept of Microbiology. Vadodara, Gujarat, India.
4IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Paediatrics. Bhubaneswar, Odisha, India.
5Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
6Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
7Krishna Institute of Medical Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”, Dept. of Pharmacology. Taluka-Karad, Dist-Satara, Maharashtra, India.
Cite as: Mane M, Kemothi S, Jagdish Upadhye V, Rath D, Bhalla A, Das S, et al. Challenges and Resilience: Leadership, PQOL, and Moral Distress Amidst The COVID-19 Crisis. Health Leadership and Quality of Life. 2024; 3:.404. https://doi.org/10.56294/hl2024.404
Submitted: 14-03-2024 Revised: 02-08-2024 Accepted: 10-11-2024 Published: 11-11-2024
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
To appreciate how the professional demands brought on by the corona virus disease - 2019 (COVID-19) pandemic impacted nurses and other healthcare workers’ morale and general quality of life (QOL), and how it influenced their capacity to serve patients. For healthcare professionals who are providing patient care, this pandemic presents the prospect of a poor work-life balance and heightened Moral Distress (MD). Research that was semi-structured with outpatient healthcare professionals (HCP) was conducted using a converging multidisciplinary design with snowball sampling techniques. As a consequence of the apparent lack of support from decision-making leadership, the availability of personal protective equipment (PPE), and the frequently shifting legislation, healthcare professionals (HCPN) reported an increase in moral agony and a decrease in their professional quality of life (PQOL). By implementing shared governance, training in crisis management, and increased communication, executive leadership may be able to prevent a decrease in PQOL and an increase in MD among front-line HCPNs.
Keywords: Moral Distress (MD); Professional Quality of Life (PQOL); Leadership Nurses; Health Care Providers (HCP).
RESUMEN
Apreciar cómo las exigencias profesionales provocadas por la pandemia de la enfermedad por el virus de la corona - 2019 (COVID-19) repercutieron en la moral y la calidad de vida (CV) general de las enfermeras y otros profesionales sanitarios, y cómo influyeron en su capacidad para atender a los pacientes. Para los profesionales sanitarios que prestan cuidados a los pacientes, esta pandemia presenta la perspectiva de un mal equilibrio entre la vida laboral y personal y un mayor Malestar Moral (DM). Se llevó a cabo una investigación semiestructurada con profesionales sanitarios ambulatorios (HCP) utilizando un diseño multidisciplinar convergente con técnicas de muestreo de bola de nieve. Como consecuencia de la aparente falta de apoyo del liderazgo en la toma de decisiones, la disponibilidad de equipos de protección individual (EPI) y la legislación frecuentemente cambiante, los profesionales sanitarios (HCPN) informaron de un aumento de la agonía moral y una disminución de su calidad de vida profesional (PQOL). Mediante la implantación de una gobernanza compartida, la formación en gestión de crisis y el aumento de la comunicación, el liderazgo ejecutivo puede ser capaz de prevenir una disminución de la PQOL y un aumento de la DM entre los HCPN de primera línea.
Palabras clave: Malestar Moral (DM); Calidad de Vida Profesional (CVP); Liderazgo Enfermeras; Proveedores de Atención Sanitaria (PS).
