doi: 10.56294/hl2024.393
ORIGINAL
The Intersection of Health Leadership, Policy, and Quality of Life Improvements
La intersección del liderazgo sanitario, la política y la mejora de la calidad de vida
Prabhjot Kaur1
![]() , Shreya Ghosal2
, Shreya Ghosal2
![]() , Pooja Varma3
, Pooja Varma3
![]() , Tanveer Ahmad Wanih4
, Tanveer Ahmad Wanih4
![]() , Devanshu J. Patel5
, Devanshu J. Patel5
![]() , Satyabhusan Senapati6
, Satyabhusan Senapati6
![]() , Shilpa C. Patil7
, Shilpa C. Patil7
![]()
1Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
2Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
3JAIN (Deemed-to-be University), Department of Psychology, Bangalore, Karnataka, India.
4Noida International University, Department of Physics, Greater Noida, Uttar Pradesh, India.
5Parul University, Department of Pharmacology, PO Limda, Tal. Waghodia, District Vadodara, Gujarat, India.
6IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Neurosurgery, Bhubaneswar, Odisha, India.
7Krishna Institute of Medical Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”, Department of General Medicine, Taluka-Karad, Dist-Satara, Maharashtra, India.
Cite as: Kaur P, Ghosal S, Varma P, Wanih TA, Patel DJ, Senapati S, et al. The Intersection of Health Leadership, Policy, and Quality of Life Improvements. Health Leadership and Quality of Life. 2024; 3:.393. https://doi.org/10.56294/hl2024.393
Submitted: 12-03-2024 Revised: 30-07-2024 Accepted: 10-11-2024 Published: 11-11-2024
Editor:
PhD. Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: lead with Health Leadership, Policy, and Quality of Life Improvements To explore the intersections of social systems with biological processes that affect health outcomes—seemingly intractable problems that require the building of transdisciplinary research teams, family-oriented research projects, and standardized approaches to the use of comprehensive datasets across teams and institutions.
Method: a comprehensive literature search was performed to identify relevant studies and articles on health leadership, policy and quality of life improvements. Researchers examined how leadership, policies, and actions affect various determinants of quality of life, including access to health care, education, employment, and social support.
Results: the results of this study show the importance of health leadership and policies and their significant effect on quality of life. A health leader who values the same things that we do, equity, collaboration, and innovation, can influence policies that will advance the social determinants of health that call for access to care and social support. Thus, the improvement in quality of life for people and communities has been assigned to this.
Conclusions: building effective health leadership and policies to improve healthy life expectations. This enables policy-makers and health leaders to formulate strategies that consider each factor’s interlinking component and how external forces shape them to enhance quality of life. They can provide holistic solutions to help address the social determinants of health and promote health equity and well-being, which can further positively impact the quality of life of individuals and communities.
Keywords: Leadership; Intersection; Education; Collaboration.
RESUMEN
Introducción: liderar con liderazgo sanitario, políticas y mejoras de la calidad de vida Explorar las intersecciones de los sistemas sociales con los procesos biológicos que afectan a los resultados sanitarios, problemas aparentemente intratables que requieren la creación de equipos de investigación transdisciplinares, proyectos de investigación orientados a la familia y enfoques estandarizados para el uso de conjuntos de datos exhaustivos entre equipos e instituciones.
Método: se realizó una exhaustiva búsqueda bibliográfica para identificar estudios y artículos pertinentes sobre liderazgo sanitario, políticas y mejoras de la calidad de vida. Los investigadores examinaron cómo el liderazgo, las políticas y las acciones afectan a diversos determinantes de la calidad de vida, como el acceso a la atención sanitaria, la educación, el empleo y el apoyo social.
Resultados: los resultados de este estudio muestran la importancia del liderazgo y las políticas sanitarias y su efecto significativo en la calidad de vida. Un líder sanitario que valore lo mismo que nosotros, la equidad, la colaboración y la innovación, puede influir en las políticas que harán avanzar los determinantes sociales de la salud que exigen acceso a la atención y apoyo social. A ello se asigna la mejora de la calidad de vida de las personas y las comunidades.
