doi: 10.56294/hl2024.403
ORIGINAL
Balancing Ethics and Professionalism: Acute Care Physical Therapy in COVID-19
Equilibrio entre ética y profesionalidad: Fisioterapia de cuidados intensivos en COVID-19
Supriya Awasthi1 ![]() , Jagdish Gohil2
, Jagdish Gohil2 ![]() , Uddhav T. Kumbhar3
, Uddhav T. Kumbhar3 ![]() , Debashree Priyadarshini4
, Debashree Priyadarshini4 ![]() , Jaspreet Sidhu5
, Jaspreet Sidhu5 ![]() , Nitish Vashisht6
, Nitish Vashisht6 ![]()
1School of Allied Health Sciences, Noida International University, Greater Noida, Uttar Pradesh, India.
2Parul Institute of Medical Sciences and Research, Parul University, Vadodara, Gujarat, India.
3Krishna Institute of Medical Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”, Department of Community Medicine, Taluka-Karad, Dist-Satara, Pin-415 539, Maharashtra, India.
4IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Paediatrics, Bhubaneswar, Odisha, India.
5Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
6Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
Cite as: Awasthi S, Gohil J, Kumbhar UT, Priyadarshini D, Sidhu J, Vashish N. Balancing Ethics and Professionalism: Acute Care Physical Therapy in COVID-19. Health Leadership and Quality of Life. 2024; 3:.403. https://doi.org/10.56294/hl2024.403
Submitted: 15-03-2024 Revised: 03-08-2024 Accepted: 07-11-2024 Published: 08-11-2024
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
The physical therapists’ moral dilemmas in assisting patients with COVID-19. The difficulties physical therapists experienced in terms of their profession and morals during the COVID-19 outbreak this research looked at their experiences. Individual interviews were analysed in the present research using reflexive theme analysis, a technique reflexive thematic analysis (RTA) developed for qualitative research. The analysis of these coded interviews yielded 4 main themes and related subthemes: ensuring attentive care and favorable working conditions, Instability, The function of a physical therapist, Feelings. During COVID-19, physical therapists encountered a wide range of ethics and professional problems on an individual, organizational, and social level. Research emphasizes a desire to provide physical therapists with the knowledge and tools need to be prepared for the moral and professional challenges will face in pandemics. Physical therapists’ role in pandemics is clarified, and staff members must be trained to handle anxiety; pandemics bring uncertainty and organizational adjustments. Organizations might create equitable triage methods and allocate limited resources for acute care physical therapy. Physical therapy practice and health care have substantially changed due to the COVID-19 epidemic. Research presents the results of initial research; knowledge highlighted the ethic that acute care physical therapy professionals were facing in relation to the COVID-19 outbreak that consultants had to navigate. Physical therapists may benefit from the research’s findings in preparing and dealing with challenges that arise in acute treatment during a pandemic.
Keywords: Ethics, Professional Issues; Physical Therapists; Acute Care; Professional-Patient Relations.
RESUMEN
Los dilemas morales de los fisioterapeutas al asistir a pacientes con COVID-19. Las dificultades que los fisioterapeutas experimentaron en términos de su profesión y la moral durante el brote de COVID-19 esta investigación examinó sus experiencias. Las entrevistas individuales se analizaron en la presente investigación utilizando el análisis temático reflexivo, una técnica de análisis temático reflexivo (ACR) desarrollada para la investigación cualitativa. El análisis de estas entrevistas codificadas arrojó 4 temas principales y subtemas relacionados: garantizar una atención atenta y condiciones de trabajo favorables, Inestabilidad, La función de un fisioterapeuta, Sentimientos. Durante el COVID-19, los fisioterapeutas se encontraron con una amplia gama de problemas éticos y profesionales a nivel individual, organizativo y social. La investigación hace hincapié en el deseo de proporcionar a los fisioterapeutas los conocimientos y herramientas necesarios para estar preparados ante los retos morales y profesionales a los que se enfrentarán en las pandemias. Se aclara el papel de los fisioterapeutas en las pandemias, y los miembros del personal deben recibir formación para manejar la ansiedad; las pandemias conllevan incertidumbre y ajustes organizativos. Las organizaciones podrían crear métodos de triaje equitativos y asignar recursos limitados para la fisioterapia de agudos. La práctica de la fisioterapia y la atención sanitaria han cambiado sustancialmente debido a la epidemia de COVID-19. La investigación presenta los resultados de la investigación inicial; los conocimientos pusieron de relieve la ética a la que se enfrentaban los profesionales de fisioterapia de cuidados intensivos en relación con el brote de COVID-19 que los asesores tuvieron que sortear. Los fisioterapeutas pueden beneficiarse de los resultados de la investigación a la hora de prepararse y afrontar los retos que surgen en el tratamiento de agudos durante una pandemia.
