doi: 10.56294/hl2024.396
ORIGINAL
Bariatric Surgery and Pregnancy: Impact on Maternal and Fetal Health
Cirugía Bariátrica y Embarazo: Impacto en la salud materna y fetal
Jagmeet
Sohal1 ![]() ,
RenukaJyothi S2
,
RenukaJyothi S2 ![]() ,
Dhairyasheel D. Patil3
,
Dhairyasheel D. Patil3 ![]() ,
Sameer Rastogi4
,
Sameer Rastogi4 ![]() ,
Ravindra5
,
Ravindra5 ![]() ,
Suvendu Narayan Mishra6
,
Suvendu Narayan Mishra6 ![]() ,
Nittin Sharma7
,
Nittin Sharma7 ![]()
1Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
2JAIN (Deemed-to-be University), Department of Biotechnology and Genetics, Bangalore, Karnataka, India.
3Krishna Institute of Medical Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”, Dept. of Medicine, Taluka-Karad, Dist-Satara, Maharashtra, India.
4School of Pharmacy, Noida International University, Greater Noida, Uttar Pradesh, India.
5Parul Institute of Nursing, Parul University, PO Limda, Tal. Waghodia, District Vadodara, Gujarat, India.
6IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Psychiatry, Bhubaneswar, Odisha, India.
7Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
Cite as: Sohal J, yothi S R, Patil DD, Rastogi S, Ravindra R, Narayan Mishra S, et al. Bariatric Surgery and Pregnancy: Impact on Maternal and Fetal Health. Health Leadership and Quality of Life. 2024; 3:.396. https://doi.org/10.56294/hl2024.396
Submitted: 29-03-2024 Revised: 14-08-2024 Accepted: 09-12-2024 Published: 10-12-2024
Editor:
PhD. Prof. Neela Satheesh
![]()
ABSTRACT
Introduction: to contrast the prenatal results of female patients prior to and following weight-loss surgery giving birth.
Method: a review of the literature was conducted at a hospital to examine the prenatal results of women who gave birth before and after having weight loss procedure. To account for confounders, a model with multiple logistic regression variables was created.
Results: 301 deliveries occurred before and 507 occurred after weight loss surgery across the research period. Following the procedure, there was a notable decrease in the incidence of fetal obesity (6,5 % vs. 4,5 %; P=0,002), hypertensive diseases (13,6 % vs.10,2 %; P=0,001), and metabolic syndrome (17,3 % vs. 11,0; P=0,009). The results indicated that there was an independent link between bariatric surgery and a decrease in the incidence of hypertension (OR: 0,29,87 %; CI 0,14-0,48; P=0,001), diabetes mellitus (OR: 0,42, 95 %; CI 0,26-0,67; P=0,001), and macros (-0,82; P=0,044).
Conclusions: bariatric surgery before pregnancy can enhance maternal health, though it must be carefully monitored to avoid nutritional deficits. Optimal prenatal care is critical for both fetal growth and maternal health.
Keywords: Diabetes mellitus; Macrosomia; Birth weight; Pregnancy complications; Fetal Health; Bariatric Surgery.
RESUMEN
Introducción: contrastar los resultados prenatales de las pacientes que dieron a luz antes y después de la cirugía de pérdida de peso.
Método: se realizó una revisión bibliográfica en un hospital para examinar los resultados prenatales de las mujeres que dieron a luz antes y después de someterse a un procedimiento de pérdida de peso. Para tener en cuenta los factores de confusión, se creó un modelo con múltiples variables de regresión logística.
Resultados: durante el periodo de investigación se produjeron 301 partos antes y 507 después de la cirugía de pérdida de peso. Tras el procedimiento, se produjo una notable disminución de la incidencia de obesidad fetal (6,5 % frente a 4,5 %; P=0,002), enfermedades hipertensivas (13,6 % frente a 10,2 %; P=0,001) y síndrome metabólico (17,3 % frente a 11,0 %; P=0,009). Los resultados indicaron que existía una relación independiente entre la cirugía bariátrica y la disminución de la incidencia de hipertensión (OR: 0,29; 87 %; IC: 0,14-0,48; P=0,001), diabetes mellitus (OR: 0,42,95 %; IC: 0,26-0,67; P=0,001) y macros (-0,82; P=0,044).
Conclusiones: la cirugía bariátrica antes del embarazo puede mejorar la salud materna, aunque debe ser cuidadosamente monitorizada para evitar déficits nutricionales. Un cuidado prenatal óptimo es fundamental tanto para el crecimiento fetal como para la salud materna.
Palabras clave: Diabetes Mellitus; Macrosomía; Peso al Nacer; Complicaciones del Embarazo; Salud Fetal; Cirugía Bariátrica.
