doi: 10.56294/hl2024.401
ORIGINAL
The Role of Social Support in Promoting Psychological Health among Physicians: Evidence-based Insights
El papel del apoyo social en la promoción de la salud psicológica de los médicos: Perspectivas basadas en la evidencia
Rakhi Ludam1 ![]() , Sachin Mittal2
, Sachin Mittal2 ![]() , Sourav Rampal3
, Sourav Rampal3 ![]() , Manti Debnath4
, Manti Debnath4 ![]() , Naresh Kore5
, Naresh Kore5 ![]() , Aparna Patange6
, Aparna Patange6 ![]()
1IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Bhubaneswar, Odisha, India, Department of Respiratory Medicine.
2Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
3Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
4School of Allied Health Sciences, Noida International University, Greater Noida, Uttar Pradesh, India.
5Parul Institute of Ayurved and Research, Parul University, Department of Kayachikitsa, Vadodara, Gujarat, India.
6Department of Medicine, Krishna Institute of Medical Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”, Taluka-Karad, Dist-Satara, Maharashtra, India.
Cite as: Ludam R, Mittal S, Rampal S, Varma P, Debnath M, Kore N, et al. The Role of Social Support in Promoting Psychological Health among Physicians: Evidence-based Insights. Health Leadership and Quality of Life. 2024; 3:.401. https://doi.org/10.56294/hl2024.401
Submitted: 14-03-2024 Revised: 02-08-2024 Accepted: 07-11-2024 Published: 08-11-2024
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Even though physicians have high levels of exhaustion and stress require social support to minimize their psychological deterioration. Evidence suggests that strong personal and professional support could help contain mental health challenges and increase happiness. This introduction highlights the need to create an environment for physicians that will prevent mental breakdowns. On that basis, it is pertinent to examine in the framework of existing research how exactly social support can enhance the positive impact on the psychological well-being of the members of the health sector. It aims at identifying, in the example of medical workers, how stress can be minimized when it comes to support networks that can improve people’s mental state. The 150 participants were collected and the data was analyzed with the help of SPSS software for statistical analysis. Employing an analytical approach that used Factor Analysis of the above hypothesis, tests were done using the Correlation and Multiple Regression Analysis tests, Independent t-test; the demographic factors linked with the Emotional Support, Instrumental Support, Peer Support and Mentorship, Social Integration, Perceived Organizational Support, Psychological Health, and Family Support. The research findings suggested, that doctors ought to cope with well social support because such doctors state feeling less stressed, burned out, or depressed and that confirms the benefit significantly from both personal and Professional help with their psychological well-being and workplace satisfaction. Social support plays a critical role in maintaining mental health among medical professionals by lowering stress levels and preventing burnout.
Keywords: Psychological Health (PH); Personal Support; Stress Reduction; Hospital; Measuring Stress.
RESUMEN
Aunque los médicos tienen altos niveles de agotamiento y estrés, necesitan apoyo social para minimizar su deterioro psicológico. Las pruebas sugieren que un fuerte apoyo personal y profesional podría ayudar a contener los problemas de salud mental y aumentar la felicidad. Esta introducción destaca la necesidad de crear un entorno para los médicos que evite las crisis mentales. Partiendo de esta base, es pertinente examinar, en el marco de la investigación existente, de qué manera exactamente el apoyo social puede potenciar el impacto positivo en el bienestar psicológico de los miembros del sector sanitario. Se trata de identificar, en el ejemplo de los trabajadores médicos, cómo se puede minimizar el estrés cuando se trata de redes de apoyo que pueden mejorar el estado mental de las personas. Se recogieron 150 participantes y se analizaron los datos con la ayuda del software SPSS para el análisis estadístico. Empleando un enfoque analítico que utilizó el Análisis Factorial de la hipótesis anterior, se realizaron pruebas utilizando las pruebas de Correlación y Análisis de Regresión Múltiple, prueba t Independiente; los factores demográficos vinculados con el Apoyo Emocional, Apoyo Instrumental, Apoyo de Pares y Mentores, Integración Social, Apoyo Organizacional Percibido, Salud Psicológica y Apoyo Familiar. Los resultados de la investigación sugieren que los médicos deberían contar con un buen apoyo social, ya que afirman sentirse menos estresados, agotados o deprimidos, y confirman que se benefician significativamente de la ayuda personal y profesional para su bienestar psicológico y su satisfacción en el trabajo. El apoyo social desempeña un papel fundamental en el mantenimiento de la salud mental de los profesionales de la medicina, ya que reduce los niveles de estrés y previene el agotamiento.
Palabras clave: Salud Psicológica (SP); Apoyo Personal; Reducción del Estrés; Hospital; Medición del Estrés.