Palabras clave: Ética, Cuestiones Profesionales; Fisioterapeutas; Cuidados Agudos; Relaciones Profesional-Paciente.
INTRODUCTION
Critical patient care’s professional pressures and dangers substantially changed due to the COVID-19 epidemic. It was discovered that crucial healthcare personnel and members of their households had a much higher risk of having severe COVID-19. Lack of Personal Protective Equipment (PPE) made it harder for nurses to lower workplace risks. Many nurses said that little managerial assistance or attention was given to the heightened risk and stress that their working environment presented. As a result, nurses who are caring for patients with COVID-19 report more psychological anguish, dread, and intention to quit their employment.(1) Increased use of PPE, digital platforms for care delivery, and improvements to care delivery methods was among the technique changes that physical therapists noted. Healthcare systems, however, faced several uncertainties due to frequent revisions to safety guidelines, availability of resources, including PPE, and shifting COVID caseloads.(2) Healthcare professionals reported dread, worry, tension, uncertainty, sadness, moral anguish, and “moral injury” in COVID-19. Due to this epidemic, there is much debate about professional and ethical difficulties in medicine and other healthcare fields. The COVID-19 pandemic presents several ethical challenges, such as changing Patient-centered public health frameworks, allocating few resources, implementing fair patient triage procedures, psychological consequences of systemic bias, ambiguity, and other factors on patients’ rights defense under challenging situations healthcare workers.(3) Physical therapy practice faced unprecedented challenges of professionalism and ethics because to the financial hardships caused by the COVID-19 epidemic, unpredictability, risk of exposure, and extensive consequences. Applied professional ethics has recognized the value of practitioners’ moral backgrounds in medicine, healthcare, and Physical Therapy. The early emphasis on normative rational philosophical analysis in professional ethics has given way to integrating social science research that emphasizes contextual moral experience.(4) At a moment when their expertise is most needed, Healthcare Personnel (HCPs) may leave a hospital bed because of lowered professional Quality of Life (QOL) and increased moral unrest. The scholarship that is currently available on COVID-19 concentrates on, although there is a lack of research on patient diagnosis and Therapy, its effect on shifting standards of care and leadership on moral pain and professional QOL of HCPs during the COVID-19 epidemic.(5)
Respiratory therapists and nurses in a big university medical centre provided direct care for the initial wave COVID-19 epidemic facility using qualitative research techniques.(6) The investigated the ethical dilemmas that Intensive Care Unit (ICU) nurses and doctors encountered, and arrived at decisions throughout its initial and subsequent “COVID-19 pandemic waves”. The COVID-19 pandemic epidemic caused a dramatic increase in hospital admissions and morbidity, placing a heavy therapeutic strain on Intensive Care Units (ICUs).(7) In reaction to an increased burden brought on by caring for severely sick COVID-19 patients, intensive care nurses reported experiencing both physical and mental stress.