INTRODUCTION
Professionals in social work often encounter difficult emotional circumstances in addition to organizational challenges.(1) Nurses were providing a level of care for emergencies while juggling their responsibility to look out for patients with their responsibility to safeguard itself and their families. The moral suffering felt by nurses through the pandemic and its link to kind for patients who had COVID-19 and lacked personal protective equipment (PPE) has not received much attention.(2) Several types of research have shown that moral distress has a detrimental impact on the healthcare institution, the healthcare professionals, and the patient. The well-being of medical personnel, the standard of treatment, and the ability to meet institutional goals are three key areas where moral distress has an impact.(3) Hospitals have increased their ability to offer intense care, but staff in intensive care units (ICUs) has had a lot of difficulty caring for very sick patients. In the past, nurses had to deal with personal dangers such as weariness, burnout, and moral discomfort even when there wasn't a crisis.(4) It emphasized the moral pain have gone through as a result of the Covid-19 epidemic and stressed the need of distinguishing between individual burnout and moral harm brought on by systemic hardship.(5) Compassion satisfaction (CS) and burnout (BO) are two good and negative aspects of PQOL.(6) Some of COVID-19's most devastating effects on people who were infected fell on the healthcare industry. They were close to hospital patients on the front lines. Frontline health professionals were under a lot of stress from the outset of the epidemic due to the enormous demand for their services.(7) It showed the COVID-19 of PQOL and moral distress challenges, Crisis leadership, and resiliency.(8)
To described the PQOL and how people feel about their work as caregivers.(9) The research examines previous and recent evidence on the mode of transmission of respiratory transmissible viruses in relation to SARS-CoV-2, the current PPE recommendations in Korea in comparison to those of the WHO and other organisations, and the standard requirements and proper selection of PPE for respiratory and body protection.(10) To demonstrated that social workers faced significant workplace changes that led to secondary traumatic stress while also increasing their sense of compassion. However, the availability of social support mitigated these effects to keep secondary traumatic stress at a minimum.(11) The Research sought to delve deeply into the perspectives of healthcare workers during the COVID-19 crisis.(12) The research aimed to acquire a better understanding of the obstacles that healthcare providers faced while caring for adult patients during the COVID-19 epidemic.(13) Used a cross-sectional design and mixed-methods survey methodology to establish odds ratios for factors impacting PQOL.(14) Since there was a dearth of literature on this subject in India, a survey was conducted online to gauge healthcare provided by.(15) COVID-19 cases were on the rise in Taiwan, and with more hospital workers came more mental health issues, so researchers looked at the link between QOL at work, stress levels, and overall well-being.(16) Identified emotional labour and job stress that was seen during administrative work and how they impact the PQOL of Public Health Nurses (PHN) depending on the employment type. The PQOL Questionnaire was intended to be culturally adjusted for Greece in this research.(17) To determined that a curriculum based on the compassionate mind model lessens students' perceived aversions to compassion and enhances their professional well-being.(18) To addressed moral distress and other pertinent concerns, including how it impacts the PQOL of the ICU treatment staff. A survey of the consultant membership of the Faculty of Intensive Care Medicine was conducted using the PQOL (Pro-QOL) survey technique.(19) Evaluated the frequency of compassion fatigue among occupational therapists have shown that empathy is essential for preventing secondary trauma, preventing burnout, and improving compassion satisfaction.(20) The research aimed to examine healthcare workers' perspectives and experiences with COVID-19 and care delivery methods used in the UK.(21)
METHOD
A convergent mixed-methods approach is employed to gather the two types of qualitative information at the same time. A mixed-methods approach was used better understand the effect of professional obligations on the moral suffering of HCPs providing patient care during the COVID-19 epidemic. Several analyses of both qualitative and quantitative data were merged to provide a single set of conclusions.
Participant Details
During the COVID-19 pandemic, data on 180 HCPs were collected. This information includes demographic, ProQOL, MMD-HP, and COVID-19 practice-related data. The majority of participants were married women who were bedside nurses in acute care settings. Participants' workweeks ranged from 20 to 45 hours on average, and they had been in practice for 21 + years on average. The majority of the participants (69 %) were registered nurses. The average education level of those who took part was a bachelors. 18 % percent of the HCPs in our sample had to make a transition from one specialty to another, such as moving from the cardiovascular critical care facility to the COVID-19 unit. Table 1 gives the participants demographic details.
