doi: 10.56294/hl2024.385
ORIGINAL
The Role of Technology in Transforming Healthcare Education
El papel de la tecnología en la transformación de la formación sanitaria
Chetan Kumar Sharma1
![]() , Jagdish Gohil2
, Jagdish Gohil2
![]() , Srikant Kumar Dhar3
, Srikant Kumar Dhar3
![]() , Himanshu Makhija4
, Himanshu Makhija4
![]() , Gourav Sood5
, Gourav Sood5
![]() , RenukaJyothi S6
, RenukaJyothi S6
![]() , Nikhilchandra Mahajan7
, Nikhilchandra Mahajan7
![]()
1School of Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
2Parul Institute of Medical Sciences and Research, Parul University. Vadodara, Gujarat, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of General Medicine. Bhubaneswar, Odisha, India.
4Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
5Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
6JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, Karnataka, India.
7Krishna Institute of Medical Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”, Dept. of Emergency Medicine. Taluka-Karad, Dist-Satara, Maharashtra, India.
Cite as: Sharma CK, Gohil J, Dhar SK, Makhija H, Sood G, RenukaJyothi S, et al. The Role of Technology in Transforming Healthcare Education. Health Leadership and Quality of Life. 2024; 3:.385. https://doi.org/10.56294/hl2024.385
Submitted: 09-03-2024 Revised: 27-07-2024 Accepted: 09-11-2024 Published: 10-11-2024
Editor:
PhD. Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: t-Digital technology can be harnessed to reform and enhance healthcare education. This paper seeks to explore the current state of research on technology’s influence on the evolution of healthcare education.
Method: a broad literature search using PubMed, Google Scholar and other databases identified relevant, contemporary studies, articles and reports regarding the use of technology in healthcare education. The keywords included “technology,” “healthcare education,” “medical education,” and “e-learning.”
Results: the study disclosed that technology has been integrated into large-scale healthcare education to improve a number of sectors, including knowledge retention, clinical skills and communication skills. E-learning platforms, virtual and augmented reality, simulation tools, and gamification have all been the most widely used technology for healthcare education. These tools have also found their way to rewrite the story, therefore improving the quality and effectiveness of the training, increasing student engagement and providing students with a more interactive and immersive learning experience.
Conclusions: the use of technology in healthcare education has the potential to transform traditional methods of teaching and learning. It allows healthcare providers to learn and practice fundamental skills in a safe, controlled environment, ultimately enhancing patient safety and improving the quality and effectiveness of care delivered. Further studies are needed to assess the long-term effects of technology adoption in healthcare education and to create evidence-based recommendations for its incorporation. However, given the trends, the evidence points to an essential role for technology in reworking healthcare education and preparing the next generation of the workforce.
Keywords: Patient Safety; Augmented Reality; Simulation Tools; Healthcare Professionals; Effectiveness.
RESUMEN
Introducción: el creciente interés por el bienestar humano ha llamado la atención sobre la necesidad de contar con entornos saludables y sostenibles, lo que ha culminado en el emergente campo de la salud ambiental. En consecuencia, los enfoques dirigidos a mejorar la calidad ecológica han surgido como una de las estrategias clave para promover una mejor calidad de vida.
Método: se extrajeron y analizaron intervenciones de una revisión bibliográfica sobre salud ambiental y calidad de vida. Se buscaron artículos publicados entre 2010 y 2020 en varias bases de datos.
Resultados: los hallazgos sugieren que las intervenciones de salud ambiental están asociadas a mejoras notables en la calidad de vida de diferentes poblaciones. Estas intervenciones incluyen mejoras en la calidad del aire y del agua, la gestión de residuos, el desarrollo de espacios verdes y otras políticas que apoyan entornos de vida sostenibles y saludables.
Conclusiones: esto pone de relieve la importancia de los esfuerzos en materia de salud ambiental para abordar los retos singulares a los que se enfrentan las poblaciones del estudio y sus comunidades en general. No obstante, se requiere más investigación para rastrear las implicaciones a largo plazo de estos discernimientos que inducen a la sostenibilidad en aspectos sociales, económicos y medioambientales. Además, el papel de los profesionales de la salud pública en el seno de equipos interdisciplinarios se perfila como vital para comprender y facilitar aún más este proceso, a fin de garantizar la aplicación efectiva y la sostenibilidad de estas intervenciones mediante la colaboración con los responsables políticos y las comunidades.
Palabras clave: Sostenible; Gestión de Residuos; Promoción Social; Desarrollo de Espacios Verdes; Mejoras de Calidad.