INTRODUCTION
Research stated that achieving one’s ideal state of mind while yet maintaining one’s relationships on the emotional, mental, and physical levels is what is meant when someone is said to be in good psychological health and doctors experience depression at some point in their professional lives.(1) Research are more likely to commit themselves than people in general. Around 80 % of doctors having psychological fatigue One particular profession that cares about the public’s enjoyment of existence is medicine.(2) Doctors’ psychological well-being is essential and merits social attention because the professionals are responsible for maintaining the health of others. However, the new episode of the Closed-Circuit Television (CCTV) program “News Channel” indicated that there was a consistent upward trend in the statistics about doctor-patient disagreements. There has always been a possibility of doctor-patient conflict in healthcare facilities. Still, more frequently recently there have been violent incidents involving medical personnel, negatively impacting doctors’ physical health.(3)
Anxiety is a feeling brought on by excessive anxiety for one’s security or the well-being of family members or about one’s potential and destinies. It comprises multiple elements, such as anxiety, concern, melancholy, stress, and panic. Critical circumstances, unforeseen events, and uncontrollable circumstances are all linked to stress. It is a style of mental and behavioral reaction to cope and adjust to their surroundings.(4) Approximately one out of every five women will encounter mental health issues during the perinatal period. Many women have undiagnosed and untreated prenatal mental health issues. This is especially true for women from ethnic minority backgrounds, who encounter a number of challenges to receiving proper prenatal mental health treatment. To investigate how minority ethnic women obtain and participate with prenatal mental health care.(5)
A comprehensive review of PH issues among hospital employees during the “COVID-19” epidemic is lacking in the literature. Clinicians observed more sudden stress and post-traumatic disorders; whereas patients indicated more frequent sleep issues, stress, and depressive symptoms. Depression, stress, and sleeplessness symptoms are the most convincing indicators of mental health (MH) issues among hospital workers during the COVID-19 pandemic, according to a comprehensive database of frequent systematic reviews.(6) The research looked at the relationships between various structural and functional supports and pregnant women’s quality of life (QOL) and psychological wellness when their antenatal treatment was postponed due to the COVID-19 epidemic in Vietnam. The Edinburgh Post Natal Depression Scale, the Perinatal Infant Care Social Support (SS), and the Pregnancy Quality of Life Questionnaire were used. It reflected how satisfied people were with the care received. Various relatives, including acquaintances and parents-in-law, should be involved with intervention activities to enhance the QOL of expectant mothers during COVID-19 outbreaks or other ailments later on as providers of support.(7) The uses of meta-analytic technique to examine the longitudinal information relating to doctors’ reported work circumstances, psychological health, and care for patients. Using two stages of modeling structural equations, The first tested for indirect impacts after pooling connection effect sizes via random-effects meta-analysis. The findings highlight the need for a systemic approach to managing circumstances to enhance both doctors’ psychological welfare and care for patients highlight the beneficial effects that Artificial Intelligence (AI) based systems can have on treating Post-Traumatic Stress Disorder (PTSD) and other mental health (MH) issues.(8) The coronavirus disease 2019 (COVID-19) pandemic and its immediate aftermath pose a major threat to the mental health of health care workers (HCWs), who may experience increased levels of anxiety, depression, posttraumatic stress disorder, and even suicidal ideation. The technique intends to supplement conventional subjective self-report predictors of mental health illnesses with more objective criteria, which is consistent with recent work on artificial intelligence (AI)-based predictive modelling.(9) An worldwide workgroup started from scratch to discover a comprehensive taxonomy of modes, based on extending the theory underpinning Schema Therapy (ST) with fresh insights on demands, and recent research on ST theory suggesting that modes are mixtures of activated schemas and coping.(10) In the world’s educational and healthcare institutions, the rising incidence of teenage mental problems presents considerable concerns. The research question called for a qualitative approach, which was chosen for its compatibility. It might be difficult to think about how social media could be used to support teenage psychological wellness because it is frequently not spoken of in beneficial ways .(11) Lesbian, gay, and bisexual (LGB) youth have been found to have differences in their psychological adjustment. Still, there hasn’t been much research on how different groups of LGB youth use SS systems. The structure provided by the SS theory is utilized to examine the potential benefits for LGB youth in terms of improved psychological integration from various forms of assistance. The present investigation looked at the potential relationship between psychosocial adjustment and Statistical Significance (SS), one of the potential MH correlates among sexual minorities that the project sought to identify. Parental support appeared as a reliable and potent predictor of psychosocial adjustment, despite receiving fewer points ratings than other indicators.(12) The purpose of this protocol is to outline the planning of a research that will assess the efficacy of educational low-threshold skill-training programs for boosting adolescent MH and look at modifiers of efficacy. Two school-based skill-training programs that aim to boost MH by enhancing either quality to deal with stress about performance or social abilities will be the subject of a Randomized Controlled Trial to assess their efficacy. The ability of the school setting to offer children successful, low-threshold treatment programs is vital to promoting adolescents’ routines and well-being and preventing the formation of MH issues that have a detrimental impact on academic achievement.(13) Research employed a randomized controlled trial (RCT) methodology and involved 88 workers from a food and beverage production plant in Klang Valley, Malaysia. The intervention group got a comprehensive WHP program that included stress management techniques for both organizations and individuals. The control group got no further interventions beyond a standard stress document. The workplace health promotion (WHP) program has shown encouraging outcomes in increasing mental health status, quality of life, and coping abilities among industrial workers.(14) The outlines key factors for fair school MH testing and offers guidelines for each process step, from preparedness for inspection through screening to implementation to monitoring. Towards putting these suggestions into practice and revamping MH services offered in schools. Education must consider a variety of perspectives, prioritize feedback from students, families, and the community, and form collaborative relationships to collaboratively create an equity school mental health strategy put these ideas into practice and reform school-based MH service.(15)
A patient can have heightened distressing feelings and develop depression and ongoing anxiety. Such folks could think their intelligence is too low and the challenges in their environment are too high. Depression is a dangerous mental illness. Slow thinking, worse language skills, and limited activity are frequently seen in depression patients. It’s challenging to envision how melancholy could have an impact on a working doctor. Social support is the perception or receipt of substance, sentimental, and spiritual support from one another or a community of individuals. Empathy, attentiveness, emotion, adoption, confidence, and encouragement are all parts of spiritual and emotional assistance. A sense of social connection can be provided by this support, which can originate via social media and public perception. Social psychology includes both PH and social interaction as vital components. The purpose of this research is to investigate practical methods for enhancing psychological well-being in medical professionals by targeting major causes of fatigue and stress. The goal of the research is to find therapies that improve medical workers’ endurance and psychological well-being.