|
Table 1. Healthcare Participants' Job and sociodemographic factors |
|
|
Sample Quality |
N (%) |
|
Age |
|
|
18-25 |
15 (8,3) |
|
26-30 |
35 (19,4) |
|
31-40 |
50(27,8) |
|
41-50 |
45(25,0) |
|
51+ |
35(19,5) |
|
Children |
|
|
None |
70 (38,9) |
|
One |
40 (22,2) |
|
Two |
38 (21,1) |
|
Three or more |
32 (17,8) |
|
Professional Role |
|
|
imaging technician/ laboratory/ Patient care/ |
13 (7,2) |
|
Another nursing role |
32 (17,8) |
|
Bedside nurse |
115(63,9) |
|
Physician |
5 (2,8) |
|
occupational therapist/ Physical therapy |
15 (8,3) |
|
Years in Practice |
|
|
3-5 Yeas |
30 (16,7) |
|
11-20 years |
43(23,9) |
|
6-10 years |
40(22,2) |
|
Less than 2 Years |
22(12,2) |
|
21+ years |
45 (25,0) |
Enrolment and Sample Size
Convenience and snowball sampling as well as a recruitment method aided by information technology were used to find participants for an online survey. This survey was carried out remotely using Zoom and Research Electronic Data Capture (REDCap) because of constraints that were in effect during COVID-19. Participants who met the criteria below were regarded as eligible: During the corona virus pandemic, they met the following criteria:
· They were HCPs giving treatment to patients in an inpatient or outpatient environment.
· They were English-literate.
· They had internet access.
180 of the 182 individuals who accepted to participate finished the online questionnaires. Interested individuals were invited to take part in a Zoom interview to learn more about how HCPs handled patients during the COVID-19 pandemic. Table 2 provide the semi-structured interview questionnaire.
|
Table 2. Questions for a semi-structured interview |
|
|
S.No |
Semi-structured interview questions |
|
1 |
Have they contemplated giving up nursing as a result of your work with COVID-19 patients? |
|
2 |
What beneficial effects if any have or will this epidemic have? |
|
3 |
How has their day-to-day life altered since the epidemic started? |
|
4 |
How would characterize your present health? |
|
5 |
How is their household doing at the moment? |
|
6 |
How did their job typically operate before COVID-19? |
|
7 |
Tell me about your emotions when you learned you will be providing care for COVID+ patients. |
|
8 |
How do they normally deal with pressure? |
|
9 |
How have they been managing the pressure that comes with caring for COVID + patients—specifically, how have you been managing unpleasant circumstances, contamination risk, working in demanding settings, and how have you been managing people's responses to you when you return home? Please provide instances. |
|
10 |
If they have any worries concerning your safety, let me know. |
|
11 |
What was their personal PPE experience? |
|
12 |
Tell me about the kind of help you have access to or have had at their workplace. |
|
13 |
What knowledge, instruction, or training did they and their medical peers get before dealing with COVID-19 patients? |
|
14 |
What, if any, ways have the COVID-19 outbreak changed the way patients are handled at your hospital? |
|
15 |
How have their interactions with their patients changed as a result of COVID-19? |
|
16 |
What impact has taking care of COVID-19 patients had on your family life? |
|
17 |
Which time has been the most difficult? |
|
18 |
What effect did the media's coverage of the epidemic have on? |
|
19 |
What will the situation entail once corporations and states begin pre-COVID actions, in your opinion? |
|
20 |
In what ways has your company facilitated their life so far? |
|
21 |
How have modifications to COVID-19-related rules and procedures affected the capacity to provide patient care? |
Quantitative Data
The ProQOL is utilized to assess the PQOL of HCPs. Compassion satisfaction (CS) and Compassion fatigue (CF) estimate the secondary trauma (ST) and burnout, are evaluated in this 30-item self-report survey. The exam's 6-point Likert scale has subscale scores from 0 to 6, and the total score range is between 10 and 50. This scale has been used to weigh the advantages and disadvantages of helping persons who are afflicted or traumatized.
Qualitative Data
The semi-structured, open-ended questions used in the interviews were approved by HCPs who were providing care for patients who were either suspected of having COVID-19 during the pandemic or who had been diagnosed with it. The interview was conducted in a confidential workplace and videotaped. This interviewer used two to three probes to make sure the subject understood each question and to encourage more research into their experience. The analytical techniques listed below were used to analyse each set of data individually. During data interpretation, findings from the two data sets were compared for convergence or divergence to assist researchers in comprehending the primary objective of the study.
Data Analysis
Quantitative data analysis was done using SPSS Version 26. The data were cleaned using the MMD-HP cut-offs for low, average, and high values the scores from the response sample were then divided into three categories. Statistical methods such as descriptive statistics were utilized to explain the demographic, individual, and specialized information of the individuals, as well as their QOL and moral distress about their employment.