(8) To despite a diagnosis and Therapy of Guillain-Barré syndrome (GBS) associated with COVID-19 at local ACH, offers a case report outlining rehabilitation and release procedures for a patient with an independent Long-term Acute Care Hospital (LTACH) facility.(9) The applicable pandemic surge guidelines that were developed by the Task Force for Mass Critical Care (TFMCC) contained an orderly combination of gray evidence from general publications, anecdotal experience data, peer-reviewed research, and other essential information.(10) The affected an intense, multimodal, inpatient rehabilitation program for patients with COVID-19 who had recently left a critical care facility regarding their neuromuscular, respiratory, and functional deficits.(11) The effects COVID-19 epidemic on mental health, work-life balance, also readiness into continue at their existing positions were the main objectives targeted at Canadian Critical Care Nurses (CCNs).(12)Intended to comprehend professional and personal life were affected by working during the COVID-19 pandemic, people felt about institutional assistance, influence measures to lower consequences of COVID-19 and future pandemics.(13) The design for physiotherapists and other key players in an acute medical context that works with adult individuals have confirmed or suspected COVID-19.(14) The COVID-19 pandemic and the experiences of hospital professionals in allied health, including any moral unease or moral conundrums it could have encountered.(15) When limitations hinder healthcare professionals from behaving according to their fundamental moral principles, moral discomfort develops during the current Covid-19 to provide high-quality patient care outbreak, and the moral anguish experienced by nurses may be amplified.(16) The difficulties that COVID-19 presented to therapists working at a paediatric hospital before these difficulties were resolved.(17) The examined a case of ethical challenges that an assisted living institution must balance community administration with a resident’s right to self-determination and autonomy.(18) The discussion of the events surrounding COVID-19 and gave a general description of the burnout phenomenon, its causes, and its effects. This Quality Improvement (QI) initiative aimed to implement several interventions to improve utilization. Physical therapists in acute care are responsible for analyzing and interpreting Standardized Tests and Outcome Measures (STOM).(19)
METHOD
The purpose of reflexive thematic analysis (RTA), a qualitative research technique created to find, examine, and interpret themes or patterns in qualitative data. RTA, in contrast to standard theme analysis highlights how crucial it is for the researcher to actively participate in the analytical process and acknowledges the impact of the researcher’s perspectives, experiences, and prejudices on the data interpretation. It fosters a more profound interaction with the content, enabling experts to contemplate their own positioning and the circumstances surrounding the data collection, ultimately producing more profound and intricate understandings. A qualitative research method called RTA that was utilized in this research to examine physical therapists that participated individually in semi-structured interviews. A type of qualitative research known as RTA focuses on a researcher’s reflexive interaction with theory, data, and interpretation. By emphasizing researcher interaction above coding accuracy or other qualitative procedures, thematic analysis varies from qualitative methodologies. Briefly describe the three primary forms of theme analysis: reflexive, codebook, and coding reliability. Figure 1 shows the RTA process.