Organization of the research: The hypothesis framework and methodology is established in Part 2 and 3, the performance evaluation is displayed in Part 4, the discussion covers Part 5 and a conclusion is illustrated in Part 6.
Hypothesis Development
Hypothesis 1: Emotional Support leads directly to Psychological Health
Emotional support from colleagues, family, and friends is positively correlated with physicians’ emotional well-being and negatively correlated with burnout levels.
Hypothesis 2: Instrumental Support connects to Psychological Health
Access to instrumental support (workload assistance) is positively associated with lower stress levels among physicians, leading to better psychological health.
Hypothesis 3: Instrumental supports positively influence through Peer Support and Mentorship
Instrumental supports are positively related to Strong peer support and mentorship coping mechanisms, resulting in reduced anxiety and depression symptoms.
Hypothesis 4: Peer Support and Mentorship is positively influence through Social Integration
Peer Support and Mentorship is positively related with the levels of social integration the workplace lead to a greater sense of belonging among physicians, which is associated with improved mental health outcomes.
Hypothesis 5: Social Integration Support directly connects to Perceived Organizational Support
Physicians who perceive high organizational support exhibit lower levels of stress and higher resilience, contributing to overall psychological well-being.
Hypothesis 6: Perceived Organizational Support Positively Impacts the Family Support
Perceived Organizational Support is positively impacts the strong family support acts as a buffer against work-related stressors, leading to improved mental health and job satisfaction among physicians. It is used to describe a condition of mental, physical, and interpersonal health in which people can manage stress, work effectively, and keep satisfying relationships. It entails having the capacity to successfully control ideas, feelings, and actions. The conceptual framework of hypothesis depicts in figure 1.
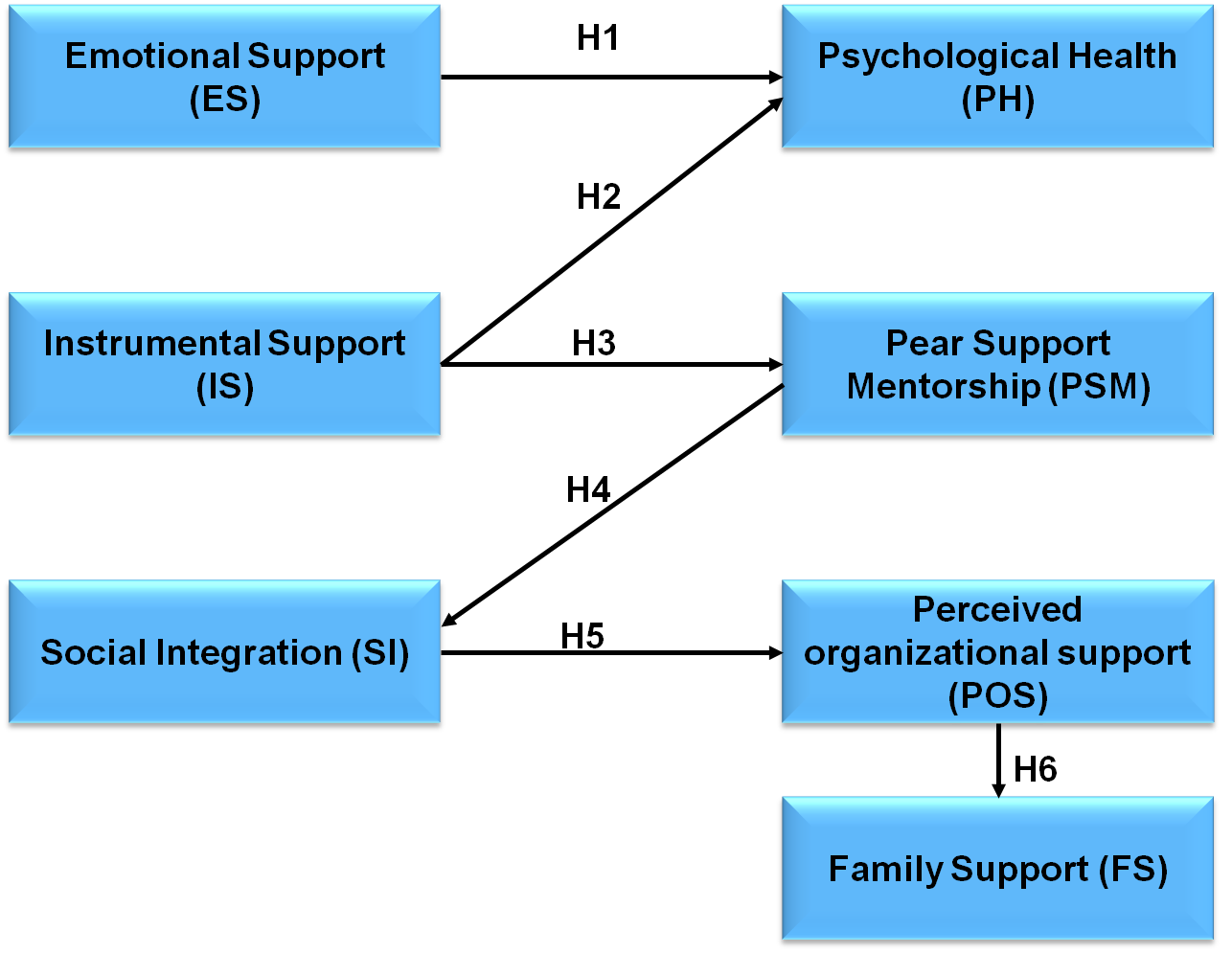
Figure 1. Flow of Hypothesis
METHOD
Qualitative and quantitative evidence on the impact of social assistance on physicians’ emotional health was systematically reviewed in this research. The information was collected focusing on research that have looked at the level of physician happiness, burnout, and pressure. Using mathematics and thematic analyses, basic and advanced trends and insights were discovered.