INTRODUCTION
The word “bariatric surgery (BS)” refers to a variety of operations, involving biliopancreatic redistribution/duodenal shift, laparoscopic adapting surgical bypass of the stomach and gastro band. The weight-loss techniques per year in the increased for the majority of the 1990s and the early 2000s. The frequency of these operations grew, from about 8 500 in 1993 to a peak of almost 115,000 in 2004.(1) Surgery-induced weight loss should theoretically lower the Risk of delivery connected to fat issues, but the procedure can complicate things and have negative reactions that could be harmful to both the woman and her unborn child. There have been reports of pregnant and foetal fatalities after weight loss operation.(2) In addition to obesity’s detrimental effects on health, it also raises the possibility of negative effects for pregnant women and their unborn children, including macrosomia, caesarean deliveries, premature delivery, fetal malformations, and perinatal mortality. Weight also lengthens labor overall, delays recovery after epidurals or general anaesthesia, and raises the risk of postpartum bleeding, deep venous thrombosis, and pulmonary thromboembolism. Therefore, sufferers who are obese women are at an exceptionally high risk.(3)
The data for better pregnancy and perinatal outcomes in pregnant women, however, is conflicting. Women of reproductive age make up the bulk of those who have bariatric surgery (BS) in several nations. A severe energy (calorie) deficit is created via a procedure called BS, which modifies the form, length, and functionality of the digestive tract and encourages significant weight loss. Though many patients continue eating poorly after surgery and might be experiencing the discharge phenomenon, acid reflux, feeling sick, and vomited are all examples of these conditions not only make it difficult to get enough nourishment but also lead to minerals and vitamins shortages.(4) Since BS brings about major and long-lastin g weight loss, it is envisioned as a reliable treatment for extreme obesity. Patients from all over the world who have a body mass index (BMI) of 40 kg/m2 or more, as well as obesity-related comorbidities including hypertension are eligible for the treatment, according to Nutrients 2022. Although there is no gender difference in obesity statistics, Females make up 73,7 % of comment-bariatric cases with the majority of them being of reproductive age.(5) Three basic forms of BS are traditionally performed, each with a unique postoperative anatomical outcome. There are several different types of BS, such as limited surgery, which reduces digestive system and restricts the amount of food consumed, malabsorptive surgery (e.g., gastric bypass surgery), which bypasses the smaller intestines for improved absorbed nutrients, and a combination of the two.(6) Numerous studies on the impact of these operations on pregnancy have found that, when in contrast to patients with obesity, have lowered maternal and new born morbidity for these patients.
In particular, patients who have had BS experience a lower prevalence of gestational diabetes and gestational hypertension than obese people who have not had the type of surgery. There is currently no established reason for the rise in preterm deliveries and small for gestational age (SGA) newborns among pregnant women throughout the world.(7) It is important to inform obese women receiving BS that their chances of becoming pregnant after BS are increased. Pregnancies, in special, should be organized following the stage of maximal weight loss because to the possibility of nutritional deficits occurring soon after BS. The effects of micronutrient deficits on the health of offspring have not been thoroughly investigated. Recommendations advise waiting until weight has stabilized after BS, or at least 12 to 18 months, before getting pregnant. A multidisciplinary team must manage pregnant patients after BS, specifically to avoid nutritional deficits in the progeny.(8)
Long-term health issues for pregnant women can result from the practices the adopt. Pregnancy is thus not seen as a condition in and of itself needing a limitation of physical activity (PA), but rather as a unique period for modifying behavior. Despite the fact that it is accompanied with deep structural and physiologic alterations. The Guidelines for Gynaecology and Obstetrical Practices actually advocate PA throughout pregnancy and its inclusion by sedentary women prior to conception.(9) The habits that pregnant women develop can have a long-term impact on their health. Despite the significant anatomical and physiological changes that are linked to pregnancy, it is still thought of as a special time for behaviour adjustment and is not seen as a medical condition in and of itself that necessitates limitations on physical activity (PA) practices. In reality, PA during pregnancy and its integration before by sedentary women conception are recommended by the Guidelines for gynecology and obstetrical.(10)
Preeclampsia, the condition of macros and the pregnancy diabetes mellitus are only a few of the harmful obstetric outcomes that are linked to obesity across pregnancy. A growing body of research suggests that having bariatric surgery can lower the likelihood of these findings. The goal was to assess the advantages and disadvantages in view of prenatal outcomes of surgical weight loss in obese women.(11) The objectives of the study are used to identify women who are of age to conceive.(12) conducting obesity surgery, to ascertain the age and the women having the procedure, and to ascertain the effect of bariatric surgery on factors impacting reproduction and the outcome of pregnancies. Additionally, according to a number of studies, pregnancies that take place less than a year after bariatric surgery have a detrimental effect on the population’s health mother and baby and result in micronutrient deficiencies because the first year is when the patient has the most significant weight loss. Anemia, low vitamin B12 and folic acid levels, and other negative effects including anemia can result in nutritional malabsorption. (13) The results of in vitro fertilization (IVF) and obesity-related infertility are discussed in the article summary of the most recent research.(14)
They have also made an effort to draw recommendations concerning the hazards to the mother and the fêtes as well as the advantages of bariatric surgery. The surgical changeable bariatric band and the Roux-en-Y are the two most popular loss of weight treatments bands. To ascertain the impact of surgery to lose weight on mother and baby physical health of pregnancy, a comprehensive analysis was carried out in accordance with the Procedure of the Information Evaluation Library of the dieting and Management the Faculty.(15) The popular and highly effective treatment for obesity is bariatric surgery. Following these methods, getting pregnant has proven to be safe, with some maternal problem rates being lower than those linked to getting pregnant in obese women. To avoid reproduction during the phase of fast weight loss, current recommendations advocate deferring pregnancies beyond the initial year after surgery.(16) The research has examined all the available evidence in the literature and offered a thorough care plan for expecting mothers who have undergone weight-loss surgery.(17)
An integrated strategy for all facets of care is prioritized. Good pregnancies depend on providing sufficient preconception, prenatal, and postnatal support, with a focus on the right dietary supplements. The purpose of the study is to ascertain whether factors such as postoperative weight, pregnancy delivery after the procedure, the kind of the operation, increase in weight, and age of mother files conditions affect the risk for adverse birth outcomes in pregnant women who having had surgery to lose weight.(18) The literature on food intake following weight loss surgery and its associations with regard to foetal and pregnancy results was conducted using the Medline Plus and base stores of data, as well as a hand-search of sources. The inclusion criteria were met by 27 of the 306 initially, which included 2056 women who had deliveries following bariatric surgery. It was discovered that the mother’s levels of iron, magnesium, selenium, phosphorus, B1, B6, B12, C, D, and K vitamins, as well as their father’s quantities, were all inadequate.(19) To assess the maternal coronary artery disease adaptations to pregnancy in women who have had prior weight loss operations to those who have not, in terms of the BMI during pregnancy of young age, and racial.(20)
METHOD
An examination of pregnant patients who had gastric bypass, sleeve gastrectomy, banding, or any form of bariatric surgery is included in the data collection. The dataset comprises 507 people for deliveries made after bariatric surgeries and 301 participants for deliveries made prior to bariatric surgeries. In addition to clinical and demographic information including age, pre-surgery BMI, pregnancy weight, fetal age, parity, and gravidity, each patient is individually recognized by a shared set of parameters known as a Patient ID. Anaemia, hypertension, gestational diabetes, and cases of macrosomia were among the important obstetric outcomes that were evaluated. Deliveries techniques and neonatal outcomes were also documented, including newborn mortality and Apgar ratings at one and five minutes after birth. This extensive dataset makes it easier to examine the obstetric risks and outcomes related to bariatric surgery in detail, which adds important knowledge on the health of mothers and newborns in this demographic. To conduct the statistical analysis, Statistical Package for the Social Sciences (SPSS) version 12.0 was used.