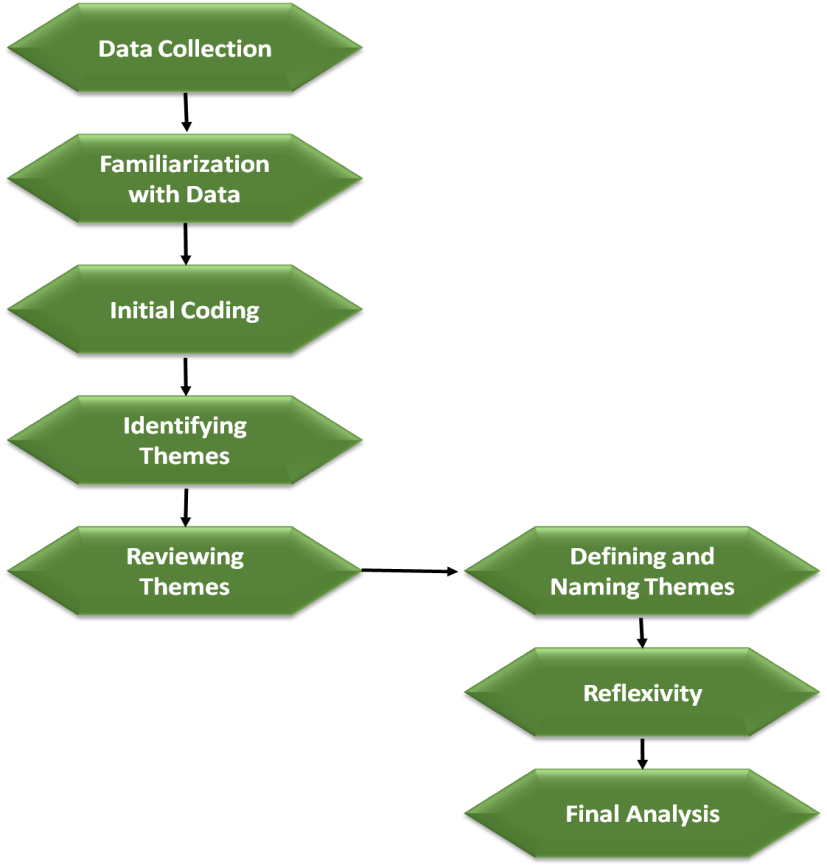
Figure 1. RTA process
According to them, RTA is a methodology that most closely adheres to its original idea, a qualitative strategy that emphasizes a researcher’s subjective perspective and source of analytic information. RTA concentrates on a researcher’s interpretation instead of qualitative research, emphasizing emergent themes, researcher bias, coding reliability, and coder agreement. Focusing consensus and researcher bias is typical as being at odds with RTA. Process facilitation and adherence to deadlines and consensus techniques are accepted in RTA. Researchers chose the RTA technique because it is adaptable, transparent, and suitable to support the contextual character.
Respondents
The transcriptions of 50 one-on-one interviews conducted with physical therapists throughout the COVID-19 pandemic were included in the dataset. Ensuring favorable working conditions and careful attention to detail, instability, the function of the physical therapist, and feelings were the four primary categories that were identified from the data. Each of these topics included three to four subthemes. The participants came from five distinct areas and ten different healthcare settings. Demographic information such as years of experience (from 1 to more than 20 years) and professional jobs are included in table 1.
|
Table 1. Demographic data |
||
|
Demographic Variable |
Categories |
Count (n=50) |
|
Experience in years |
one to five years |
12 |
|
|
Six to ten years |
15 |
|
|
Eleven to fifteen years |
10 |
|
|
sixteen to twenty years |
8 |
|
|
Twenty years above |
5 |
|
Work Setting |
Hospital Acute Care |
18 |
|
|
Rehabilitation Facility |
10 |
|
|
Home Health |
8 |
|
|
Long-Term Care |
6 |
|
|
Outpatient Clinic |
8 |
|
Gender |
Female |
30 |
|
|
Male |
20 |
|
Role |
Senior Physical Therapist |
20 |
|
|
Junior Physical Therapist |
30 |
Data Acquisition
A number of well-constructed interview questions were used to address important subjects to provide a look at the observations of physical therapists during the COVID-19 epidemic. These included shifts in organizational structure, the dynamics of healthcare teams, healthcare legislation, moral standards, the unique function of physical therapists, and the social difficulties are encountered. Through in-depth interviews, primary data was acquired, giving participants the chance to express their opinions and thoughts on the moral and professional difficulties were faced in their line of employment. A thorough grasp of the complex effects of the pandemic on physical therapy was made possible by this qualitative method.
RESULT
The analysis of coded interviews identified four main categories reflecting physical therapists’ perspectives throughout the COVID-19 epidemic. Ensuring attentive care and favorable working conditions highlights the challenges in maintaining quality care. Instability addresses the uncertainties faced in healthcare settings. The function of a physical therapist explores their evolving roles within multidisciplinary teams. Lastly, feelings capture the emotional responses of therapists, including stress and anxiety, revealing the profound impact of the pandemic on their professional lives.