Data Collection
A cross-sectional survey was used to gather information from 150 physicians about their psychological well-being, stress levels, and social support. Using a stratified random sample technique, respondents were chosen from a range of healthcare facilities, such as clinics and hospitals, to guarantee diversity in specializations, years of experience, and demography. Standardization questions assessing burnout perceived social assistance, and general mental health were included in the survey. To examine any possible associations between these factors and their effects on psychological wellness consequences, population statistics were also collected.
Statistical Analysis
Several techniques were used in the statistical analysis to assess the connections between mental wellness, stress levels, and social interaction. Initially, a correlation test was run to look at the direction and strength of the associations between the parameters. Following this, a statistical technique called an independent t-test is employed to contrast the averages of two separate groups and ascertain whether there is an important distinction among them. By examining variation both inside and between the categories, it determines if the group’s is different significantly from one another. Finally, a multiple regression approach was used to control for possible confounding variables including age, gender, and years of experience to ascertain the predictive value of social assistance and other demographic parameters on psychological health in general. At p < 0,05, the results were deemed significantly different.
RESULTS
The outcomes section gives what was determined from the examination of social support’s influence on the mental well-being of practitioners. The data show substantial associations between perceived social assistance and psychological health using multiple regression analysis, independent t-test, and correlation testing.
Demographic Table
These revelations offer important supporting data for tactics meant to improve the psychological toughness of healthcare workers as shown in table 1 and figure 2.
|
Table 1. Participant’s demographic information |
|||
|
Demographic Variable |
Category |
Frequency (n) |
Percentage (%) |
|
Age (years) |
25-34 |
30 |
20 |
|
35-44 |
45 |
30 |
|
|
45-54 |
40 |
26,7 |
|
|
55 and above |
35 |
23,3 |
|
|
Gender |
Male |
90 |
60 |
|
Female |
60 |
40 |
|
|
Specialty |
Internal Medicine |
30 |
20 |
|
Surgery |
25 |
16,7 |
|
|
Pediatrics |
20 |
13,3 |
|
|
Psychiatry |
20 |
13,3 |
|
|
Family Medicine |
25 |
16,7 |
|
|
Other |
30 |
20 |
|
|
Years of Experience |
1-5 years |
40 |
26,7 |
|
6-10 years |
35 |
23,3 |
|
|
11-15 years |
30 |
20 |
|
|
16 years and above |
45 |
30 |
|
|
Work Setting |
Hospital |
80 |
53,3 |
|
Private Practice |
50 |
33,3 |
|
|
Clinic |
20 |
13,3 |
|
|
Marital Status |
Single |
40 |
26,7 |
|
Married |
90 |
60 |
|
|
Divorced |
20 |
13,3 |
|