RESULTS
Time Points, Type of Surgery and Gender
Three outcome criteria were considered for the purposes of the study. In patients treated for Roux-en-Y Gastric Bypass (RYGB) and Specialist Group (SG) procedures, as well as in patients who were male and female, compared the averages of water retention (WR), excess weight loss (EWL), and total weight loss (TWL) over the course of the observation period. A comparison of the TWL, WR, and EWL indicative values for each of the six research phases. Figures 1 a–b, c–d, and e–f illustrates how comparable the comparisons are for %EWL, %TWL, and %WR.
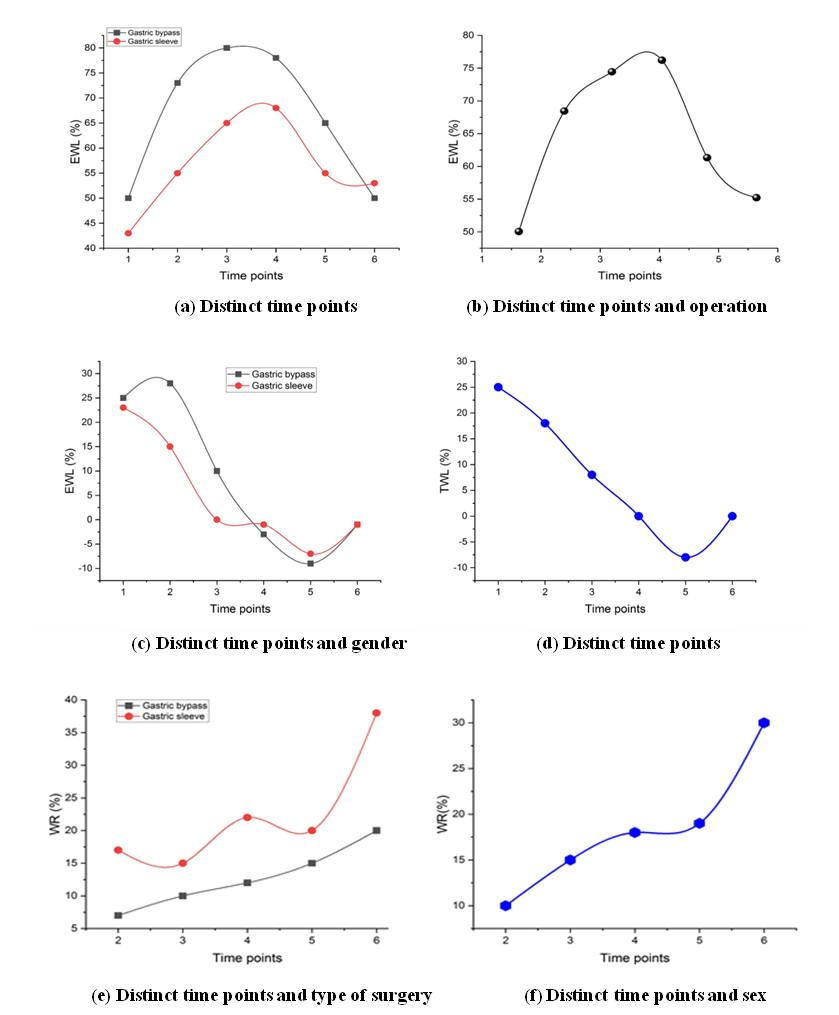
Figure 1. Implementation of Nanoparticles in Growth Factor Therapy
Maternal age was older and there was more parity and gravidity in post-bariatric surgery pregnancies (table 1). Those who gave birth following bariatric surgery reported significantly greater rates of prior cesarean deliveries compared to those who gave birth before surgery. Obesity rates Pregestational diabetes mellitus and pre-pregnancy BMI were dramatically decreased following bariatric surgery. The majority of the population was made up of mothers. Figure 2 shows the outcome of Gravidity and Parity.