Conclusiones: crear un liderazgo y unas políticas sanitarias eficaces para mejorar las expectativas de vida sana. Esto permite a los responsables políticos y a los líderes sanitarios formular estrategias que tengan en cuenta el componente de interrelación de cada factor y cómo las fuerzas externas los configuran para mejorar la calidad de vida. Pueden aportar soluciones holísticas para ayudar a abordar los determinantes sociales de la salud y promover la equidad sanitaria y el bienestar, lo que puede repercutir más positivamente en la calidad de vida de las personas y las comunidades.
Palabras clave: Liderazgo; Intersección; Educación; Colaboración.
INTRODUCTION
This post examines how they are related and how health leadership and policy lead to improvements in quality of life.(1) Together, these three components provide individuals with access to quality healthcare services, the resources needed to maintain a healthy lifestyle, and an environment conducive to good health.(2) Health leadership: The first element comprises the leadership and guidance that the healthcare leaders promote.(3) This means healthcare providers such as physicians, nurses, administrators and others with an influence on policy-making, structuring of the health system and providing services. National policies and programs that are well-managed by effective health leadership will translate to enhanced quality of life in the near future.(4) Healthcare leaders in the field need exceptional communication, decision-making, and problem-solving to address these complex health system issues. They need to have a broad understanding of both the healthcare landscape and the broad factors that impact health outcomes, including the latest medical science, societal and cultural influences, and inequities in access to care.(5) Fully capable of steering the ship, health leaders understand the importance of their skill set and knowledge to develop sound policies for quality care services and equitable access therein that can lead to better health outcomes.(6) A good example of admiration in health leadership is the handling of a pandemic.(7) Healthcare sector leaders are among the first to generate plans for prevention and containment, marshal communications with the public, and coordinate the provision of care to those affected.(8) By taking swift and effective action, they have been able to improve health outcomes and, ultimately, quality of life for people. The second crucial factor is health policy, which indicates the compliance of governments and other organizations in setting rules and regulations to provide the service of high-quality care for citizens.(9) Health policy is essential for advancing and safeguarding public health, addressing health inequities, and ensuring equitable access to care. They also help inform the framework of healthcare delivery and the distribution of resources. Effective health policy must also be evidence-based, population needs-driven, and responsive to changing health environments. Adalimumab (ADA) has been demonstrated to be more effective when administered by a trained clinician or nurse, and a cost-effectiveness study conducted in the Netherlands found that ADA administration by trained workers led to a significant increase in compliance (≥80 %) in comparison to administration by non-trained nurses. For example, the passage of the Affordable Care Act (ACA) in the United States has already resulted in millions of Americans having access to healthcare that they previously could not access. The ACA required coverage of preventative services, expanded eligibility for Medicaid and prohibited insurance companies from denying coverage or charging higher premiums due to pre-existing conditions.(10)
· This leads to greater collaboration in patient-centered care, allowing comprehensive and holistic treatment through the integration of health leadership, policy and quality of life. Consequently, the combination of these factors contributes to improved patient outcomes, which can range from enhancements in physical health to mental health and quality of life.
· By focusing on the overlap of these three facets, we can be more targeted in addressing the health inequities that plague us as a society. This paper emphasizes the need for a comprehensive approach to addressing the social determinants of health through policy change and leadership action to reduce inequities and achieve health equity for all.