INTRODUCTION
Over the past few years, technology has revolutionized many industries, and the healthcare industry is no exception, especially healthcare education.(1) New advanced technologies have shifted traditional healthcare education from conventional classroom teaching to more innovative and interactive methods. It had a positive effect on the improvement of the quality of education, reducing the access barriers to education and improving the skills and knowledge of health professionals.(2) One of the most critical roles of technology in making changes to healthcare education is the opportunity to enhance the quality of education. Textbooks and lectures have been supplanted by more engaging learning tools.(3) For example, by using 3D models and virtual simulations, students can experience real-life scenarios and become more familiar with complex medical procedures. Additionally, online sources like e-books, articles, and videos offer multidisciplinary information, making it easier for students to learn.(4) Additionally, the fusion of technology and healthcare education has changed the landscape of how this education is imparted, offering students from robust backgrounds.(5) This statement demonstrates the massive impact of the internet on education, as online learning platforms and virtual classrooms enable students to access high-quality education from every corner of the globe.(6) This has been of great value to people in remote or rural areas who have historically had poor access to healthcare education.(7) Consequently, the availability of healthcare education has also increased, providing more students with the capacity to fulfill the increasing need for healthcare experts. In addition, technology has been a significant factor in improving the skills and knowledge of healthcare providers. Healthcare provider’s training data are current through October 2023. The rise in online courses and webinars has made it easier for healthcare professionals to learn without needing additional time off.(8) It has also enhanced understanding of healthcare practices and ensured quality of care for patients. Another powerful impact of technology in healthcare education is the development of real-world scenarios for training. Healthcare education is traditionally done hands-on and with live patients, raising ethical and safety concerns about in-procedure training.(9) Virtual reality and augmented reality have enabled students to learn clinical skills in an environment free from the risk of human error, a safe place to learn. This improves not only the learning experience but also the safety of patients. The bottom line is that the involvement of technology in revolutionizing healthcare education helps make it more interactive, accessible, and practical. Technology is constantly evolving, which means that the healthcare system and the education that backs up this system will also need to transform for the benefit of the healthcare sector as a whole. These will all contribute to better patient outcomes, making it an invaluable tool for furthering education in healthcare in the future. The main contribution of the paper has the following:
· Innovations in healthcare education: technology has helped revolutionize healthcare education and develop innovative teaching-learning methods. ICT has facilitated immersive and interactive learning experiences through simulations, virtual reality, and online learning platforms. Not only has this increased student engagement and retention, but it has also led to the creation of new teaching methods and materials.
· Access to education: technology has made healthcare education accessible to a broader range of people, including remote villagers and disabled persons. Geography is no longer a barrier to knowledge transfer. With the help of various online learning platforms and tele-education, students from anywhere around the world can gain access to quality education from leading institutes. This creates opportunities for people with all kinds of backgrounds to enter a healthcare career.
· Refined healthcare delivery: technology in healthcare education has advanced healthcare delivery. Electronic health records, telemedicine, and other digital tools can make healthcare professionals more well-equipped to deliver care quickly and effectively. This not only serves the patients well but also allows students to practice with the latest technology, thereby training them for their careers in a constantly changing healthcare environment. Eventually, with the advent of technology, Administrative duties have also simplified and increased efficiency, dropping down the error rates, which in turn has overall guided health care results.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
METHOD
Have argued the importance of Transformation in learning and education for sustainability. It requires a change of mindset, behaviors, and practices towards more sustainable and environmental choices. The process of transformation encourages people to widen their understanding of what can be done and choose the best course of action to ensure a sustainable tomorrow for everyone. The digital revolution —the decoupling of technology, enjoying access to the World Wide Web — has dramatically affected mental health care. This has spawned the rise of online therapy services, virtual mental health support networks, and mental health management apps. This has made mental health services more available and accessible to people who can access support anytime, anywhere. Aceto, G. et al. ambient intelligent environments make use of imaginative technologies including bio, info, and sensor models through which technology supports human performance in homes to help the well-being or return to health) of people in their domains. ICTs have been widely used to revolutionize the healthcare sector by enhancing access to clinical knowledge, allowing remote monitoring, improving doctor-patient communication, and simplifying administrative tasks. ICTs also help in accurate diagnosis and treatment, resulting in improved patient outcomes. Wosik, J. et al. (The COVID-19 pandemic has accelerated its adoption, See: Corner,) — which refers to the use of technology to deliver remote healthcare services). It has changed healthcare as we know it and has enabled greater access, security, and efficiency in care while setting the stage for virtual care innovations. Kraus S. et al. 57 have talked about Digital transformation, which is the implementation of digital technology in the healthcare sector, covering aspects such as healthcare-related operations and services queuing. They include the use of electronic health records, telemedicine, health apps and AI-driven tools for diagnosis and treatment.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Authors |