|
Table 1. Clinical characteristics of post-bariatric surgery and pre-bariatric surgery mothers who delivered |
|||
|
Features |
Deliveries after bariatric surgical procedure |
Deliveries before bariatric surgical procedure |
P-value |
|
|
(n=507) |
(n=301) |
|
|
Gravidity |
|
|
b0,001 |
|
1 |
21,2 |
43,2 |
1 |
|
2–4 |
66,5 |
51,8 |
2–4 |
|
≥5 |
8,3 |
5,0 |
≥5 |
|
Maternal age, y |
32,3±5,1 |
26,5±4,4 |
b0,001 |
|
age, wk |
|
|
|
|
Gestational |
38,7±2,4 |
38,9±2,5 |
0,14 |
|
Previous cesarean |
20,1 |
7,6 |
b0,001 |
|
delivery |
|
|
|
|
Obesityb |
9,5 |
19,6 |
b0,001 |
|
Pregestational diabetes |
2,4 |
5,6 |
0,014 |
|
Parity |
|
|
b0,001 |
|
1 |
18,5 |
36,9 |
|
|
2–4 |
60,0 |
55,8 |
|
|
≥5 |
21,5 |
14,3 |
|
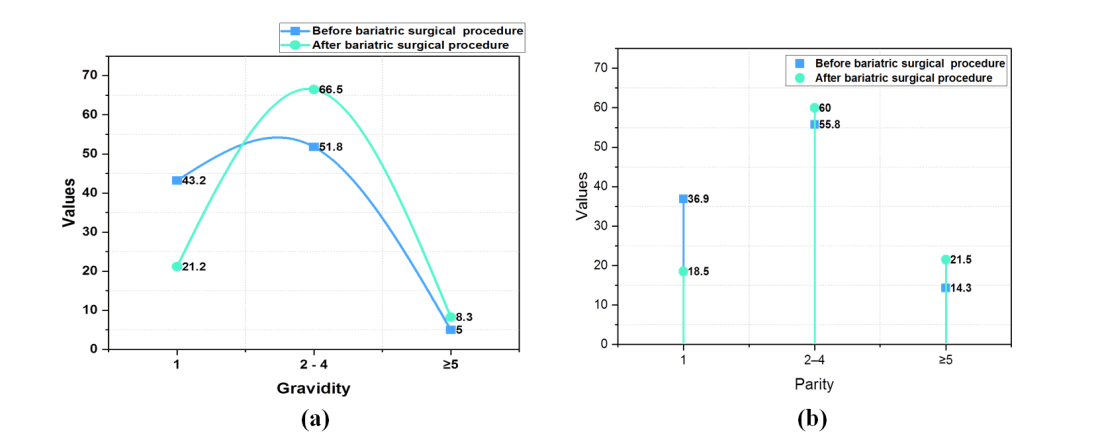
Figure 2. Outcome of (a) Gravidity and (b) Parity
Table 2 lists the perinatal problems and gestational risk factors for individuals who gave birth before and after surgery to lose weight. Figure 3 shows the effects of bariatric surgery on women’s chances of getting pregnant and dealing with postpartum complications. After weight loss operation, there were considerably decreased rates of prenatal hemoglobin in the range of 10 g/dL is considered anemic and diabetes mellitus, as well as reduced prevalence of serious forms of pre- and overall hypertension in specific. In comparison to deliveries that took place prior to the surgery, there was a tendency increasing frequency of delivery misrepresentations that took place after the surgery. No in relation to limitations to intrauterine growth, repeat abortion, pregnancy-related diabetes, placental abruption, early tear of the membrane, and egg donation with each group, systematically significant variation were discovered.
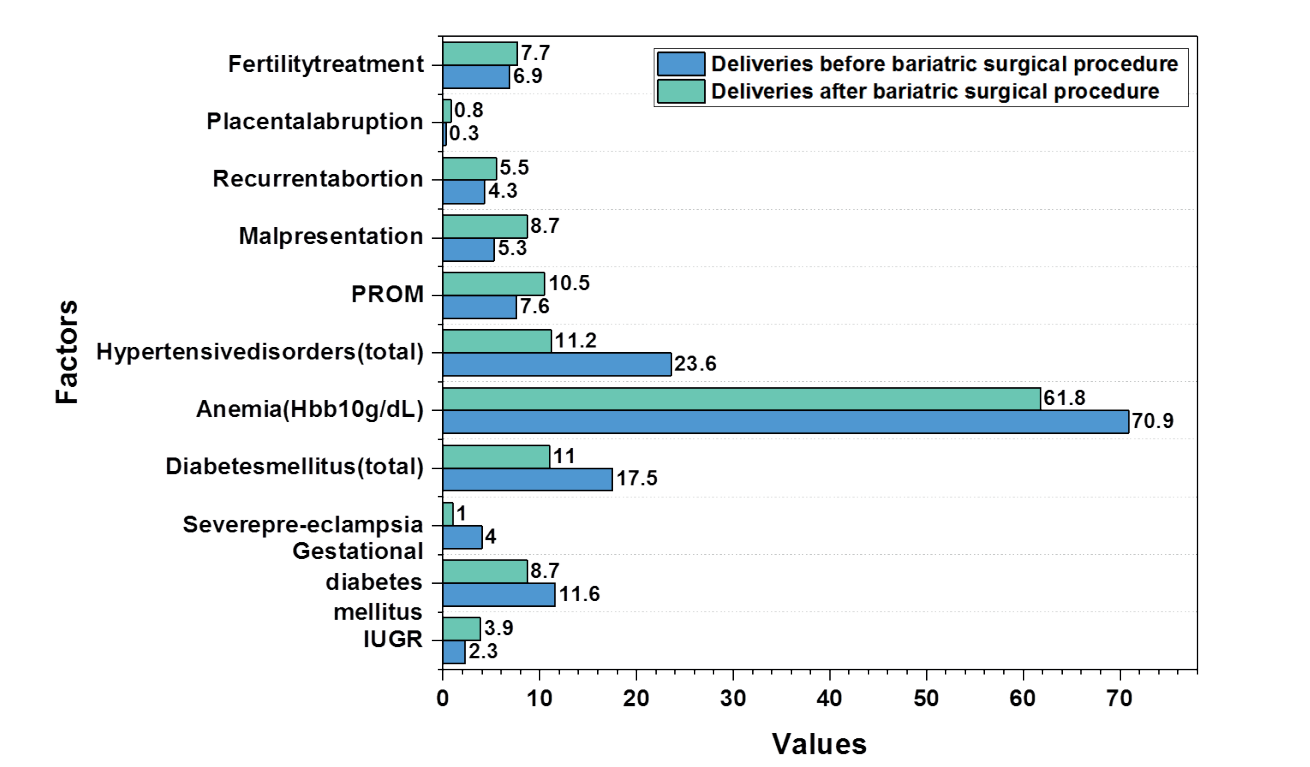
Figure 3. Effects of bariatric surgery on women’s chances of getting pregnant and dealing with postpartum complications
|
Table 2. Risk factors during pregnancy and postpartum issues in women who gave birth prior to and following bariatric surgery. |
|||
|
Factors |
95 %CI |
OR |
P -value |
|
IUGR |
0,7–4,1 |
1,7 |
0,15 |
|
Severe pre-eclampsia |
0,1–0,7 |
0,2 |
0,005 |
|
Diabetes mellitus(total) |
0,4–0,9 |
0,6 |
0,009 |
|
Anemia (Hbb10g/dL) |
0,5–0,9 |
0,7 |
0,014 |
|
Gestational diabetes mellitus |
0,5–1,2 |
0,7 |
0,11 |
|
