doi: 10.56294/hl2024.388
ORIGINAL
Quality of Life and the Role of Integrated Care Models in Healthcare
Calidad de vida y papel de los modelos de atención integrada en la asistencia sanitaria
Jaskirat Singh1 ![]() , Divya Sharma2
, Divya Sharma2 ![]() , Mukesh Parashar4
, Mukesh Parashar4 ![]() , Geetika M. Patel5
, Geetika M. Patel5 ![]() , Asish Malla6
, Asish Malla6 ![]() , Rajsinh V. Mohite7
, Rajsinh V. Mohite7 ![]()
1Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
2Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
3School of Business Management, Noida International University. Greater Noida, Uttar Pradesh, India.
4Parul University, Department of Community Medicine. PO Limda, Tal. Waghodia, District Vadodara, Gujarat, India.
5IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of General Medicine. Bhubaneswar, Odisha, India.
6Krishna Institute of Medical Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”, Dept. of Preventive & Social Medicine. Taluka-Karad, Dist-Satara, Maharashtra, India.
Cite as: Singh J, Sharma D, Parashar M, Patel GM, Malla A, et al. Quality of Life and the Role of Integrated Care Models in Healthcare. Health Leadership and Quality of Life. 2024; 3:.388. https://doi.org/10.56294/hl2024.388
Submitted: 10-03-2024 Revised: 28-07-2024 Accepted: 10-11-2024 Published: 11-11-2024
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: quality of life use has gained attention from healthcare professionals due to its broad intersections of factors from personal relationships to social support to psychological well-being and physical health.
Discussion: integrated care models may help improve the overall quality of life by focusing on coordinated, generalized, systematic and comprehensive healthcare. The objective of this study was to examine how integrated care models can enhance the quality of life of individuals within healthcare systems.
Method: a systematic literature review was performed to assess the effectiveness of integrated care models on healthcare quality of life. Data from relevant publications between 2010 and 2020 were included, and quality assessments were made using standardized tools.
Results: the evidence shows that integrated care models have a positive impact on the quality of care. Such models incentivize cooperation between healthcare suppliers, generating a more complete and patient-centered solution. In addition, they promote family and social support network involvement and enhance individuals’ personal relations and psychological well-being. Incorporating digital technology into integrated care models can improve access to care and enable self-management of health, both of which positively impact overall quality of life as well.
Conclusions: integrated care models support individuals with diseases in health facilities to improve their quality of life. It also reinforces the importance of a more integrated and holistic healthcare system—which focuses on quality of life, not just stroke and disabling conditions. Long-term goals need to be assessed in terms of quality of life by implementing integrated care models into practice.
Keywords: Physical Health; Psychological; Integrated; Healthcare.
RESUMEN
Introducción: el uso de la calidad de vida ha ganado la atención de los profesionales sanitarios debido a sus amplias intersecciones de factores que van desde las relaciones personales al apoyo social, pasando por el bienestar psicológico y la salud física.
Discusión: los modelos de atención integrada pueden ayudar a mejorar la calidad de vida en general al centrarse en una atención sanitaria coordinada, generalizada, sistemática e integral. El objetivo de este
estudio fue examinar cómo los modelos de atención integrada pueden mejorar la calidad de vida de las personas dentro de los sistemas sanitarios.
Método: se realizó una revisión sistemática de la literatura para evaluar la eficacia de los modelos de atención integrada en la calidad de vida de la atención sanitaria. Se incluyeron datos de publicaciones relevantes entre 2010 y 2020, y se realizaron evaluaciones de calidad utilizando herramientas estandarizadas.
Resultados: la evidencia muestra que los modelos de atención integrada tienen un impacto positivo en la calidad asistencial. Dichos modelos incentivan la cooperación entre proveedores sanitarios, generando una solución más completa y centrada en el paciente. Además, promueven la participación de la familia y la red de apoyo social y mejoran las relaciones personales y el bienestar psicológico de los individuos. La incorporación de la tecnología digital a los modelos de atención integrada puede mejorar el acceso a la atención y permitir la autogestión de la salud, factores ambos que también repercuten positivamente en la calidad de vida en general.
Conclusiones: los modelos de atención integrada ayudan a las personas con enfermedades en centros sanitarios a mejorar su calidad de vida. También refuerzan la importancia de un sistema sanitario más integrado y holístico, que se centre en la calidad de vida y no sólo en el ictus y las afecciones discapacitantes. Es necesario evaluar los objetivos a largo plazo en términos de calidad de vida mediante la implantación en la práctica de modelos de atención integrada.
Palabras clave: Salud Física; Psicológica; Integrada; Asistencia Sanitaria.