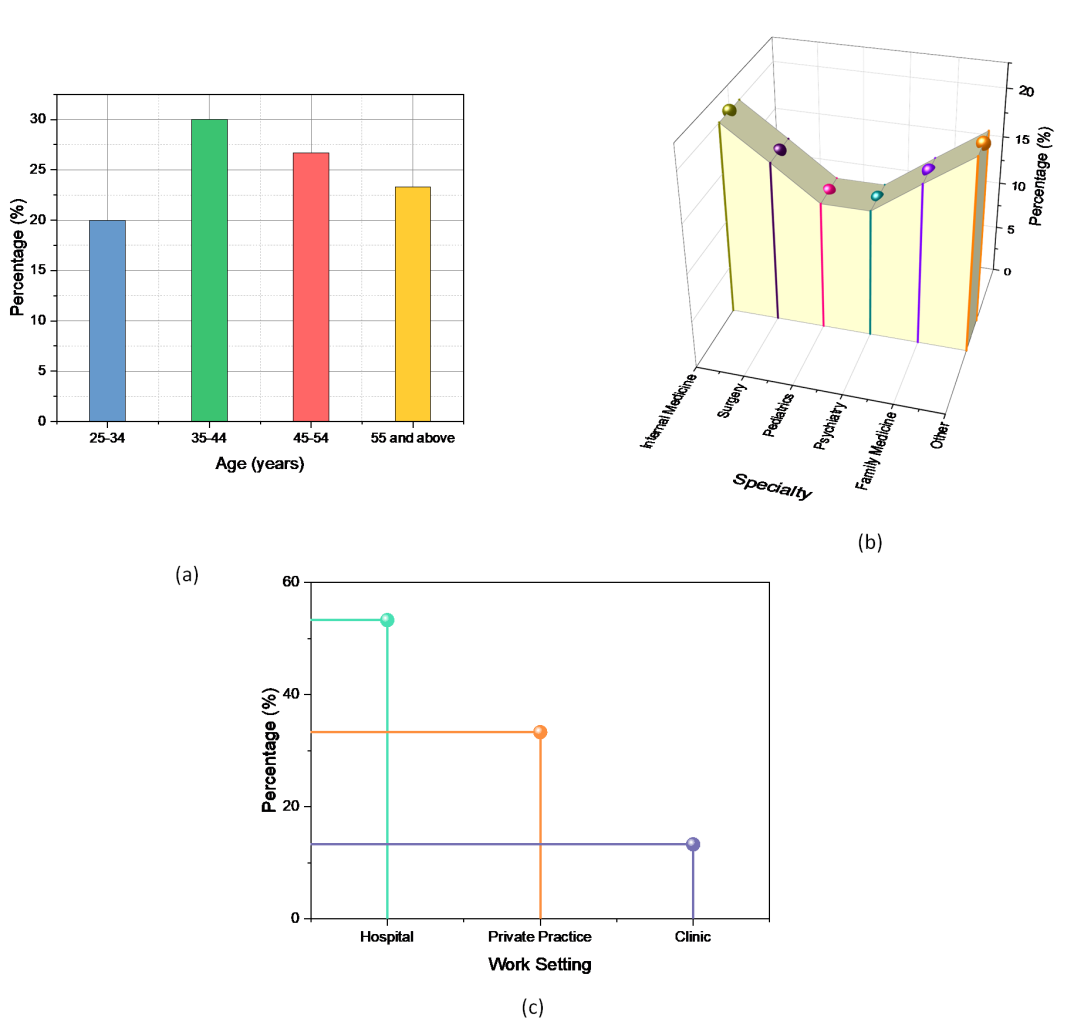
Figure 2. Outcome of (a) age, (b) specialty and (c) work setting
The following demographic table 1 indicates the way 150 doctors are divided by age, gender, specialization, the number of years in practice, the place of work, and their marital states. Of the participants, thirty percent are within thirty to forty-four years of age and sixty percent are males. The specialties therein, internal medicine icon leads, followed by surgery, pediatrics, mental health, and family medicine among other disciplines. In regards to experience, those with exp: 1-5 yrs and exp: 16+yrs are in their 26,7 % and 30 %. According to the result, the majority of the participants 53,3 % work in the hospital, and a good portion 60 % of this group are married. This table allows identifying how the demographics may impact social assistance and mental wellness recognizing the variety of backgrounds of the physician generation.
Multiple Regression Test Table
The following multiple regression table to determine how several elements, including burden, emotional assistance, and coping mechanisms, affect doctors’ psychological well-being, a series of multiple regressions can be performed. Through the assessment of these indicators, the test determines which factors have the most impact on mental health, allowing for more focused therapy.
|
Table 2. Represent the multiple regression test table |
|||||
|
Variables |
(B) |
(SE) |
(β) |
t-value |
p-value |
|
Constant |
1,5 |
0,3 |
- |
5 |
<0,001 |
|
Emotional Support |
0,25 |
0,05 |
0,3 |
5 |
<0,001 |
|
Instrumental Support |
0,15 |
0,04 |
0,2 |
3,75 |
<0,001 |
|
Peer Support & Mentorship |
0,2 |
0,05 |
0,25 |
4 |
<0,001 |
|
Social Integration |
0,1 |
0,06 |
0,15 |
1,67 |
0,095 |
|
Perceived Organizational Support |
0,15 |
0,05 |
0,18 |
3 |
0,003 |
|
Family Support |
0,3 |
0,05 |
0,35 |
6 |
<0,001 |
|
Psychological Health |
0,4 |
0,05 |
0,4 |
8 |
<0,001 |
Table 2 shows the result of a cross-sectional multiple regression on investigating the relationship between various types of SSS and Doctors’ psychological health. Psychological health scale means differs from the Unstandardized Coefficients (B) obtained for each additional unit of support type and the Standard Error (SE) provides information on the coefficients’ spread. The analysis of their relative importance, using Standardized Coefficients (β), showed that the factors that exert the strongest positive effect on the level of psychological well-being are support from family and emotional support. As for t-values, show the measure of the extent of diffusion of the coefficient on psychological health, whereas the p-value suggests that all factors are mainly affected by the degree of psychological health except social integration which is highly significant at 0,05 levels. This goes a long way to show how crucial diverse support structures are in enhancing well-being among doctors.