Hypertensive disorders(total) |
0,3–0,6 |
0,4 |
b 0,001 |
|
PROM |
0,8–2,4 |
1,4 |
0,11 |
|
Malpresentation |
0,9–3,1 |
1,7 |
0,056 |
|
Recurrent abortion |
0,7–2,5 |
1,3 |
0,28 |
|
Placental abruption |
0,3–21,4 |
2,4 |
0,39 |
|
Fertility treatment |
0,6–1,9 |
1,1 |
0,38 |
Table 3 and figure 4 details the results of pregnancy as well as delivery for patients who gave birth both before and after having a bariatric procedure. In deliveries that took place after bariatric surgery, the average infant pregnancy weight was substantially lower, and reduced incidence elevated for pregnancies infants (4000 g and greater birth weights) were observed. However, after surgery to lose weight, rates of C-sections and foetal abnormalities considerably increased. The Mantel-Haenszel test was used to adjust for past cesarean deliveries, and Numbers of C-section births were no longer significant. Small apgar values at 1 and 5 seconds, low birth weights, and perinatal morbidity rates were slightly distinct from one another amongst the groups.
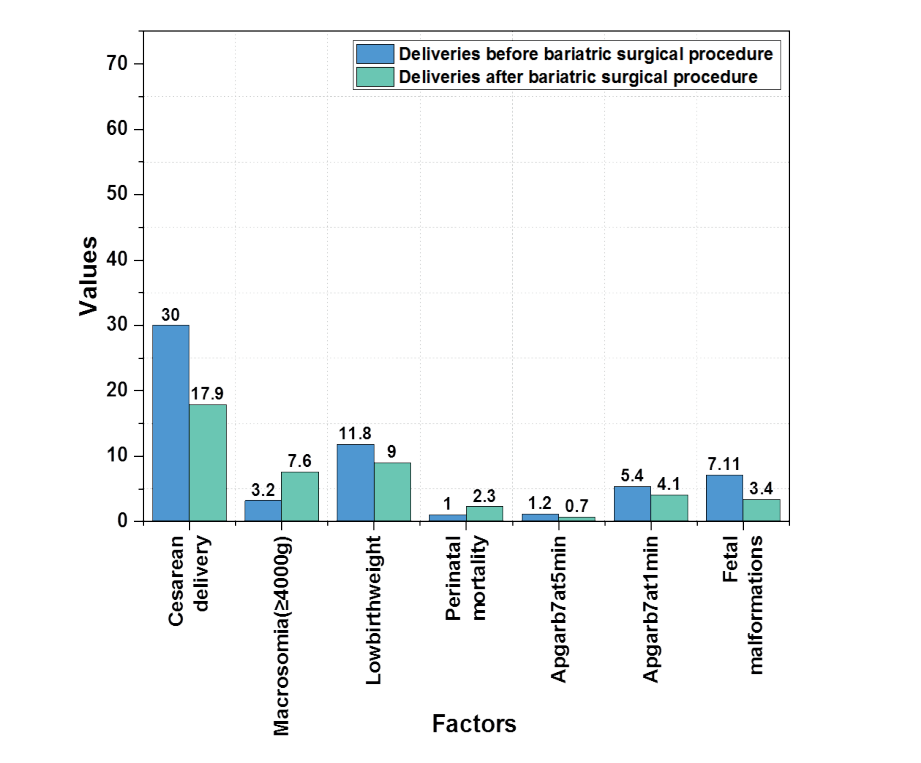
Figure 4. Outcomes of Maternity and delivery results comparing in before and after
|
Table 3. Maternity and delivery results comparing women who had bariatric surgery |
|||
|
Factors |
95 %CI |
OR |
P value |
|
Cesarean delivery |
1,4–2,8 |
1,9 |
b0,001 |
|
Macrosomia(≥4000g) |
0,2–0,8 |
0,4 |
0,004 |
|
Low birth weight |
0,8–2,2 |
1,4 |
0,12 |
|
Perinatal mortality |
0,1–1,3 |
0,4 |
0,11 |
|
Apgarb7at5min |
0,4–8,9 |
1,8 |
0,38 |
|
Apgarb7at1min |
0,7–2,7 |
1,3 |
0,25 |
|
Fetal malformations |
1,2–5,1 |
2,7 |
0,006 |
The rates of obesity Deliveries that had undergone bariatric surgery had a considerably higher caesarean delivery rate. Table 4 lists the reasons for a caesarean delivery in both groups. Before bariatric surgery, there was a noticeable decrease in the need for a caesarean delivery to fetal macrosomia, and there were no incidences of subsequent dystocia. The main reason for repeated caesarean deliveries for individuals after bariatric surgery. There were no reported incidences of placental previa. There was no distinction that is significantly different among the two categories for any other reasons for having a caesarean delivery. Figure 5 shows the outcome of pre and post-bariatric surgery indications for caesarean deliveries.