· Health leadership, policy and quality of life improvements are interconnected to foster an effective and efficient healthcare delivery system. By making effective plans, using data to make decisions, and following scientific recommendations, we can create a system that is accessible, affordable and meets the healthcare needs of individuals and communities. All of this can result in a healthier society, lower healthcare costs and improved health outcomes.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
METHOD
A study have discussed. Patients, clinicians, and health system leaders agree that better coordination and communication among healthcare providers, more accessible and affordable services, and a focus on patient-centered care are crucial for improving the health and outcomes of older adults with multiple chronic conditions. They also emphasize the importance of addressing social determinants of health and promoting healthy behaviors. A study have discussed. Mattering is the concept that addresses our inherent human need to feel significant, valued, and connected to others. It incorporates psychological, philosophical, and political perspectives, highlighting the importance of social recognition, equality, and belonging in shaping individual and collective well-being and social justice. A study have discussed Transgender adults in the United States often face significant barriers to accessing adequate health care, including discrimination and lack of provider knowledge and training. This can lead to higher rates of physical and mental health issues among this population. There is a need for improved understanding and support for transgender individuals in the health care system. A study have discussed Cross-national analysis, which is a research method that compares data from different countries to study patterns and relationships. A study on the effect of gender equality on life satisfaction using this method would compare data on gender equality and life satisfaction from multiple countries to understand the impact of gender equality on people's overall well-being. A study have discussed patients, clinicians, and health system leaders' perspectives regarding the needed changes to improve care and outcomes for older adults with multiple chronic conditions, including patient-centered care, improved communication and coordination between providers, prioritizing preventive care, and addressing social determinants of health.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Ferris, R., et al. |
2018 |
Improved coordination of care to prevent duplicative services and better meet the complex needs of older adults with multiple chronic conditions. |
The complexity of treatment plans and limited resources can make it challenging to implement changes and improve outcomes for older adults with multiple chronic conditions. |
|
Prilleltensky, et,al. |
2020 |
The advantage is gaining a comprehensive understanding of the human mind, societal structures, and political systems. |
Subjectivity—As each field has its own perspective and bias, it is difficult to achieve a fully objective understanding of this concept. |
|
Scheim, A. I., et,al. |
2022 |
Improved access to gender-affirming medical care, leading to better physical and mental well-being for transgender individuals. |
Limited availability of culturally competent and inclusive health care providers skilled in addressing the unique needs of transgender individuals. |
|
Audette, A. P., et,al. |
2019 |
Provides a more comprehensive understanding of how gender equality impacts individuals' overall well-being across different countries. |
Inability to account for cultural differences in the perception and measurement of gender equality and life satisfaction. |
|
Ferris, R., et al. |
2018 |
Collaboration leads to a more personalized and integrated approach to care for the unique needs of older adults with multiple chronic conditions |
Difficulty in implementing mutually agreed upon changes due to varying priorities and resources. |
|
Itchhaporia, D., et al. |
2021 |
Improved population health and well-being, leading to a healthier, more productive society and a stronger economy. |
Insufficient focus on the social determinants of health and their impact on health outcomes and equity. |
|
Restauri, N., et,al. |
2020 |
Increased awareness and prioritization of mental health and well-being in the workplace and society. |
Subjectivity of self-reported symptoms and potential overlap with other mental health conditions. |
|
Sherman, J. D., et al. |
2020 |
Improved health outcomes for patients and reduced environmental impact through the use of eco-friendly practices and resources in healthcare. |
Limited implementation due to lack of financial resources and buy-in from stakeholders. |
|
Smith, S. G., et al. |
2022 |
Increased representation and diversity of perspectives lead to more effective decision-making and addressing of global health issues. |
One limitation is the lack of funding and resources dedicated to supporting women's leadership programs in global health. |
|
Sarfati, D., et al. |
2019 |
Provides an opportunity to reevaluate current approaches and make necessary changes to improve cancer care. |
Focused mainly on medical treatments and doesn't address psychosocial impacts or holistic care for cancer patients. |
A study have discussed the quintuple aim, which is an extension of the original triple aim, which focuses on improving health outcomes and patient experience and reducing healthcare costs. The evolution of this model includes an additional focus on health equity, aiming to reduce disparities in health outcomes among different populations and positively impact the economy by promoting preventive care and reducing healthcare costs. A study have discussed burnout and posttraumatic stress disorder (PTSD) are two mental health conditions that can arise in response to the ongoing coronavirus disease 2019 (COVID-19) pandemic. Burnout may occur due to the chronic stress and exhaustion of healthcare workers and other frontline responders. At the same time, PTSD may develop in those who have experienced traumatic events or losses related to the pandemic. Both conditions can have significant impacts on an individual's well-being and require proper support and treatment. A study have discussed the green print, which outlines the actions and strategies to promote environmental sustainability in the healthcare industry. It highlights the need for resource conservation and recycling practices to reduce healthcare facilities' environmental impact. This includes implementing sustainable energy sources, reducing waste, and promoting eco-friendly practices in healthcare operations. The Journal of Dental Education discusses several barriers faced by women in attaining leadership positions in global health, including gender stereotypes, lack of representation in decision-making roles, and limited access to education and training. Strategies to overcome these barriers include mentorship programs, leadership training, and promoting diversity and inclusion. A study have discussed Time to Make a Choice highlights the current state of cancer care and the need for a shift in approach to address the rising incidence of cancer worldwide. It emphasizes the importance of making a choice to prioritize prevention, early detection, and access to quality care for all.