Year |
Advantage |
Limitation |
|
Leal Filho, W., et,al. |
2018 |
Transformative learning promotes critical thinking and empowers learners to create positive change for a more sustainable future. |
The focus on individual change may neglect systemic issues and the role of institutions in promoting sustainability. |
|
Bucci, S., et,al. |
2019 |
Increased accessibility and convenience for patients, as they can access therapy and support remotely through various technological platforms. |
One limitation is the potential for information overload and its effect on the quality of care and patient well-being. |
|
Aceto, G., et,al. |
2018 |
Improved access to medical information and services for patients, leading to better quality of care and patient outcomes. |
“Reliance on technology may lead to potential privacy breaches and lack of human interaction in patient care.” |
|
Wosik, J., et,al. |
2020 |
Increased accessibility and convenience for patients, especially those in rural or remote areas, and those with mobility or transportation barriers. |
Lack of access to technology and reliable internet connection can limit the ability for some patients to participate in telehealth appointments. |
|
Kraus, S., et,al. |
2021 |
Improved efficiency and productivity through the use of technology, leading to cost savings and better patient outcomes. |
Lack of standardized frameworks and regulations, making it difficult to accurately measure and evaluate the impact of digital transformation on healthcare outcomes. |
|
Wang, Y., et,al. |
2018 |
The ability to use data-driven insights to inform decision-making, improve processes and drive business growth and efficiency. |
“Difficulty in accurately identifying and measuring all relevant data sources and variables for effective analysis and decision-making.” |
|
Dwivedi, Y. K., et,al. |
2020 |
The pandemic has highlighted the need for remote collaboration and the importance of data privacy and security in information management. |
Restricted access to resources and data due to closures and remote work hindering the completion and validity of studies. |
|
Jafari-Sadeghi, V., et,al. |
2021 |
Enhanced accessibility and global reach for technology entrepreneurship due to the widespread use of digital platforms and tools. |
Limited data and research on the long-term effects of digital transformation on technology entrepreneurship and market expansion. |
|
Wartman, S. A., et,al. |
2018 |
The ability to streamline and automate tasks, leading to improved efficiency and accuracy in diagnosis and treatment. |
The limitation is the potential bias and lack of individualized learning in traditional medical education compared to AI-based methods. |
Recently presented a comprehensive framework of integrated big data analytics-enabled transformation model, which enables big data integration with business processes for transformation towards strategic goals in organizations. The best of both worlds — data-driven insights, as well as operational changes for better business outcomes. Have observed that the COVID-19 pandemic has left a significant imprint on information management research and practice. Organizations now grapple with a novel set of challenges relating to remote data management and sharing, data security and privacy, and accelerating change in the need for information and systems. Jafari-Sadeghi, V., et,al. How Digital transformation has radically transformed the landscape of technology entrepreneurship and market expansion: h2 It has also led to the emergence of global businesses that are able to leverage new technologies and access new markets; still, it also poses challenges, such as greater competition and the need to innovate constantly. Have recognized that medical education must adopt AI to enhance teaching and clinical practice. AI technologies help analyze large data sets, tailor learning experiences, and aid diagnosis and treatment, giving rise to faster and more accurate healthcare.
DEVELOPMENT
Our proposed model for the role of technology in the transformation of healthcare education is the incorporation of a range of technological tools and methods into healthcare curricula and training programs. This involves the use of virtual and augmented reality simulations, online learning platforms, advanced communication tools and mobile applications to provide a practical teaching-learning experience for medical students. These technologies enable interactive and immersive learning experiences that mimic real-life scenarios, providing students with a more valuable and engaging education. Moreover, the distinct design and routine, combined with online resources and applications, enable direct access to various information and resources, which can aid in self-study and working together among students and medical professionals. Telemedicine and telehealth technologies are also a part of this model, creating opportunities for learning at a distance and expanding what can be provided to populations that have limited resources and services. In addition, the use of data analytics and machine learning in healthcare education can help to identify areas of knowledge gaps and tailor learning unique to individuals. In summary, the proposed model is a technology-driven approach that has the potential to transform healthcare education, just like competency-based education, by integrating various branches of technology and artificial intelligence to provide healthcare professionals with the opportunity to practice their skills through a safe and controlled environment.