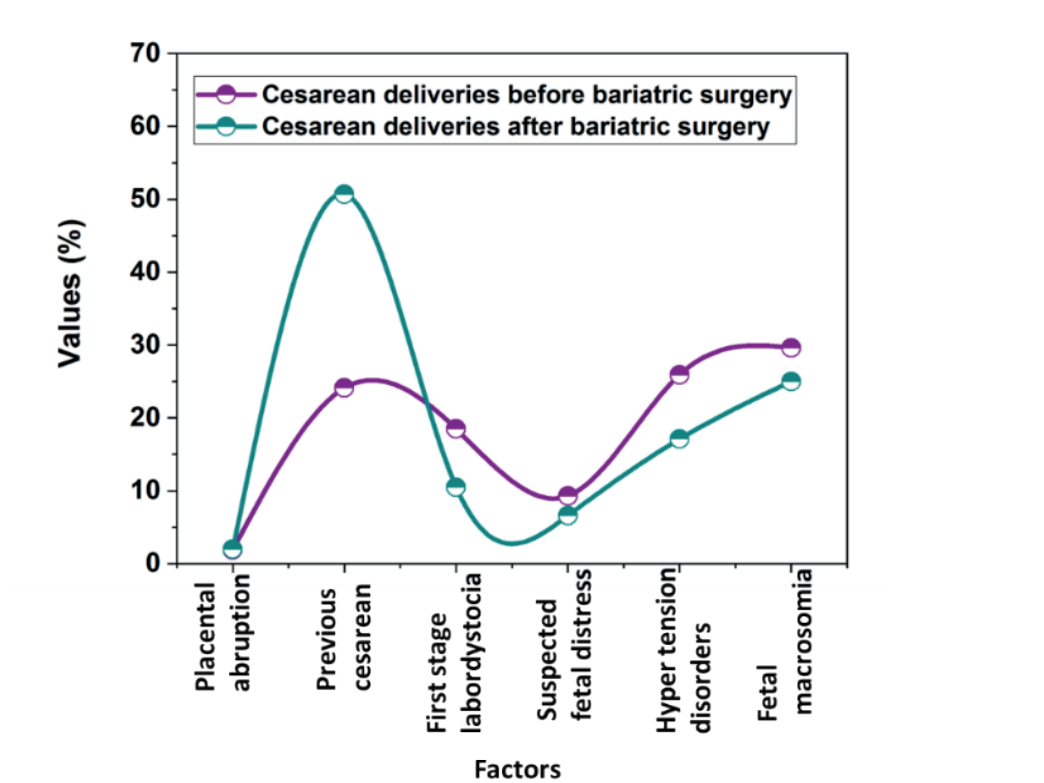
Figure 5. Outcome of pre and post-bariatric surgery indications for caesarean deliveries
|
Table 4. Pre and post-bariatric surgery indications for caesarean deliveries |
|||
|
Factors for cesarean deliveryb |
OR |
95 %CI |
P value |
|
Placental abruption |
1,0 |
0,1–10,5 |
0,72 |
|
Previous cesarean |
3,24 |
1,6–6,5 |
0,001 |
|
First stage labordystocia |
0,5 |
0,2–1,2 |
0,10 |
|
Suspected fetal distress |
0,7 |
0,2–2,1 |
0,35 |
|
Hyper tension disorders |
0,6 |
0,3–1,2 |
0,11 |
|
Fetal macrosomia |
0,24 |
0,08–0,72 |
0,011 |
Fetal abnormalities were used as the outcome variable in a new multivariate evaluation because were significantly more frequent in babies born following bariatric surgery than in babies born before that procedure. The model took into account potential confounders such mother age, obesity, and birth weight. The prevalence of foetal abnormalities was shown to be greater in pre- and post-bariatric surgery babies, however this trend was not statistically significant. Table 5 shows that there is no proof that bariatric surgery increases the incidence of fetal abnormalities. Next to weight loss surgery, a multivariate experiment with the following variables revealed that the following conditions were significantly reduced reversed elimination. Diabetes mellitus, hypertension, and fetal macrosomia.
|
Table 5. Decrease in prenatal problems that is independently correlated with the status of bariatric surgery |
|||
|
Features |
95 %CI |
OR |
P value |
|
Preterm delivery |
2,75–12,7 |
5,9 |
b0,001 |
|
Bariatric surgery |
0,88–4,12 |
1,9 |
0,089 |
|
Maternal age |
1,00–1,13 |
1,07 |
0,037 |
DISCUSSION
The goal of the current study was to determine the significance of weight loss in lowering obese women’s risk of medical and obstetric problems. The study focused on a sizable cohort and investigated some of the negative consequences and prenatal problems linked to overweight mothers. According to the current study, compared to pregnancy that occurred before the surgery hypertension rates diseases, diabetes mellitus, and fetal macrosomia were significantly lower in pregnancy that followed the procedure. Obesity surgery is a rapidly expanding topic of current surgery practice. This industry’s explosive expansion is a result of both the development of safer, less intrusive treatments and the efficacy of bariatric surgery to produce significant and long-lasting weight loss. With the help of restrictive or malabsorptive therapy, bariatric surgery aims to limit calorie consumption. The most popular methods are the duodenum diverting of the bile Change (a few malabsorptive and restricted), endoscopic variable gastric band (restrictive only), and Pancreatic bypass surgery (restrictive and occasionally malabsorptive).