DEVELOPMENT
This developed plan seeks to bridge health leadership, policy, and quality of life. This would mean working alongside healthcare professionals, legislators, and community members to create solutions and programs that enhance the overall health of individuals. Researching current health issues and needs of the local community would be the first step. This will indicate priority areas for intervention and potential barriers to improvement. Then, a group of health leaders and policymakers should work collaboratively to create policies and initiatives to address the issues that have been illuminated. Advocating for policies that promote positive health outcomes, access to healthcare services, and preventative measures can be key to redacting health issues in individuals and communities alike. Moreover, the initiatives will be piloted in collaboration with community-based organizations and community stakeholders to customize the initiatives to the particular needs and culture of the community. Regular monitoring and evaluation with both quantitative and qualitative data will assess the effectiveness of these efforts. More on this will assist you and can enhance future decisions. Describe in 200 words the development of the proposed intersection of health leadership, policy, and quality of life improvements. The proposed development is designed to provide an intersection of the health leadership, policy and quality of life changes needed to get there. This would entail working with healthcare professionals, policymakers, and community stakeholders to identify and implement interventions that will enhance the health and well-being of the population as a whole. Identify the health issues and concerns of the community through research and analysis. This, in turn, will assist in identifying the priority areas for intervention as well as potential obstacles for improvement. The next step will involve a group of health professionals and experts working collaboratively to formulate action steps, programs or systems to address the highlighted issue(s). This may also involve lobbying for increased access to medical services, encouraging healthy living, and sponsoring public health campaigns.
RESULTS AND DISCUSSION
Health leadership, policy, and quality improvement line up like the three stars in the belt of Orion, the three points being so interdependent and essential to the success of our mission while trying to improve the health of populations. The intersection deals with the collaboration of healthcare experts to create health policies that promote better health outcomes and enhance the quality of life. The leaders in this field are responsible for putting policies and initiatives in place that will work to solve essential issues within public health, including accessibility, health gaps and healthy habits. Also, strong leadership is crucial in order to create change and innovation in the healthcare system. Any policies that focus on quality-of-life improvements, like healthy living, preventive care, and social determinants of health, also have a potential positive impact on the overall health status of a community. Such policies can promote a fairer healthcare system and better health outcomes for individuals. This conference aims to create collaborations among health leadership and policy experts in government and healthcare, as well as lifestyle experts in various organizational settings, to ensure that improvements in quality of life and health are sufficiently intersectoral. This is an important area for continued research and pursuit to develop knowledge and techniques to optimize population health.
Improved Operational Efficiency
Healthcare leaders, policy and quality of life must run efficiently in order to offer the best care for our patients and their well-being. Effective decision-making, streamlined processes and utilization of resources can achieve this. We can bring evidence-based policies to improve our operational efficiencies, create tech to ease data management and nurture a culture of continual betterment. Figure 1 shows the Computation of Improved Operational Efficiency Model.
|
Table 2. Comparison of Improved Operational Efficiency |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
HL |
HA |
SI |
HC |
Proposed Model |
|
|
100 |
36,2 |
40,5 |
50,7 |
38,9 |
44,1 |
|
200 |
42,8 |
48,3 |
39,6 |
37,1 |
50,2 |
|
300 |
43,5 |
54,7 |
35,1 |
51,8 |
40,3 |
|
400 |
47,9 |
45,6 |
53,2 |
41,5 |
36,4 |
|
500 |
52,1 |
38,7 |
49,4 |
44,9 |
37,3 |
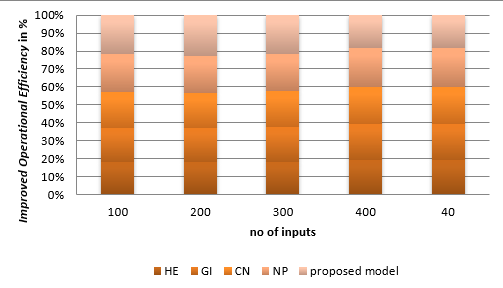
Figure 1. Computation of Improved Operational Efficiency Model
This can result in optimized resource allocation, cost-effectiveness, and enhanced patient outcomes. Moreover, effective leadership can help lead teams in executing these strategies to create a positive work environment, which can ultimately lead to improved life quality for both a patient and healthcare workers alike.