Feelings
The psychological responses that result from treating patients during a pandemic are represented by feelings. A variety of feelings were expressed by the participants, including tension, guilt, fear, worry, fatigue, and irritation. The emotional toll was different for each person based on the workload and the period of the pandemic, but it affected everyone in the long run. These emotions frequently had an impact on their general well-being and ability to operate professionally, underscoring the significant psychological difficulties encountered by healthcare professionals. Table 2 shows the suggestions based on the results
Instability
The confusion and unpredictability were caused by inconsistent information and support, which was a defining feature of instability. The challenge resulted from the pandemic’s abrupt modifications to policies and procedures, which hampered team relationships, communication, and resource accessibility. Every facet of their work was plagued by an overwhelming feeling of unpredictability due to the continual growth of treatment choices and patient requirements. The participants highlighted the difficulties people had adjusting to a healthcare environment that was always changing by comparing this instability to traveling through dangerous conditions.
Ensuring Attentive Care And Favourable Working Conditions
The right conditions and sufficient emphasis on care emphasize the importance and the effects of the environment on care providers and care receivers. The use of personal protective equipment (PPE) for instance, has many implications on physiotherapy practitioners; effects on their health and their efficiency in providing services. These factors not only increase the work demands physiotherapists face, especially with a growing older patient population, but may also be oppressive. The treated space might have air conditioning, which may in turn feel less comforting than anticipated. Using gowns, masks, and face shields contributes to the discomfort physically, making it feel like a sweatshop. Care giving takes time and energy, especially when it involves heart rates or blood pressures of patients or their complaints that one has to be on the alert for all the time which is tiring to the body and the mind as well. These environments may exhaust both physical energy and healthy psychological states to a point where the care provided suffers.
The Function Of A Physical Therapist
A physical therapist performs and is expected to perform includes several elements associated with patient care and rehabilitation services. Further, the relevance of physical therapy to patients on acute treatment has been a debate in the wake of the corona virus disease. Many physical therapists made a vigorous case on their participation in the care of the COVID-19 patient’s significance of rehabilitation in the healing process. However, certain healthcare practitioners opposed the involvement of physical therapists on the ground, which focused mainly on whether rehabilitation treatment was deserved in such dire situations. In spite of these circumstances, physical therapists were willing to pay back relief care for so affected patients.
|
Table 2. Suggestions based on research results |
||
|
Strategies |
Action |
Domain |
|
Moral Principles |
Apply emergency moral principles to physical therapy. |
Individual |
|
Fair Allocation |
Outline methods for patient division and resource allocation. |
Individual |
|
Crucial Care |
Advocate for physical therapy across all patient stages. |
Individual |
|
Treatment Strategies |
Develop patient interaction strategies amid resource scarcity. |
Individual |
|
Ethical Training |
Promote training for DPT programs and practitioners. |
Individual |
DISCUSSION
Individual, organizational, and societal level, participants had significant problems with professionalism during the COVID-19 pandemic. Concerns expressed by physical therapists included PPE, uncertainty, equal resource allocation, redeployment, uncommon jobs, and preserving Core Values of Professionalism. It was difficult for physical therapists to strike a balance between public health or economic ethics and patient-centered ethics. It was mirrored in the therapy assessment, lack of family engagement, and patient prioritization. The outcomes emphasized aspects of physical therapy and rehabilitation. The rehabilitation therapy continuum was interrupted, according to the limiting the amount of time spent with patients, providing inadequate family education and support, having fewer staff members, and limiting access to facilities or equipment were some of the factors that affected concerns regarding release. Those physical therapists put the “greatest common good” a utilitarian principle above the interests of their particular patients.
Other moral and skilled concerns specific to physical therapy in the setting of organizations were also brought up, in addition to discharge. COVID-19 care regarded PPE’s importance or the opinions of other healthcare professionals as tricky, whether voluntary or required, in the COVID-19 team assignment procedure identified unfairness as a second organizational problem. Physical therapists with existing problems were protected by assignment voluntarily to COVID-19 units; those interested in treating COVID-19 patients had prospects for professional growth. Mandatory terms raise questions regarding the equitable distribution of possible exposure. A few instances of moral issues concerning the unpredictable nature of the clinical environment in the human and organizational domains are the condition, the use of PPE, and the need for healthcare teams and organizations to adapt quickly to change. The extent of uncertainty in health care was found to be “pervasive” and to have overlapping structural and foundations. Provide health systems, clinicians, patients, and families with comprehensive guidance on navigating ambiguity during the COVID-19 pandemic. This should include establishing novel pandemic designs, preparing physicians for unclear circumstances, and coming up with creative ways to include patients and families.