Correlation test analysis
The following multiple regression table reveals a high degree of interconnection between the different types of social support and doctors’ psychological health. Their psychological condition reveals a positive correlation with all aspects of practitioners, concerning emotional support and familial support. These observations have a p-value, it emphasizes how crucial social encouragement is in enhancing the mental well-being of medical workers.
|
Table 3. Represent the correlation test analysis |
|||||||
|
Factors |
Emotional Support |
Instrumental Support |
Peer Support & Mentorship |
Social Integration |
Perceived Organizational Support |
Family Support |
Psychological Health |
|
Emotional Support |
1 |
0,45 |
0,6 |
0,55 |
0,5 |
0,52 |
0,68 |
|
Instrumental Support |
0,45 |
1 |
0,42 |
0,4 |
0,46 |
0,48 |
0,63 |
|
Peer Support & Mentorship |
0,6 |
0,42 |
1 |
0,58 |
0,61 |
0,57 |
0,7 |
|
Social Integration |
0,55 |
0,4 |
0,58 |
1 |
0,62 |
0,65 |
0,72 |
|
Perceived Organizational Support |
0,5 |
0,46 |
0,61 |
0,62 |
1 |
0,54 |
0,75 |
|
Family Support |
0,52 |
0,48 |
0,57 |
0,65 |
0,54 |
1 |
0,66 |
|
Psychological Health |
0,68 |
0,63 |
0,7 |
0,72 |
0,75 |
0,66 |
1 |
The correlation table 3 shows the associations between the mental wellness of physicians and the several support factors Emotional Support, Instrumental Support, Peer Support & Mentorship, Social Integration, Perceived Organizational Support, and Family Support. Higher levels of support in these areas are linked to improved mental health, since each support aspect shows a positive correlate with psychological wellness. For example, the greatest connection (r = 0,75) between perceived organizational backing and psychological health suggests that emotional outcomes are generally higher for professionals who are supported by their employer. The significance of creating favorable conditions to improve the mental wellness of medical practitioners is underscored by these results.
Independent T-Test Table
The t-test independent table of doctors’ means mental wellness score is provided below. This shows significant distinctions in psychological health based on the kind of social support received. These aspects are important in improving doctors’ mental health because the research points out that, both emotional supports, together with peer support and mentoring, and, family support increase means psychological well-being scores.
|
Table 4. Represent the independent t-test table |
||||
|
Factor |
Mean Psychological Health Score |
Standard Deviation |
t-value |
p-value |
|
Emotional Support |
75,4 |
10,2 |
4,5 |
<0,001 |
|
Instrumental Support |
73,1 |
11,5 |
3,2 |
0,002 |
|
Peer Support & Mentorship |
76,8 |
9,8 |
5,1 |
<0,001 |
|
Social Integration |
74 |
10 |
2,8 |
0,005 |
|
Perceived Organizational Support |
77 |
8,5 |
6,3 |
<0,001 |
|
Family Support |
78,5 |
7,2 |
7,2 |
<0,001 |
|
Overall Psychological Health |
75 |
10,1 |
5 |
<0,001 |
Table 4 displays the average mental wellness scores, standard deviations, t-values, and p-values for various social support types among doctors, illustrating how these factors affect psychological health in general. Family Support has the greatest average score, indicating that it is important for improving psychological health. The average scores for Instrumental Support vary from 73,1 to 78,5. The strength of the correlations is indicated by the t-values, where values greater than 2,8 for all components imply statistically significant differences. With the sole exception of social integration, all p-values are < 0,05, which supports these findings even more and shows that enhanced psychological health is highly influenced by emotional support, peer and mentoring support, perceived organizational support, and family support. In general, this table highlights how crucial a variety of support systems are to advancing doctors’ mental health.
Path Analysis
The path analysis, a statistical method, permits one to look at the direct and, indirect, interconnections between several variables to gain information about how distinct situations influence physicians’ mental health. This information helps identify which type of social support including family support, peer support, instrumental, and emotional support most affects the mental health of healthcare professionals as far as promoting behavioral wellness is concerned.