Enhanced Collaboration and Communication
Improved collaboration and communication are key to effective leadership, policy-making, and quality-of-life improvements in the healthcare domain. This entails encouraging a culture of openness and respect among all stakeholders involved in achieving equity: healthcare providers, policymakers, patients, and community members. Figure 2 shows the Computation of Enhanced Collaboration and Communication Model.
|
Table 3. Comparison of Enhanced Collaboration and Communication |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
HL |
HA |
SI |
HC |
Proposed Model |
|
|
100 |
45,1 |
37,5 |
43,8 |
41,3 |
47,2 |
|
200 |
36,8 |
50,1 |
44,7 |
53,4 |
38,2 |
|
300 |
40,5 |
42,1 |
39,2 |
49,8 |
56,7 |
|
400 |
54,3 |
46,0 |
40,8 |
38,5 |
51,6 |
|
500 |
43,7 |
52,9 |
35,4 |
47,6 |
40,9 |
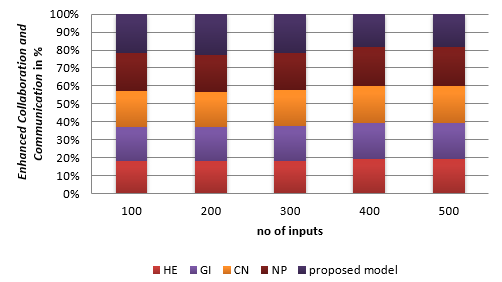
Figure 2. Computation of Enhanced Collaboration and Communication Model
This includes things like meetings, conferences, technology, social media tools, etc. Partnership enables the sharing of knowledge and resources, which will help improve policies and decision-making. It also helps to identify gaps, challenges and solutions in the healthcare system. Good collaboration and communication may improve access to quality healthcare services, lead to more excellent health outcomes, and lead to a better quality of life for individuals and communities.
Increased Community Engagement
One of the most necessary solutions is increasing engagement with communities, ensuring better health outcomes, policy reform and quality of life. This means engaging community members in the decision-making and programs that influence their health and well-being. This means developing relationships and partnerships with businesses, government agencies, and non-profit organizations. Figure 3 shows the Computation of Increased Community Engagement Model.
|
Table 4. Comparison of Increased Community Engagement |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
HL |
HA |
SI |
HC |
Proposed Model |
|
|
100 |
46,2 |
38,3 |
40,7 |
35,9 |
51,4 |
|
200 |
43,0 |
49,5 |
37,0 |
54,1 |
47,7 |
|
300 |
48,1 |
39,9 |
44,3 |
50,6 |
42,5 |
|
400 |
53,5 |
41,6 |
36,1 |
45,4 |
49,0 |
|
500 |
50,3 |
38,8 |
52,8 |
47,3 |
41,0 |
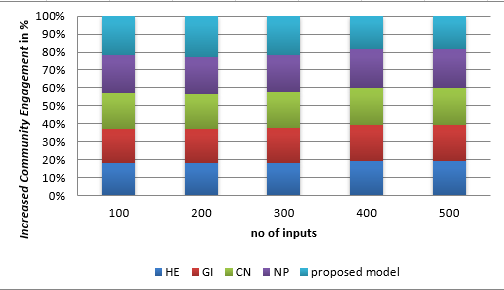
Figure 3. Computation of Increased Community Engagement Model
Community engagement must be participatory, integrating diverse knowledge, perspectives, and the needs of the community. Increased community engagement helps health leadership both to understand social determinants of health and to develop policies and initiatives that attend to the arena in which community members reside. As a result, community members experience better health outcomes, lower health disparities, and an enhanced quality of life.