CONCLUSION
According to the research, physical therapists could benefit from receiving training in subjects like public health ethics, standards pertaining to pandemics in general and particular, adaptation techniques, and the disadvantages of isolating patients. The profession has created resources to promote reasonable physical therapy triage procedures, action, and communication plans in case of treatment changes, support for Physical Therapy, and crucial element of a continuum of treatment. Physical therapists could address moral and professional concerns brought an application of pandemic ethics in public health with more resources and education. Research’s sample size, while in line with requirements for theme analysis, is physical therapist assistants, physical therapists, and any facilities.
REFERENCES
1. Christianson J, Guttormson J, McAndrew NS, Calkins K. Impact of COVID-19 on intensive care unit nurse duty of care and professional roles: a qualitative content analysis. SAGE Open Nursing. 2022 Jul;8:23779608221113539. DOI: 10.1177/23779608221113539
2. Ditwiler RE, Swisher LL, Hardwick DD. Professional and ethical issues in United States acute care physical therapists treating patients with COVID-19: stress, walls, and uncertainty. Physical therapy. 2021 Aug 1;101(8):pzab122. https://doi.org/10.1093/ptj/pzab122
3. Griffin KM, Karas MG, Ivascu NS, Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. American journal of respiratory and critical care medicine. 2020 Jun 1;201(11):1337-44. https://doi.org/10.1164/rccm.202004-1037CP
4. Ditwiler RE, Swisher LL, Hardwick DD. Doing things you never imagined: Professional and ethical issues in the US outpatient physical therapy setting during the COVID-19 pandemic. Musculoskeletal Science and Practice. 2022 Dec 1;62:102684. https://doi.org/10.1016/j.msksp.2022.102684
5. Ness MM, Saylor J, DiFusco LA, Evans K. Leadership, professional quality of life and moral distress during COVID‐19: A mixed‐methods approach. Journal of nursing management. 2021 Nov;29(8):2412-22. https://doi.org/10.1111/jonm.13421
6. Trachtenberg S, Tehan T, Shostak S, Snydeman C, Lewis M, Romain F, Cadge W, McAuley ME, Matthews C, Lux L, Kacmarek R. Experiences of moral distress in a COVID‐19 intensive care unit: A qualitative study of nurses and respiratory therapists in the United States. Nursing inquiry. 2023 Jan;30(1):e12500.. https://doi.org/10.1111/nin.12500
7. Falcó‐Pegueroles A, Bosch‐Alcaraz A, Terzoni S, Fanari F, Viola E, Via‐Clavero G, Hoyo SG, Parini AM, Poveda‐Moral S, Parozzi M, Guàrdia‐Olmos J. COVID‐19 pandemic experiences, ethical conflict and decision‐making process in critical care professionals (Quali‐Ethics‐COVID‐19 research part 1): An international qualitative study. Journal of Clinical Nursing. 2023 Aug;32(15-16):5185-200. https://doi.org/10.1111/jocn.16633
8. Kagan I, Lancman N, Weisbord I. Experiences and psychosocial predictors of professional function among intensive care nurses under the shadow of Covid‐19: A mixed‐methods study. Journal of Nursing Scholarship. 2022 Nov;54(6):787-98. https://doi.org/10.1111/jnu.12796
9. Connors C, McNeill S, Hrdlicka HC. Occupational and physical therapy strategies for the rehabilitation of COVID-19-related Guillain-Barré syndrome in the long-term acute care hospital setting: case report. JMIR rehabilitation and assistive technologies. 2022 Feb 10;9(1):e30794.