INTRODUCTION
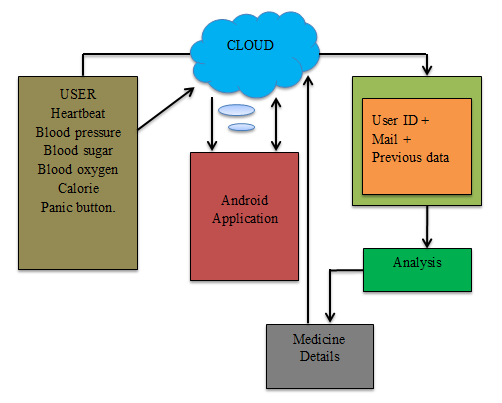
Quality of life is a multidetermined phenomenon with both objective and subjective variables. These aspects include physical health, mental health, social support, and economic stability.(1) In healthcare, the aim always is not just to treat diseases and conditions but also to enhance the quality of life of patients. Integrated care models are crucial in helping individuals live their best lives and achieve optimal health/well-being. Integrated care describes the organization of health services delivering primary, secondary, and tertiary health care in a coherent unit of health care provision.(2) The cooperative approach to diverse sectors, including primary care, specialty care, mental health, and social services, will lead to a holistic healthcare solution. Studies suggest that integrated care models can enhance patient quality of life by meeting a patient's physical, mental and social needs more efficiently and effectively. One of the key advantages of integrated care models is their focus on prevention and early intervention. Coordinating with the various providers in the healthcare continuum shuttles people to see if these concerns are treated early enough to prevent serious health issues down the line. This is not just about enhancing their overall health but also curbing healthcare expenses in the future. An example of integrated care could be a patient with a chronic disease like diabetes, whose visit schedule may involve regular check-ups with their primary care doctor, nutrition counseling sessions with a registered dietitian, and exercise therapy with a physiatrist.(3) This holistic approach enables more effective management of patients' overall health care, as lifestyle components are addressed in addition to medical questions contributing to that person's condition. Integrated care models also foster patient-centered care, where patients are involved in their own healthcare decisions. The model encourages patients to express their needs and desires, and medical providers collaborate to create a specialized care plan factoring in the patient's objectives, preferences, and values.(4) "This helps empower patients to take ownership of their health and well-being and helps them feel — and be — more satisfied with their care. This subsequently improves their quality of life. Mental health, despite being an essential part of a person's overall health, is typically overlooked by the healthcare system. Integrated care models acknowledge the interconnection between physical health and mental well-being, incorporating mental health services within the broader care plan. It is particularly significant for people living with chronic illnesses, who are more susceptible to developing mental health problems, including depression and anxiety. Patients whose mental health needs are addressed along with their physical health can enjoy an improved quality of life and overall outcomes.(5) Additionally, integrated care models facilitate improved communication and coordination between healthcare providers. This will contribute to an efficient and streamlined healthcare delivery system, which in turn eliminates severe burdens for patients and their families.(6) For example, people with complex medical needs might need to deal with many practitioners and appointments, which can be overwhelming. An integrated care model ensures that healthcare professionals involved in a patient's care are connected and communication is streamlined, thus ensuring that the patient gets the best care possible and is able to get their needs addressed as soon as possible.(7) This can help patients avoid the stress and frustration of navigating the healthcare system and encourage a healthier and happier life for them. Finally, quality of life is an integral part of healthcare, and integrated care models can play a prominent role in improving it. The integrated care model treats the patient holistically, addressing their physical, mental, and social needs rather than simply focusing on disease management. They encourage prevention and early intervention, patient-centered care, and improved communication among health care providers.(8) Thus, they play an instrumental role in enhancing the quality of life for individuals and healthier and happier communities. The main contribution of the paper has the following:
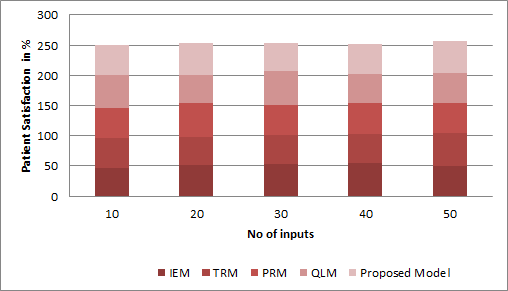
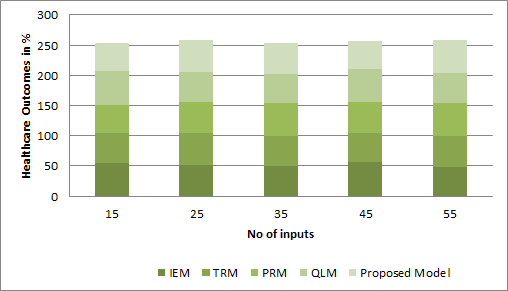
· Consolidating care models in healthcare has demonstrated better patient outcomes, including greater satisfaction with care, improved health outcomes and decreased hospital readmissions.