CONCLUSIONS
Leadership and policy play a central role in improving the quality of life, and they must be considered in any health plan. Strong and successful health leadership is vital for establishing and executing policies that favor and promote improvements in quality of life. This involves elements like putting resources behind collaboration across stakeholders and proposing policies to address social determinants of health. Soundly informed policies under strong leadership can positively impact the quality of life indicators such as access to health care, education, and opportunities for meaningful work. Improvements in quality of life, in turn, can also influence health policy, creating a loop of feedback that enables ongoing enhancement. With a holistic approach to improving it—captured in the short-term health improvements and long-term quality of life (QoL) expansion addressable by health leadership and policy collaboration, directly affiliated with the wonks of June and Fleet, and beyond.
BIBLIOGRAPHIC REFERENCES
1. Ferris, R., Baum, C., Kwak, E., Austin, J., Ester son, J., Harmless, G., ... & Tinetti, M. E. (2018). Perspectives of patients, clinicians, and health system leaders on changes needed to improve the health care and outcomes of older adults with multiple chronic conditions. Journal of aging and health, 30(5), 778-799.
2. Prelutsky, I. (2020). Mattering at the intersection of psychology, philosophy, and politics. American journal of community psychology, 65(1-2), 16-34.
3. Scheid, A. I., Baker, K. E., Restart, A. J., & Sell, R. L. (2022). Health and health care among transgender adults in the United States. Annual review of public health, 43(1), 503-523.
4. Audette, A. P., Lam, S., O’Connor, H., & Radcliff, B. (2019). (E) Quality of life: A cross-national analysis of the effect of gender equality on life satisfaction. Journal of Happiness Studies, 20(7), 2173-2188.
5. Ferris, R., Baum, C., Kwak, E., Austin, J., Ester son, J., Harmless, G., ... & Tinetti, M. E. (2018). Perspectives of patients, clinicians, and health system leaders on changes needed to improve the health care and outcomes of older adults with multiple chronic conditions. Journal of aging and health, 30(5), 778-799.
6. Ethiopia, D., (2021). The evolution of the quintuple aim: health equity, health outcomes, and the economy. Journal of the American College of Cardiology, 78(22), 2262-2264.
7. Restaurant, N., & Sheridan, A. D. (2020). Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: intersection, impact, and interventions. Journal of the American College of Radiology, 17(7), 921-926.
8. Sherman, J. D., Thiel, C., MacNeill, A., Eckel man, M. J., Dubrow, R., Hop, H., ... & Bile, M. M. (2020). The green print: advancement of environmental sustainability in healthcare. Resources, Conservation and Recycling, 161, 104882.
9. Smith, S. G., & Sink ford, J. C. (2022). Gender equality in the 21st century: Overcoming barriers to women's leadership in global health. Journal of Dental Education, 86(9), 1144-1173.
10. Serrati, D., Jackson, C. G. C. A., Macfarlane, S., Bissett, I., Robson, B., Gurney, J., ... & McMenamin, J. (2019). Cancer Care at a Crossroads: time to make a choice. NZ Med J, 132(1493), 6-11.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Prabhjot Kaur, Shreya Ghosal, Pooja Varma, Tanveer Ahmad Wanih, Devanshu J. Patel, Satyabhusan Senapati, Shilpa C. Patil.
Methodology: Prabhjot Kaur, Shreya Ghosal, Pooja Varma, Tanveer Ahmad Wanih, Devanshu J. Patel, Satyabhusan Senapati, Shilpa C. Patil.
Software: Prabhjot Kaur, Shreya Ghosal, Pooja Varma, Tanveer Ahmad Wanih, Devanshu J. Patel, Satyabhusan Senapati, Shilpa C. Patil.
Drafting - original draft: Prabhjot Kaur, Shreya Ghosal, Pooja Varma, Tanveer Ahmad Wanih, Devanshu J. Patel, Satyabhusan Senapati, Shilpa C. Patil.
Writing - proofreading and editing: Prabhjot Kaur, Shreya Ghosal, Pooja Varma, Tanveer Ahmad Wanih, Devanshu J. Patel, Satyabhusan Senapati, Shilpa C. Patil.