RESULTS
Quantitative
Professional Life Quality: the ProQOL scale was completed by 152 of the 180 participants (table 3). A strong correlation was found between the respondents' evaluations and all three measures of ProQOL. Burnout and PTSD symptoms went down, but participants reported more happiness from showing kindness after receiving assurances from higher-ups.
|
Table 3. The COVID-19 Pandemic's Effects on the PLOQ and MD of HCP |
||
|
Measurement |
Mean (SD) |
Range |
|
Professional quality of life subscales |
|
|
|
Secondary traumatic stress (STS) |
15,50+6,90 |
(10–42) |
|
Compassion Satisfaction (CS) |
28,30+6,9 |
(8–52) |
|
Burnout (BO) |
24,90+6,05 |
(3–36) |
|
The measure of Moral Distress-Healthcare Professionals (MMD-HCP) |
119,98+73,05 |
(1-434) |
Before COVID-19, HCPs who provided direct patient care had significantly lower mean ratings for compassion satisfaction and tiredness than those who did not provide direct patient care. According to U = 1964,5, p =0,031, HCPs who changed their practice environment had a significantly higher mean rank of compassion satisfaction. However, HCPs who altered their practice environment had a significantly lower mean rank of BO than those who did not (U = 1149,5, p =0,003) (table 4). HCPs who put in extra time had a considerably higher mean rank of STS than those who did not (see figure 1), in comparison to those who did it.
|
Table 4. Strong kindred between contextual variables and work-related happiness dimensions |
|||
|
|
U value |
P value |
Mean rank |
|
Compassion satisfaction (CS): professional quality of life (PQoL) |
|||
|
No group (n = 68) |
|
|
61,90 |
|
Yes group (n = 84) |
|
|
85,70 |
|
Before and during COVID-19, did you do bedside nursing duties? |
1742,0 |
0,018* |
|
|
No group (n = 43) |
|
|
88,02 |
|
Yes group (n = 109) |
|
|
70,63 |
|
Did your practice area change during COVID-19? |
1964,5 |
0,031* |
|
|
No group (n = 125) |
|
|
72,40 |
|
Yes group (n = 25) |
|
|
91,50 |
|
Health Care Provider Moral Distress Index |
|
|
|
|
Did you do any acute care work during COVID-19? |
1479,0 |
0,003* |
|
|
No group (N = 23) |
|
|
41,79 |
|
Yes group (N = 94) |
|
|
63,21 |
|
Did you put in extra time during COVID-19? |
3383,6 |
0,001** |
|
|
No group (N = 68) |
|
|
66,65 |
|
Yes group (N = 82) |
|
|
82,83 |
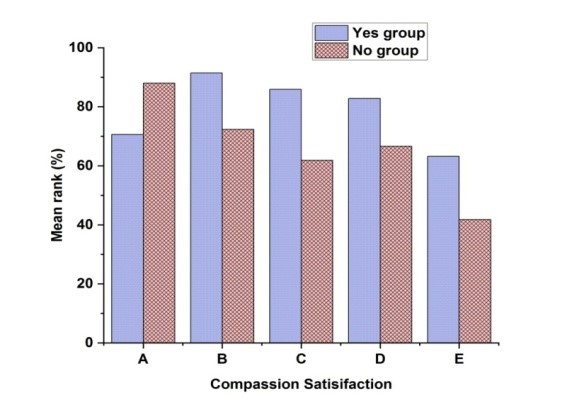
Figure 1. Medical staff morale during the COVID-19 epidemic as measured by their moral distress
Figure 1 displays the morale of the medical professionals during the COVID-19 outbreak as shown by their moral anguish. A indicates the work as a bedside nurse during COVID. The COVID-19 epidemic may be difficult and stressful, but also immensely necessary and satisfying, to work as a bedside nurse. Prevention of infection strategies is crucial during the pandemic. They must rigorously stick to the rules and procedures established by healthcare institution, including donning PPE, washing hands properly, and taking isolation precautions. During COVID-19, B denotes the change in the practice area. The distinction between professional and private lives may have dissolved as remote service has become increasingly common. Separating the surroundings of work and home may be difficult for many individuals, which can cause an imbalance. It's essential to establish clear boundaries, designate a distinct workspace, and adhere to a routine to foster a healthy work-life balance. As indicated by the letter C, fresh PPE is provided for each shift that takes place during COVID. To preserve people's safety and welfare, personal protective equipment (PPE) regulations were altered in response to the COVID-19 epidemic. It's critical to remember that PPE requirements might vary according to local regulations, restrictions unique to certain industries, and our expanding understanding of the virus. D denotes that more work was done for COVID-19. Many individuals found themselves working longer hours often throughout the COVID-19 pandemic. The epidemic's many challenges and workplace modifications sometimes demanded extra time and effort. E indicates the work in the field of critical care During COVID-19. Healthcare personnel have found it tough and stressful to work in the area of critical care during COVID-19. To reduce the danger of infection, HCP is required to follow stringent guidelines for the use of PPE. Wearing masks, gloves, gowns, and face shields or goggles is part of this. To maintain safety, proper donning and doffing procedures are essential. Relationship status and bed count as a metric of the practice size. At a p-value of 0,001, substantial relationships between the ProQOL subscales were discovered. Burnout and compassion satisfaction had a negative link (r =0,492), but secondary traumatic stress and burnout were positively connected (table 5).