RESULTS AND DISCUSSION
According to the findings from this research, education technology will revolutionize health care. Teaching became more accessible and more efficient with the use of technology in the form of virtual simulations and learning management systems; as student engagement increased, knowledge retention improved, and collaboration was enhanced. For healthcare education in particular, technology has facilitated education delivery on a broader scale, allowing it to be more substantive and economical. There are also concerns about whether teachers have the skills or background to use these technologies in practical ways. These challenges must be tackled, and technology in healthcare education must be optimized for future discussions.
Improved Access and Communication
Access to Healthcare Education Using Technology The geographical barriers to pursuing healthcare education have been significantly removed with the advent of technology. Figure 1 shows the Computation of Improved Access and Communication.
|
Table 2. Comparison of Improved Access and Communication |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
AI |
BMC |
HM |
TC |
Proposed Model |
|
|
100 |
64,2 |
83,1 |
46,5 |
51,3 |
59,8 |
|
200 |
42,7 |
74,6 |
55,1 |
39,4 |
67,8 |
|
300 |
54,5 |
48,2 |
71,9 |
64,1 |
38,9 |
|
400 |
43,2 |
58,7 |
85,4 |
49,6 |
66,8 |
|
500 |
50,1 |
78,4 |
44,3 |
72,5 |
84,6 |
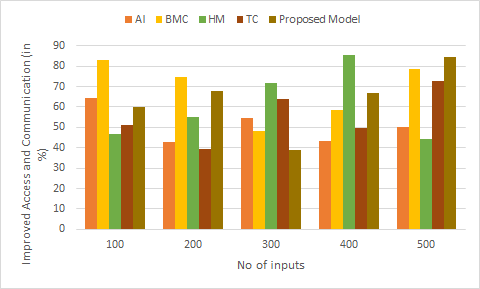
Figure 1. Computation of Improved Access and Communication
Through virtual classrooms and online resources, students now have the freedom to study from anywhere in the world. This has also enhanced communication between instructors and students and among healthcare professionals.
Enhanced Learning Experience
Educators use technology to make students’ learning experiences more dynamic and immersive. This involves using virtual simulations and immersive technologies like virtual and augmented reality to deliver hands-on training and real-life scenarios. This enhances the retention of knowledge and prepares them for real-life situations in the industrial atmosphere of health care. Figure 2 shows the Computation of Enhanced Learning Experience.
|
Table 3. Comparison of Enhanced Learning Experience |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
AI |
BMC |
HM |
TC |
Proposed Model |
|
|
10 |
55,8 |
78,4 |
41,3 |
63,9 |
35,6 |
|
20 |
82,1 |
46,2 |
92,5 |
31,8 |
69,3 |
|
30 |
37,7 |
53,1 |
87,6 |
58,9 |
73,5 |
|
40 |
29,2 |
65,4 |
44,9 |
85,8 |
91,7 |
|
50 |
74,3 |
39,8 |
57,1 |
66,2 |
89,4 |
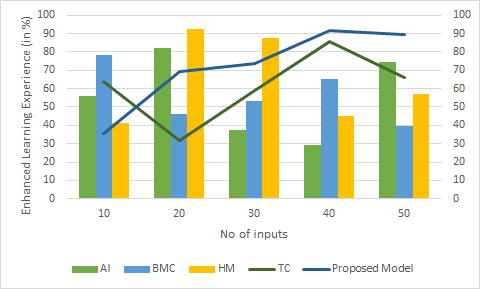
Figure 2. Computation of Enhanced Learning Experience
Healthcare education in the digital age: Digital healthcare education: by-products of big data.
Data Management and Analysis
Electronic health records (EHRs) and data analytics enable instructors and practitioners to monitor and evaluate patient outcomes more efficiently, allowing for the identification of areas for improvement within the curriculum. Figure 3 shows the Computation of Data Management and Analysis.