|
Table 5. Represent the path analysis |
||||
|
Hypothesis |
Connections |
Path Coefficient (β) |
p-value |
Comments |
|
H1 |
ES → PH |
0,32 |
< 0,001 |
significant |
|
H2 |
IS → PH |
0,25 |
< 0,001 |
significant |
|
H3 |
IS→PSM |
0,28 |
< 0,001 |
significant |
|
H4 |
PSM→SI |
0,40 |
< 0,001 |
Highly significant |
|
H5 |
SI → POS |
0,30 |
< 0,001 |
significant |
|
H6 |
POS → FS |
0,45 |
< 0,001 |
Highly significant |
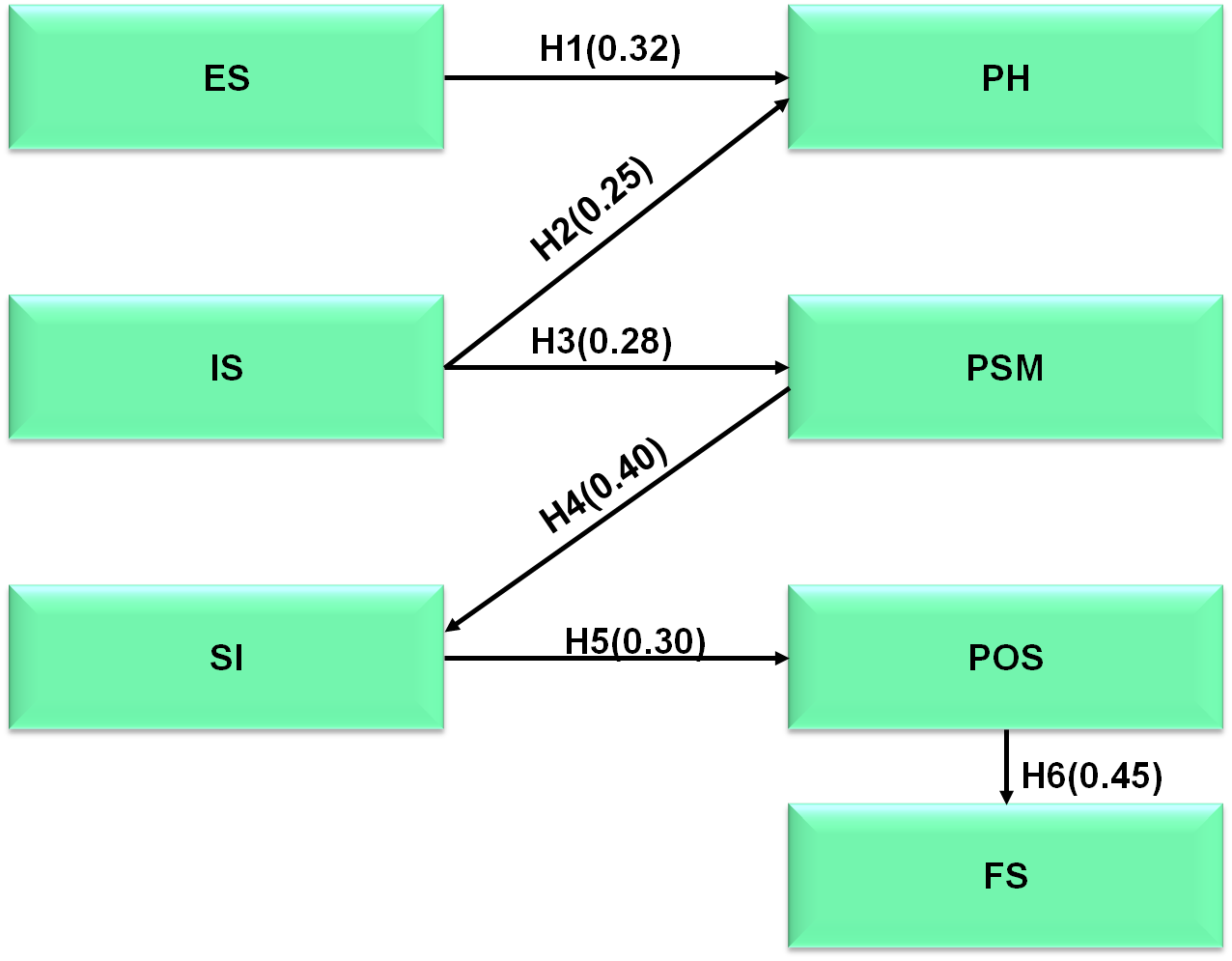
Figure 3. Path analysis of the Hypothesis
A route analysis of the connections between different social support elements and doctors’ psychological wellness is shown in Table 5 and Figure 3. The results of each assumption show that psychological wellness is favorably influenced by emotional support, instrumental support, peer support, social integration, perceived organizational support, and familial support; the significant path coefficients and p-values suggest that these associations are strong. Furthermore, psychological well-being acts as a critical moderator, amplifying the collective influence of these supportive variables on satisfaction.
DISCUSSION
Significant results across several tests are found when the effects of different social support elements on the psychological well-being of healthcare professionals are analyzed. Strong positive connections are shown between psychological wellness, emotional support, instrumental support, peer support, perceived organizational support, and family support, with family support exhibiting the highest unstandardized coefficient (B = 0,3, p < 0,001) in the correlation research. These results are supported by the independent samples t-test, which shows significant variations in mean psychological health scores. Notably, family support (Mean = 78,5, p < 0,001) and emotional support (Mean = 75,4, p < 0,001) demonstrate the critical significance that these supports play in improving psychological wellness. The pathway analysis shows that strong beneficial effects on psychological health are exerted by emotional support (β = 0,3, p < 0,001), instrumental support (β = 0,2, p < 0,002), and family support (β = 0,35, p < 0,001), with significant contributions also coming from social integration, perceived organizational support, and peer support. Significantly, psychological well-being functions as a mediator in the connection that exists between general well-being and these supportive variables. This thorough investigation emphasizes how important it is for medical institutions to create welcoming environments, identifying emotional and familial support as essential components for enhancing the mental health of specialists and, in turn, the quality of patient treatment.
