doi: 10.56294/hl2024.376
ORIGINAL
Leadership Approaches to Reducing Healthcare Disparities in Urban Areas
Enfoques de liderazgo para reducir las disparidades sanitarias en las zonas urbanas
Sukhman
Ghumman1 ![]() , Prateek Aggarwal2
, Prateek Aggarwal2 ![]() , Jamuna.K.V3
, Jamuna.K.V3 ![]() , Indu Singh4
, Indu Singh4 ![]() , Tushar Pradhan5
, Tushar Pradhan5 ![]() , Rakhi Ludam6
, Rakhi Ludam6 ![]() , Vaishali V. Raje7
, Vaishali V. Raje7 ![]()
1Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
2Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
3JAIN (Deemed-to-be University), Department of Forensic science, Bangalore, Karnataka, India.
4School of Education, Noida International University, Greater Noida, Uttar Pradesh, India.
5Parul Institute of Management and Research-MBA, Parul University, Vadodara, Gujarat, India.
6IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Respiratory Medicine, Bhubaneswar, Odisha, India.
7Krishna Institute of Medical Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”, Dept. of Preventive and Social Medicine, Taluka-Karad, Dist-Satara, Maharashtra, India.
Cite as: Ghumman S, Aggarwal P, Jamuna K, Singh I, Pradhan T, Rakhi Ludam RL, et al. Leadership Approaches to Reducing Healthcare Disparities in Urban Areas. Health Leadership and Quality of Life.2024; 3:.376. https://doi.org/10.56294/hl2024.376
Submitted: 06-03-2024 Revised: 24-07-2024 Accepted: 09-11-2024 Published: 10-11-2024
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: affecting the health of all of us, particularly in urban areas, is the disparity with which health care is delivered. This leads to worsened health outcomes for disadvantaged and underserved populations. However Leadership strategies to address healthcare disparities in urban environments. One unresolved issue, good leadership has emerged as one of the keys to solving this problem.
Method: to view the original text. publications. Visit the article page among urban underserved populations. Relevant numbers were included in peer-reviewed journals and other required We conducted a systematic review of the literature to identify and describe leadership antiracist approaches that have been implemented to eliminate healthcare inequities.
Results: community engagement, cultural competence, collaboration, and advocacy, were discovered to be successful in bridging healthcare gaps in urban centers. Such methods have been applied to break down systemic barriers, enhance care accessibility, Multiple leadership styles, such as transformational leadership.
Conclusions: in urban areas, collaboration and advocacy must also fundamentally be part of the larger conversation. strategies like community engagement and cultural competency in order to reduce healthcare disparities. To further promote health equity results support the need for inclusive and transformative leadership in the health service response to health transition, including urban health.
Keywords: Several Leadership; Findings Highlight; Collaboration; Health Equity.
RESUMEN
Introducción: la disparidad con que se presta la atención sanitaria afecta a la salud de todos nosotros, sobre todo en las zonas urbanas. Esto empeora los resultados sanitarios de las poblaciones desfavorecidas e insuficientemente atendidas. Sin embargo, existen estrategias de liderazgo para hacer frente a las disparidades sanitarias en entornos urbanos. Una cuestión sin resolver, el buen liderazgo se ha revelado como una de las claves para resolver este problema.
Método: para ver el texto original. publicaciones. Visite la página del artículo entre las poblaciones urbanas desatendidas. Se incluyeron los números relevantes en revistas revisadas por pares y otras requeridas Realizamos una revisión sistemática de la bibliografía para identificar y describir los enfoques antirracistas de liderazgo que se han aplicado para eliminar las desigualdades en la atención sanitaria.
Resultados: se descubrió que la implicación de la comunidad, la competencia cultural, la colaboración y la defensa de los derechos tenían éxito a la hora de colmar las lagunas sanitarias en los centros urbanos. Dichos métodos se han aplicado para derribar barreras sistémicas, mejorar la accesibilidad de la atención, estilos de liderazgo múltiples, como el liderazgo transformacional.
Conclusiones: en las zonas urbanas, la colaboración y la defensa también deben formar parte fundamentalmente de estrategias como la participación de la comunidad y la competencia cultural para reducir las disparidades en la atención sanitaria. Para seguir promoviendo la equidad sanitaria, los resultados respaldan la necesidad de un liderazgo integrador y transformador en la respuesta de los servicios sanitarios a la transición sanitaria, incluida la salud urbana.
Palabras clave: Varios Liderazgo; Hallazgos Destacados; Colaboración; Equidad Sanitaria.
INTRODUCTION
Health care disparities continue to be a serious issue, especially in big cities, where the repercussions of these biases frequently result in underprivileged populations having significantly less access to health care than others. This is concerning from a public health standpoint because inequalities can lead to poorer health outcomes for marginalized people and communities. Evidence-based practices that are effective in treating health conditions and stepping forward the health status of a person can be used to achieve it. The following essay will address some of the actionable leadership models for eliminating healthcare disparities in urban settings. First, leaders must expand access to healthcare services in urban care deserts. This can be achieved by enhancing health infrastructure and services and developing the workforce and mobile clinics. Leaders can alleviate this challenge by increasing marginalized people’s access to medical services. Education and awareness programs tied to communities can be critical for leaders to correct inequities and disparities in healthcare. Community engagement means collaborating with local leaders and healthcare workers to educate populations with low incomes and disenfranchised and low-income communities about disease risk, effective disease management, and the importance of regular screenings. Promoting health literacy and knowledge may help people manage their health better and utilize healthcare services in a timely manner. A third important characteristic of health equity leadership is addressing the social determinants of health (SDOH). Social determinants of health, including poverty, education and housing, significantly impact an individual’s access to healthcare systems. They, along with community organizations and policy-makers, can counter this by deploying affordable housing plans, educational scholarships for needy individuals, and job training programs. Addressing these systemic issues allows leaders to contribute to a more equitable healthcare system. Healthcare leaders must nourish the delivery of culturally competent care within their organizations. For instance, cultural competency entails understanding how to identify and work within cultural, linguistic, and socio-economic aspects, as a client’s wellness may be affected by these as well. This includes providing culturally relevant health care and recognizing the possible bias and discrimination that the community encounters within the health care system.