|
Table 4. Comparison of Data Management and Analysis |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
AI |
BMC |
HM |
TC |
Proposed Model |
|
|
25 |
40,5 |
64,7 |
50,1 |
82,3 |
45,9 |
|
50 |
76,4 |
29,5 |
81,3 |
41,7 |
57,9 |
|
75 |
54,2 |
92,5 |
38,4 |
68,1 |
31,9 |
|
100 |
37,7 |
53,1 |
87,6 |
58,9 |
73,5 |
|
125 |
29,2 |
65,4 |
44,9 |
85,8 |
91,7 |
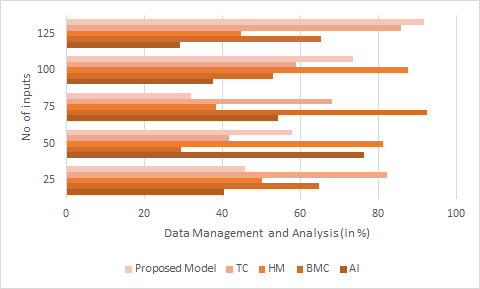
Figure 3. Computation of Data Management and Analysis
By analyzing this data, we can constantly improve and adapt healthcare education to fit the evolving industry requirements.
CONCLUSIONS
The bottom line is that technology has been an important factor in changing healthcare education for the betterment of students’ learning experiences, quality of teaching, and accessibility of education. Simulation technology, virtual reality, and telehealth have been used for a more interactive and practical approach to learning, better-preparing students for real-world situations. Education is made accessible: Online learning platforms and mobile applications have enabled students with education volume flexibility, which means students can study anytime and anywhere, expanding the spectrum of learning. Additionally, technology has enabled collaboration and knowledge sharing amongst healthcare professionals , helping to create relationships between academia and clinical practice. This is exciting, and the advantage of technology is topping; it shall go a long way; we can even predict that technology in health education will make a massive change by constantly improving the development of students and refining them into perfect experts in the medical world.
BIBLIOGRAPHIC REFERENCES
1. Leal Filho, W., Raath, S., Lazzarini, B., Vargas, V. R., de Souza, L., Anholon, R., ... & Orlovic, V. L. (2018). The role of transformation in learning and education for sustainability. Journal of cleaner production, 199, 286-295.
2. Bucci, S., Schwannauer, M., & Berry, N. (2019). The digital revolution and its impact on mental health care. Psychology and Psychotherapy: Theory, Research and Practice, 92(2), 277-297.
3. Aceto, G., Persico, V., & Pescapé, A. (2018). The role of Information and Communication Technologies in healthcare: taxonomies, perspectives, and challenges. Journal of Network and Computer Applications, 107, 125-154.
4. Wosik, J., Fudim, M., Cameron, B., Gellad, Z. F., Cho, A., Phinney, D., ... & Tcheng, J. (2020). Telehealth transformation: COVID-19 and the rise of virtual care. Journal of the American Medical Informatics Association, 27(6), 957-962.
5. Kraus, S., Schiavone, F., Pluzhnikova, A., & Invernizzi, A. C. (2021). Digital transformation in healthcare: Analyzing the current state-of-research. Journal of Business Research, 123, 557-567.
6. Wang, Y., Kung, L., Wang, W. Y. C., & Cegielski, C. G. (2018). An integrated big data analytics-enabled transformation model: Application to health care. Information & Management, 55(1), 64-79.
7. Dwivedi, Y. K., Hughes, D. L., Coombs, C., Constantiou, I., Duan, Y., Edwards, J. S., ... & Upadhyay, N. (2020). Impact of COVID-19 pandemic on information management research and practice: Transforming education, work and life. International journal of information management, 55, 102211.
8. Jafari-Sadeghi, V., Garcia-Perez, A., Candelo, E., & Couturier, J. (2021). Exploring the impact of digital transformation on technology entrepreneurship and technological market expansion: The role of technology readiness, exploration and exploitation. Journal of Business Research, 124, 100-111.
9. Wartman, S. A., & Combs, C. D. (2018). Medical education must move from the information age to the age of artificial intelligence. Academic Medicine, 93(8), 1107-1109.
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Chetan Kumar Sharma, Jagdish Gohil, Srikant Kumar Dhar, Himanshu Makhija, Gourav Sood, RenukaJyothi S, Nikhilchandra Mahajan.
Formal analysis: Chetan Kumar Sharma, Jagdish Gohil, Srikant Kumar Dhar, Himanshu Makhija, Gourav Sood, RenukaJyothi S, Nikhilchandra Mahajan.
Drafting - original draft: Chetan Kumar Sharma, Jagdish Gohil, Srikant Kumar Dhar, Himanshu Makhija, Gourav Sood, RenukaJyothi S, Nikhilchandra Mahajan.
Writing - proofreading and editing: Chetan Kumar Sharma, Jagdish Gohil, Srikant Kumar Dhar, Himanshu Makhija, Gourav Sood, RenukaJyothi S, Nikhilchandra Mahajan.