|
Table 5. The moral struggle of the medical professionals during the COVID-19 the epidemic |
||||
|
Variables |
MMD-HP |
CS |
BO |
STS |
|
MMD-HP |
1 |
-0,463** |
0,550** |
0,330** |
|
CS |
-0,463** |
1 |
-0,492** |
-0,290** |
|
BO |
0,550** |
-0,492** |
1 |
0,630** |
|
STS |
0,335** |
-0,290** |
0,630** |
1 |
Qualitative
23 people were interviewed using semi-structured methods. Among HCPs, nurses with less than 10 years of practice dominated. Most healthcare providers have at least a bachelor's degree. Three main themes related to the crash of this pandemic on professionals' morale and QOL were identified through a thematic analysis of qualitative data from 23 healthcare professionals. Topics included structural defects and leadership difficulties and their management, as well as resilience and collaboration.
Between moral responsibility and Fright: HCPs faced significant challenges, maintaining their dedication to patients while enduring emotional strain. Many in this generation may carry permanent emotional scars. Despite concerns for their own health and the risk of contracting the virus, HCPs continued to prioritize patient care. Nurse expressed concerns about following safety protocols, ensuring proper use of PPE, and protecting family members. Nonetheless, HCPs felt a strong obligation to support their colleagues and remain on the front lines. Nurse stayed committed to her work out of a sense of duty, while a patient care technician, felt "called" to help during the pandemic. For those working in emergencies, such as EMTs and paramedics, responding to crises became both a responsibility and a privilege.
Despite setbacks caused by management and the system, they persisted in their work: healthcare providers faced on going frustration due to constantly changing information from management, leading to a lack of trust. Nurse expressed feelings of confusion, wondering what exactly was expected of them. The inconsistent use and distribution of PPE increased both the emotional burden and cost of patient care. Providers felt vulnerable, especially when top executives failed to respond adequately. Expressed deep frustration when non-clinical management criticized the use of protective gear, claiming it scared patients, yet offered no practical alternatives. Some participants also noted that the "lead" label placed on HCPs during the pandemic added further pressure. Nurse commented that the "lead" narrative felt hollow, adding to the emotional toll on those working on the front lines. Despite these challenges, healthcare workers continued to fulfil their duties with resilience.
Collaboration and resilience-building as priorities building resilience: participants reported feeling a stronger sense of teamwork and enhanced communication regarding patients and treatment options during the pandemic. Nurse noted that the crisis revealed a more humanizing aspect of their colleagues, seeing them beyond just professionals. Nurses, in particular, highlighted improved collaboration among the entire healthcare team, including doctors, nurses, and auxiliary staff. One nurse shared how the pandemic felt like a shared battle, bringing everyone closer and making them a more cohesive unit. The added responsibility often fell on nurses to manage patient care and emotions, especially when other staffs was unable or hesitant to enter patient rooms, further strengthening their role as the primary link between patients and the rest of the healthcare team. Despite these increased pressures, the experience fostered greater unity and collective problem-solving within teams.