10. Dichter JR, Devereaux AV, Sprung CL, Mukherjee V, Persoff J, Baum KD, Ornoff D, Uppal A, Hossain T, Henry KN, Ghazipura M. Mass critical care surge response during COVID-19: implementation of contingency strategies–a preliminary report of findings from the Task Force for Mass Critical Care. Chest. 2022 Feb 1;161(2):429-47. https://doi.org/10.1016/j.chest.2021.08.072
11. Rodrigues M, Costa AJ, Santos R, Diogo P, Gonçalves E, Barroso D, Almeida MP, Vaz IM, Lima A. Inpatient rehabilitation can improve functional outcomes of post-intensive care unit COVID-19 patients—a prospective study. Disability and rehabilitation. 2023 Jan 16;45(2):266-76. https://doi.org/10.1080/09638288.2022.2032408
12. Crowe S, Howard AF, Vanderspank B. The mental health impact of the COVID-19 pandemic on Canadian critical care nurses. Intensive and Critical Care Nursing. 2022 Aug 1;71:103241. https://doi.org/10.1016/j.iccn.2022.103241c
13. Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, Hodgson C, Jones AY, Kho ME, Moses R, Ntoumenopoulos G. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. Journal of physiotherapy. 2020 Apr 1;66(2):73-82. https://doi.org/10.1016/j.jphys.2020.03.011
14. van Oorsouw R, Oerlemans A, Klooster E, van den Berg M, Kalf J, Vermeulen H, Graff M, van den Wees P, Koenders N. A sense of being needed: a phenomenological analysis of hospital-based rehabilitation professionals’ experiences during the COVID-19 pandemic. Physical therapy. 2022 Jun 1;102(6):pzac052. doi: 10.1093/ptj/pzac052
15. Silverman HJ, Kheirbek RE, Moscou-Jackson G, Day J. Moral distress in nurses caring for patients with Covid-19. Nursing Ethics. 2021 Nov;28(7-8):1137-64. https://doi.org/10.1177/09697330211003217
16. Greenwood J, Fragala-Pinkham M, Dakhlian MG, Brennan E, Ploski C, Correia A. A pediatric hospital physical therapy and occupational therapy department’s response to COVID-19: An administrative case report. Physical Therapy. 2021 Sep 1;101(9):pzab164. https://doi.org/10.1093/ptj/pzab164
17. de Campos AP, Daniels S. Ethical implications of COVID-19: palliative care, public health, and long-term care facilities. Journal of Hospice & Palliative Nursing. 2021 Apr 1;23(2):120-7.DOI: 10.1097/NJH.0000000000000735
18. Howell BA. Battling burnout at the frontlines of health care amid COVID-19. AACN advanced critical care. 2021 Jun 15;32(2):195-203. https://doi.org/10.4037/aacnacc2021454
19. McDonnell B, Stillwell S, Hart S, Davis RB. Breaking down barriers to the utilization of standardized tests and outcome measures in acute care physical therapist practice: an observational longitudinal study. Physical Therapy. 2018 Jun;98(6):528-38. https://doi.org/10.1093/ptj/pzy032
CONFLICTS OF INTEREST
None.
FINANCING
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Supriya Awasthi, Jagdish Gohil, Uddhav T. Kumbhar, Debashree Priyadarshini, Jaspreet Sidhu, Nitish Vashisht.
Investigation: Supriya Awasthi, Jagdish Gohil, Uddhav T. Kumbhar, Debashree Priyadarshini, Jaspreet Sidhu, Nitish Vashisht.
Methodology: Supriya Awasthi, Jagdish Gohil, Uddhav T. Kumbhar, Debashree Priyadarshini, Jaspreet Sidhu, Nitish Vashisht.
Writing - original draft: Supriya Awasthi, Jagdish Gohil, Uddhav T. Kumbhar, Debashree Priyadarshini, Jaspreet Sidhu, Nitish Vashisht.
Writing - review and editing: Supriya Awasthi, Jagdish Gohil, Uddhav T. Kumbhar, Debashree Priyadarshini, Jaspreet Sidhu, Nitish Vashisht.