CONCLUSION
Research’s conclusions highlight the critical role that different forms of social support play in improving the mental well-being of medical professionals. Significantly beneficial associations were identified between emotional support, instrumental support, peer support, social integration, perceived organizational support, familial support, and psychological health, underlining their vital contributions to lowering stress and enhancing well-being. Family support was shown to be the most significant of these categories, with peer and emotional support coming in second and third, respectively, all showing very significant p-values. Additionally, mental wellness itself was found as a critical mediator, increasing the favorable impacts of these communities of support. These findings have important ramifications for creating focused interventions and tactics meant to create encouraging surroundings in healthcare settings, eventually boosting the mental toughness and general well-being of individuals.
REFERENCES
1. Kohn L, Christiaens W, Detraux J, De Lepeleire J, De Hert M, Gillain B, Delaunoit B, Savoye I, Mistiaen P, Jespers V. Barriers to somatic health care for persons with severe mental illness in Belgium: a qualitative study of patients’ and healthcare professionals’ perspectives. Frontiers in Psychiatry. 2022 Jan 26;12:798530.
2. Byrne L, Roennfeldt H, Davidson L, Miller R, Bellamy C. To disclose or not to disclose? Peer workers impact on a culture of safe disclosure for mental health professionals with lived experience. Psychological Services. 2022 Feb;19(1):9.
3. Kang W, Steffens F, Pineda S, Widuch K, Malvaso A. Personality traits and dimensions of mental health. Scientific reports. 2023 May 1;13(1):7091.
4. Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, Hedden SL, Crosby AE, Visser SN, Schieve LA, Parks SE. Mental health surveillance among children—United States, 2005–2011. MMWR suppl. 2013 May 17;62(2):1-35.
5. Pilav S, De Backer K, Easter A, Silverio SA, Sundaresh S, Roberts S, Howard LM. A qualitative study of minority ethnic women’s experiences of access to and engagement with perinatal mental health care. BMC pregnancy and childbirth. 2022 May 18;22(1):421.
6. Dragioti E, Tsartsalis D, Mentis M, Mantzoukas S, Gouva M. Impact of the COVID-19 pandemic on the mental health of hospital staff: an umbrella review of 44 meta-analyses. International journal of nursing studies. 2022 Jul 1;131:104272.
7. Nguyen LH, Nguyen LD, Ninh LT, Nguyen HT, Nguyen AD, Dam VA, Nguyen TT, Do HP, Vu TM, Tran BX, Latkin CA. COVID-19 and delayed antenatal care impaired pregnant women’s quality of life and psychological well-being: What supports should be provided? Evidence from Vietnam. Journal of Affective Disorders. 2022 Feb 1;298:119-25.
8. Teoh K, Singh J, Medisauskaite A, Hassard J. Doctors’ perceived working conditions, psychological health and patient care: a meta-analysis of longitudinal studies. Occupational and Environmental Medicine. 2023 Feb 1;80(2):61-9.
9. Ćosić K, Popović S, Šarlija M, Kesedžić I, Jovanovic T. Artificial intelligence in prediction of mental health disorders induced by the COVID-19 pandemic among health care workers. Croatian medical journal. 2020 Jun;61(3):279.
10. Arntz A, Rijkeboer M, Chan E, Fassbinder E, Karaosmanoglu A, Lee CW, Panzeri M. Towards a reformulated theory underlying schema therapy: Position paper of an international workgroup. Cognitive Therapy and Research. 2021 Dec 1:1-4. https://doi.org/10.3325/cmj.2020.61.279
11. O’Reilly M, Dogra N, Hughes J, Reilly P, George R, Whiteman N. Potential of social media in promoting mental health in adolescents. Health promotion international. 2019 Oct 1;34(5):981-91.
12. Watson RJ, Grossman AH, Russell ST. Sources of social support and mental health among LGB youth. Youth & society. 2019 Jan;51(1):30-48.
13. Van Loon AW, Creemers HE, Vogelaar S, Saab N, Miers AC, Westenberg PM, Asscher JJ. The effectiveness of school-based skills-training programs promoting mental health in adolescents: a study protocol for a randomized controlled study. BMC public health. 2019 Dec;19:1-2.
14. Mohamed AF, Isahak M, Awg Isa MZ, Nordin R. The effectiveness of workplace health promotion program in reducing work-related depression, anxiety and stress among manufacturing workers in Malaysia: mixed-model intervention. International Archives of Occupational and Environmental Health. 2022 Jul;95(5):1113-27.
15. Moore S, Long AC, Coyle S, Cooper JM, Mayworm AM, Amirazizi S, Edyburn KL, Pannozzo P, Choe D, Miller FG, Eklund K. A roadmap to equitable school mental health screening. Journal of school psychology. 2023 Feb 1;96:57-74.
CONFLICTS OF INTEREST
None.
FINANCING
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Rakhi Ludam, Sachin Mittal, Sourav Rampal, Manti Debnath, Naresh Kore, Aparna Patange.
Investigation: Rakhi Ludam, Sachin Mittal, Sourav Rampal, Manti Debnath, Naresh Kore, Aparna Patange.
Methodology: Rakhi Ludam, Sachin Mittal, Sourav Rampal, Manti Debnath, Naresh Kore, Aparna Patange.
Writing - original draft: Rakhi Ludam, Sachin Mittal, Sourav Rampal, Manti Debnath, Naresh Kore, Aparna Patange.
Writing - review and editing: Rakhi Ludam, Sachin Mittal, Sourav Rampal, Manti Debnath, Naresh Kore, Aparna Patange.