CONCLUSIONS
The unique features of the COVID-19 outbreak have had devastating effects on the healthcare system and HCPs. The purpose of this mixed-methods research was to inquire into how HCPs' professional experiences kind for patients during this epidemic affected their moral distress and QOL in the workplace. The study's results suggest that HCPs were unqualified for the difficulties of providing patient care during the epidemic. The absence of support from top leadership, together with anxiety about the ease of use of clean PPE at the start of each shift, had a significant impact on professionals' QOL on the job and their sense of moral turbulence. Married or cohabiting HCPs reported higher degrees of moral unease and lower professional QOL. Employees who worked longer shifts worked more hours, or moved from a pleasant preparation environment to a COVID-19 unit showed similar correlations between a decrease in professional QOL and an increase in moral suffering. Made every effort to include a varied sample of HCPs, yet the majority of our participants were nurses. Therefore, another study should be conducted to properly examine other HCPs' experiences. The previously available information and resources have changed as a result of the COVID-19 outbreak. Data were gathered early in the epidemic before a vaccine was available when the majority peoples were suffering their initial COVID-19 cases and adhering to lockdown and social isolation.
BIBLIOGRAPHIC REFERENCES
1. Keener TA, Hall K, Wang K, Hulsey T, Piamjariyakul U. Relationship of quality of life, resilience, and associated factors among nursing faculty during COVID-19. Nurse Educator. 2021 Jan 1;46(1):17-22.
2. Lake ET, Narva AM, Holland S, Smith JG, Cramer E, Rosenbaum KE, French R, Clark RR, Rogowski JA. Hospital nurses' moral distress and mental health during COVID‐19. Journal of advanced nursing. 2022 Mar;78(3):799-809.https://doi.org/10.1111%2Fjan.15013
3. Atli Özbaş A, Kovancı MS. The experience of moral distress by chief nurse officers during the COVID‐19 pandemic: A descriptive phenomenological study. Journal of Nursing Management. 2022 Oct;30(7):2383-93.
4. Trachtenberg S, Tehan T, Shostak S, Snydeman C, Lewis M, Romain F, Cadge W, McAuley ME, Matthews C, Lux L, Kacmarek R. Experiences of moral distress in a COVID‐19 intensive care unit: A qualitative study of nurses and respiratory therapists in the United States. Nursing inquiry. 2023 Jan;30(1):e12500.
5. Xue Y, Lopes J, Ritchie K, D’Alessandro AM, Banfield L, McCabe RE, Heber A, Lanius RA, McKinnon MC. Potential circumstances associated with moral injury and moral distress in healthcare workers and public safety personnel across the globe during COVID-19: a scoping review. Frontiers in Psychiatry. 2022 Jun 13;13:863232.
6. Mehedi N, Ismail Hossain M. Experiences of the frontline healthcare professionals amid the COVID-19 health hazard: a phenomenological investigation. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2022 Jul;59:00469580221111925.
7. Moon M, Seo K. Effect of anxiety and calling on professional quality of life in COVID-19 dedicated nurses in Korea. InHealthcare 2022 Sep 18 (Vol. 10, No. 9, p. 1797). MDPI.
8. Farber J, Payton C, Dorney P, Colancecco E. Work-life balance and professional quality of life among nurse faculty during the COVID-19 pandemic. Journal of Professional Nursing. 2023 May 1;46:92-101.
9. Kreh A, Brancaleoni R, Magalini SC, Chieffo DP, Flad B, Ellebrecht N, Juen B. Ethical and psychosocial considerations for hospital personnel in the Covid-19 crisis: Moral injury and resilience. PloS one. 2021 Apr 2;16(4):e0249609.
10. Park SH. Personal protective equipment for healthcare workers during the COVID-19 pandemic. Infection & chemotherapy. 2020 Jun;52(2):165.