There is a lack of information regarding the likelihood of becoming pregnant after various forms of bariatric surgery. Numerous health advantages are seen after significant weight loss. The most notable effects of bariatric surgery are undoubtedly changes in quality of life (QOL), mental health, and illnesses associated with obesity. Significant weight loss results in full or limited command over typical dangerous disorders such Diabetes, high blood pressure, and coronary heart disease in very obese people. Following bariatric surgery, severe medical comorbidities that came along with the weight loss have been reported to dramatically improve or disappear. It is probable that the decline in primigravida’s (44,2 % vs 25,3 %), a condition considered to be a risk factor for prenatal hypertension illness, could be reflected in a reduction in pregnancy-related hypertension after weight loss surgery. However, older a different is aged mother established chance element for prenatal hypertensive morbidity, was present in pregnancies after the operation.
Following bariatric surgery, the rate of hypertensive disorders was considerably lower using a multivariate approach that controlled for potential variables. The findings are consistent with those of other research done on both pregnant and non-pregnant patients. Additionally, after having bariatric surgery, obesity rates dramatically decreased, demonstrating the relative efficacy of the operation. Tragically, weight increase information is not available in database. The metabolism disorder’s symptoms, which include hypertension, epidemically, and poor glucose tolerance, have significantly improved in non-pregnant patients.
Improvements pancreas beta-cell resistance and response to insulin activity linked to weight loss, according to, cause the majority of type 2 diabetics to go into remission and lower the likelihood of others developing the disease. Recovery in atherosclerosis is characterized by higher concentrations of HDL cholesterol and decreased triglyceride levels. These adjustments not only lower blood pressure, but also significantly lower the risk of cardiovascular disease. Significant improvements have also been made in various medical diseases brought on by or made worse by obesity, including sleep apnea, excessive daytime fatigue, allergies, or acid reflux. In fact, many Following bariatric surgery, pregnancies show improved health. The results among female patients with LAGB (laparoscopic adjustable gastric banding) for the management of severe obesity in terms of pregnancy and perinatal outcomes. The discovered that during pregnancy and delivery, LAGB is safe for both the mother and the baby. Team analyzed all pregnancies among individuals with and without prior obesity surgeries in a based-on populations analysis.
Pregnancy-related issues included poor Apgar ratings at one and five minutes, placental abruption, placenta previa, and labour dystocia, watery discharge-stained pregnancy fluid, neonatal mortality, congenital defects, and no discernible variations between the groups. However, it was discovered that bariatric surgery was a standalone risk factor for a cesarean delivery. Moreover, prior weight loss surgery was not linked to a poor perinatal outcome even in patients with pregnancy-related diabetes mellitus. Regarding the link between obesity and birth defects, there is debate. Examined, using an epidemiological situation-control study design, the relationship between various birth abnormalities and obesity. Women who are overweight (BMI 24,0-28,4) are at risk. and obese women (BMI 30) were contrasted with those for women of medium weight (BMI 18,5-24,9).
CONCLUSION
In this research conclude a strong link between fat and fetal abnormalities. Even after accounting for pregnancy diabetes, studies looking at perinatal outcomes after bariatric surgery have not discovered an important distinction among the groups for congenital abnormalities. Patients who have undergone bariatric surgery frequently subsequently have aberrant vitamin and trace mineral readings; this impact is especially pronounced after malabsorptive surgeries. This might make deadly congenital abnormalities more likely to occur. Congenital abnormalities were found to be substantially more common in the current study in deliveries that took place after bariatric surgery than in those who did not, post bariatric people undergoing operations were strongly a bit older and the link disappeared after this crucial feature was taken into account in a multivariate model with fetal abnormalities as the end variable (OR 1,9, 95 % CI 0,88-4,1; P=0,089). This can be a sign of the surgical intervention’s relative success. The study’s main strength is that looked at a sizable cohort of births. It took place in one location, the only hospital in served the entire local maternity population. As a result, the study uses insensitive data. In conclusion, after having bariatric surgery, it is possible to reduce fetal macrosomia as well as maternal problems including diabetes mellitus and hypertension. Bariatric surgery is also not a standalone danger element for poor pregnancy results. Following bariatric surgery, the weight regain is a significant problem, and long-term monitoring is necessary to make most out of this prevention.