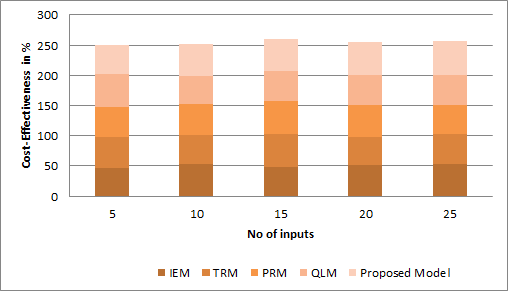
· Integrating Models For Health − Quality of Life and Integrated Care Models in Healthcare To increase Efficiency and Cost-Effectiveness, Integrated care models can help to reduce healthcare costs by coordinating care across settings and service providers, delivering care that is evidence-based and preventive, and minimizing the need for costly invasive medical intervention and hospitalization.
· Integrated care models enhance patient continuity of care as well. These models improve communication and coordination among all elements of patient care by bringing together different healthcare providers and disciplines.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
METHOD
Kilbourne, A. M., et al. Even improving the quality of mental health care globally requires measuring and accounting for factors like accessibility, effectiveness and patient satisfaction. This normalization can be made possible through standardized measures and ongoing assessment and optimization work with different stakeholders around the globe. Urban planning has been explored, which is the people habitat layout design and management process as a good home environment to improve residents' quality of life. This review covers the relationship between the built environment (i.e., design of neighborhoods and accessibility of resources) and subjective well-being (i.e., happiness and satisfaction with life). In one study of patients with diagnosed COVID-19, those with obesity had a significantly higher mortality rate. This was seen in a high-resourced integrated healthcare organization and underlines how obesity must be recognized as a risk factor for severe disease and mortality due to COVID-19. Regnault, A. et al. Mixed methods inquiry in health outcomes research [4], which integrates qualitative and quantitative data to explore complex health issues. This method incorporates the strengths of both approaches and provides a more encompassing and comprehensive understanding of health outcomes. This is an example of best practice in research, as relevant information can yield more indicative results. Have described the CABANA randomized clinical trial, which demonstrated that catheter ablation significantly improved the quality of life of patients with atrial fibrillation compared to medical therapy. The catheter ablation patients had significantly fewer symptoms and fewer limitations in daily activities, resulting in an overall improved quality of life.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Kilbourne, A. M.,et,al. |
2018 |
Identifying and addressing gaps in care can improve access, effectiveness, and overall outcomes for individuals and communities. |
The subjectivity of individual experiences cannot be fully captured in standardized quality measures and improvements. |
|
Mouratidis, K.,et,al. |
2021 |
Increased accessibility to resources and amenities, promoting a sense of community and improving overall quality of life. |
"Subjective well-being may not always be accurately reflected in objective measurements of the built environment." |
|
Tartof, S. Y.,et,al. |
2020 |
This study provides comprehensive data and insights on the link between obesity, mortality, and COVID-19 within a large healthcare organization. |
The study may not be generalizable to non-integrated healthcare organizations due to potential differences in patient characteristics. |
|
Regnault, A.,et,al. |
2018 |
The use of mixed methods, which combine qualitative and quantitative data, allows for a more comprehensive understanding of complex health outcomes. |
Mixed methods inquiry can be time-consuming and resource-intensive, potentially limiting its application in large-scale health. |
|
Mark, D. B.,et,al. |
2019 |
Catheter ablation allows for improved quality of life compared to medical therapy for patients with atrial fibrillation. |
Generalizability of results to all patients with atrial fibrillation due to specific inclusion/exclusion criteria used in the study. |
|
Nguyen, H. C.,et,al. |
2020 |
Increased understanding of COVID-19 could lead to improved self-care practices and better management of symptoms. |
Language barriers may prevent some individuals from understanding important health information related to COVID-19. |
|
Willemse, S.,et,al. |
2020 |
Enhanced overall well-being and coping strategies for patients, families, and healthcare staff, leading to improved outcomes and reduced burnout. |
"Cultural diversity among patients and healthcare providers may pose challenges for providing effective spiritual care." |
|
Tran, B. X.,et,al.[8] |
2020 |
One advantage is an increase in economic opportunities and productivity due to the shift to online and remote work. |
The limitations of insufficient economic support and resources allocated for vulnerable populations during the pandemic. |
|
Peres, M. A.,et,al. |
2019 |
Prevention and treatment of oral diseases can improve overall health and quality of life for individuals and communities. |
Lack of access to dental care and prevention programs in underserved and marginalized populations. |
|
Stafford, M.,et,al. |
2018 |
Effective management and coordination of care lead to improved health outcomes and quality of life. |
Ability to accurately capture the complexity and dynamic nature of interactions between multiple health conditions and their impacts. |