11. Buselli R, Corsi M, Veltri A, Baldanzi S, Chiumiento M, Del Lupo E, Marino R, Necciari G, Caldi F, Foddis R, Guglielmi G. Mental health of Health Care Workers (HCWs): a review of organizational interventions put in place by local institutions to cope with new psychosocial challenges resulting from COVID-19. Psychiatry research. 2021 May 1;299:113847.
12. Ardebili ME, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H. Healthcare providers experience of working during the COVID-19 pandemic: A qualitative study. American journal of infection control. 2021 May 1;49(5):547-54.
13. Ness MM, Saylor J, Di Fusco LA, Evans K. Healthcare providers' challenges during the coronavirus disease (COVID‐19) pandemic: A qualitative approach. Nursing & health sciences. 2021 Jun;23(2):389-97.
14. Min Fui W, Abdul Majid H, Ismail R, Su TT, Maw Pin T, Said MA. Psychosocial factors associated with mental health and quality of life during the COVID-19 pandemic among low-income urban dwellers in Peninsular Malaysia. Plos one. 2022 Aug 23;17(8):e0264886.
15. Wald HS. Optimizing resilience and wellbeing for healthcare professions trainees and healthcare professionals during public health crises–Practical tips for an ‘integrative resilience’approach. Medical Teacher. 2020 Jul 2;42(7):744-55.
16. Kalani Z, Barkhordari-Sharifabad M, Chehelmard N. Correlation between moral distress and clinical competence in COVID-19 ICU nurses. BMC nursing. 2023 Apr 7;22(1):107.
17. Lapum J, Nguyen M, Fredericks S, Lai S, McShane J. “Goodbye… through a glass door”: emotional experiences of working in COVID-19 acute care hospital environments. Canadian Journal of Nursing Research. 2021 Mar;53(1):5-15.
18. Karnatovskaia LV, Johnson MM, Varga K, Highfield JA, Wolfrom BD, Philbrick KL, Ely EW, Jackson JC, Gajic O, Ahmad SR, Niven AS. Stress and fear: clinical implications for providers and patients (in the time of COVID-19 and beyond). InMayo Clinic Proceedings 2020 Nov 1 (Vol. 95, No. 11, pp. 2487-2498). Elsevier.
19. Wittenberg E, Goldsmith JV, Chen C, Prince-Paul M, Johnson RR. Opportunities to improve COVID-19 provider communication resources: A systematic review. Patient education and counseling. 2021 Mar 1;104(3):438-51.
20. Gee PM, Weston MJ, Harshman T, Kelly LA. Beyond burnout and resilience: the disillusionment phase of COVID-19. AACN Advanced Critical Care. 2022 Jun 15;33(2):134-42.
21. Vindrola-Padros C, Andrews L, Dowrick A, Djellouli N, Fillmore H, Gonzalez EB, Javadi D, Lewis-Jackson S, Manby L, Mitchinson L, Symmons SM. Perceptions and experiences of healthcare workers during the COVID-19 pandemic in the UK. BMJ open. 2020 Nov 1;10(11):e040503.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Manashree Mane, Swati Kemothi, Vijay Jagdish Upadhye, Debasmita Rath, Anubhav Bhalla, Sidhant Das, A.R. Shinde.
Methodology: Manashree Mane, Swati Kemothi, Vijay Jagdish Upadhye, Debasmita Rath, Anubhav Bhalla, Sidhant Das, A.R. Shinde.
Software: Manashree Mane, Swati Kemothi, Vijay Jagdish Upadhye, Debasmita Rath, Anubhav Bhalla, Sidhant Das, A.R. Shinde.
Drafting - original draft: Manashree Mane, Swati Kemothi, Vijay Jagdish Upadhye, Debasmita Rath, Anubhav Bhalla, Sidhant Das, A.R. Shinde.
Writing - proofreading and editing: Manashree Mane, Swati Kemothi, Vijay Jagdish Upadhye, Debasmita Rath, Anubhav Bhalla, Sidhant Das, A.R. Shinde.