REFERENCE
1. Belogolovkin V, Salihu HM, Weldeselasse H, Biroscak BJ, August EM, Mbah AK, Alio AP. Impact of prior bariatric surgery on maternal and fetal outcomes among obese and non-obese mothers. Archives of gynecology and obstetrics. 2012 May;285:1211-8. https://doi.org/10.1007/s00404-011-2134-0
2. Kjaer MM, Nilas L. Pregnancy after bariatric surgery–a review of benefits and risks. Acta obstetricia et gynecologica Scandinavica. 2013 Mar;92(3):264-71. https://doi.org/10.1111/aogs.12035
3. González I, Rubio MA, Cordido F, Bretón I, Morales MJ, Vilarrasa N, Monereo S, Lecube A, Caixàs A, Vinagre I, Goday A. Maternal and perinatal outcomes after bariatric surgery: a Spanish multicenter study. Obesity surgery. 2015 Mar;25:436-42. https://doi.org/10.1007/s11695-014-1387-7
4. Guthrie TM, Dix CF, Truby H, Kumar S, de Jersey SJ. A Systematic Review Investigating Maternal Nutrition During Pregnancy After Bariatric Surgery. Obesity Surgery. 2023 Jun;33(6):1857-65. https://doi.org/10.1007/s11695-023-06565-8
5. Yu Y, Ma Q, Hollenbach S, Zhu Y, Groth S. Pregnant Women Following Bariatric Surgery: A Focus on Maternal Mental Health and Its Impact on Birth Outcomes. Obesity Surgery. 2022 Nov;32(11):3696-704. https://doi.org/10.1007/s11695-022-06283-7
6. Snoek K, van de Woestijne N, Willemsen S, Klaassen R, Galjaard S, Laven J, Steegers-Theunissen R, Schoenmakers S. The impact of preconception gastric bypass surgery on maternal micronutrient status before and during pregnancy: a retrospective cohort study in the Netherlands between 2009 and 2019. Nutrients. 2022 Feb 9;14(4):736. https://doi.org/10.3390/nu14040736
7. Grandfils S, Demondion D, Kyheng M, Duhamel A, Lorio E, Pattou F, Deruelle P. Impact of gestational weight gain on perinatal outcomes after a bariatric surgery. Journal of Gynecology Obstetrics and Human Reproduction. 2019 Jun 1;48(6):401-5. https://doi.org/10.1016/j.jogoh.2019.03.001
8. Burlina S, Dalfrà MG, Lapolla A. Pregnancy after bariatric surgery: Nutrition recommendations and glucose homeostasis: A point of view on unresolved questions. Nutrients. 2023 Mar 1;15(5):1244. https://doi.org/10.3390/nu15051244
9. Baharuddin DM, Payus AO, Fahmy EH, Sawatan W, Than WW, Abdelhafez MM, Leik NK, Daud DM, Daud MN, Ahmad ZN. Bariatric surgery and its impact on fertility, pregnancy and its outcome: A narrative review. Annals of Medicine and Surgery. 2021 Dec 1;72:103038. https://doi.org/10.1016/j.amsu.2021.103038
10. Snoek KM, Steegers-Theunissen RP, Hazebroek EJ, Willemsen SP, Galjaard S, Laven JS, Schoenmakers S. The effects of bariatric surgery on periconception maternal health: a systematic review and meta-analysis. Human Reproduction Update. 2021 Nov 1;27(6):1030-55. https://doi.org/10.1093/humupd/dmab022
11. Kwong W, Tomlinson G, Feig DS. Maternal and neonatal outcomes after bariatric surgery; a systematic review and meta-analysis: do the benefits outweigh the risks?. American journal of obstetrics and gynecology. 2018 Jun 1;218(6):573-80. https://doi.org/10.1016/j.ajog.2018.02.003
12. Edison E, Whyte M, van Vlymen J, Jones S, Gatenby P, de Lusignan S, Shawe J. Bariatric surgery in obese women of reproductive age improves conditions that underlie fertility and pregnancy outcomes: retrospective cohort study of UK National Bariatric Surgery Registry (NBSR). Obesity surgery. 2016 Dec;26:2837-42. https://doi.org/10.1007/s11695-016-2202-4
13. Alamri SH, Abdeen GN. Maternal nutritional status and pregnancy outcomes post-bariatric surgery. Obesity Surgery. 2022 Apr;32(4):1325-40. https://doi.org/10.1007/s11695-021-05822-y
14. Al-Nimr RI, Hakeem R, Moreschi JM, Gallo S, McDermid JM, Pari-Keener M, Stahnke B, Papoutsakis C, Handu D, Cheng FW. Effects of bariatric surgery on maternal and infant outcomes of pregnancy—an evidence analysis center systematic review. Journal of the Academy of Nutrition and Dietetics. 2019 Nov 1;119(11):1921-43. https://doi.org/10.1016/j.jand.2019.02.008
15. Karmon A, Sheiner E. Timing of gestation after bariatric surgery: should women delay pregnancy for at least 1 postoperative year?. American journal of perinatology. 2008 May;25(06):331-3. https://doi.org/10.1055/s-2008-1078760
16. Getahun D, Fassett MJ, Jacobsen SJ, Sacks DA, Murali SB, Peltier MR, Mulugeta W, Chiu VY, Wing DA, Coleman KJ. Perinatal outcomes after bariatric surgery. American Journal of Obstetrics and Gynecology. 2022 Jan 1;226(1):121-e1. https://doi.org/10.1016/j.ajog.2021.06.087
17. Rottenstreich A, Elazary R, Goldenshluger A, Pikarsky AJ, Elchalal U, Ben-Porat T. Maternal nutritional status and related pregnancy outcomes following bariatric surgery: a systematic review. Surgery for obesity and related diseases. 2019 Feb 1;15(2):324-32. https://doi.org/10.1016/j.soard.2018.11.018
18. Patel D, Borrelli N, Patey O, Avesani M, Johnson MR, Di Salvo G, Savvidou MD. Maternal cardiovascular adaptation to pregnancy in women with previous bariatric surgery. American Journal of Obstetrics and Gynecology. 2022 Mar 1;226(3):409-e1. https://doi.org/10.1016/j.ajog.2021.08.052
19. Cornthwaite K, Prajapati C, Lenguerrand E, Knight M, Blencowe N, Johnson A, Draycott T, Siassakos D. Pregnancy outcomes following different types of bariatric surgery: a national cohort study. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2021 May 1;260:10-7. https://doi.org/10.1016/j.ejogrb.2021.02.031
20. Rehni AK, Singh TG, Kakkar T, Arora S. Involvement of src-kinase activation in ischemic preconditioning induced protection of mouse brain. Life sciences. 2011 May 9;88(19-20):825-9. https://doi.org/10.1016/j.lfs.2011.02.024
FINANCING
None.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Research: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Methodology: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Project management: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Resources: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Software: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Supervision: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Validation: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Display: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Drafting - original draft: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.
Writing - proofreading and editing: Jagmeet Sohal, RenukaJyothi S, Dhairyasheel D. Patil, Sameer Rastogi, Ravindra, Suvendu Narayan Mishra, Nittin Sharma.