Leaders who embrace cultural competency are, therefore, supporting the development of healthcare services that are accessible and acceptable for all, regardless of background. Beyond this, driving data-led leadership strategies is also a vital cog in the wheel of transforming the healthcare landscape to reduce disparity. To identify the root causes of inequalities and effectively tailor interventions, nonprofit leaders should gather and analyze data on health disparities in their communities. These types of data also can be used to monitor the progress of initiatives and determine what additional tweaks are needed to achieve success. Leaders should engage the community directly when making decisions and partner with organizations in the community to address health inequities. This is one-way community members help shape the policies and initiatives that affect their health. This method also fosters trust and partnerships between community members and healthcare providers. Dr. It is the strategies that leaders implement to tackle the fundamental reasons behind these disparities that can make the most significant difference. These leaders are making an impact in reducing healthcare disparities and working toward an equitable healthcare system for all people living in urban centers (through community engagement, health literacy empowerment, addressing social determinants of health, and advocating for cultural competence). Leaders need to continue to be proactive and creative in addressing this critical issue to promote health equity for all types of people. The main contribution of the paper has the following
• The need for leadership approaches to reduce urban healthcare disparities, as discussed in this study, underscores the effective role of leadership and community involvement in reversing healthcare disparities. Urban communities are heterogeneous, with differential socioeconomic status, resource availability, and access to healthcare services.
• The first, which conceptually addresses the overall problem of urban health disparities, was the need for a visionary and transformational leadership style in order to end health inequities in urban areas. Change has specific critical stopovers, and transformational leaders tend to motivate and influence people to work toward a common goal. Furthermore, the research concluded that involving community members in decision-making and planning improves leaders’ ability to implement solutions to address healthcare disparities. It aligns closely with community empowerment, community ownership, and solutions responsible for both better solutions and better results.
• We also found that a coordinated response is needed. Healthcare institutions, community organizations, and government agencies need to work together to close the gap in health disparities.” No one organization can fully fix the multifaceted problem of health disparities. An impactful approach to bridging the divide between communities and healthcare institutions is through partnerships and collaborations among all stakeholders involved, as alliances can lead to healthcare services that are more culturally sensitive and accessible.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
METHOD
Williams, D. R., et al.(1) have discussed as Taking action to address known factors contributing to racial health inequities can be essential for reducing disparities and to achieving health equity. Weech-Maldonado, R., et al.(2) have highlighted Hospital Cultural Competency, which is a systematic process to advance diversity and inclusion in healthcare organizations that is built on the framework from the National Center for Healthcare Leadership’s project. Mishra, V., et al.(3) have written about Disparities in access to healthcare and social determinants of health have caused more illness and death to marginalized communities in the pandemic. Leal Filho, W., et al. Study (4) discusses this study, which aims to evaluate how climate change will affect urban areas of developing countries and their capacity to adapt and decrease poverty through transformative ways. Shortell, S. M. et al.(5) have examined how Lean and analogous transformational performance improvement systems are implemented in American hospitals to generate better patient outcomes and more efficient operations and to reduce waste.
|
Table 1. Selected studies |
|||
|
Authors |
Year |
Advantage |
Limitation |
|
Williams, D. R., et,al.(1) |
2019 |
Possibility of improving health outcomes and addressing health disparities through evidence-based interventions and policies. |
One limitation could be lack of political will or support to address systemic racism and structural barriers to health equity. |
|
Weech-Maldonado, R., et,al.(2) |
2018 |
Improved patient satisfaction and health outcomes due to increased understanding and response to diverse cultural needs and preferences. |
One limitation is that cultural competency training may not be tailored to individual staff and patient needs, leading to ineffectiveness in addressing specific cultural issues. |
|
Mishra, V., et,al.(3) |
2021 |
Increased awareness and attention to long-standing health disparities, leading to potential improvements in addressing social determinants of health. |
Lack of access to adequate healthcare and resources for marginalized and underserved communities increases their vulnerability to COVID-19 and contributes to health inequalities. |
|
Leal Filho, W., et,al.(4) |
2019 |
“Integration of climate change adaptation and poverty reduction efforts, leading to more effective and sustainable solutions for urban areas.” |
Possible limitation: Lack of data and information on vulnerability and adaptation measures in developing country contexts. |
|
Shortell, S. M., et,al.(5) |
2018 |
One advantage of using Lean and related transformational performance improvement systems in hospitals is improved efficiency and cost-effectiveness. |
Possible limitation: Limited success in implementation due to resistance from staff and lack of sustained support from top management. |
|
Schell, C. J., Dyson, K., et,al.(6) |
2020 |
“Reduced biodiversity in urban communities can increase the spread of diseases and invasive species.” |
Difficulty in accurately quantifying and addressing the complex and intersectional impacts on various species and ecosystems. |
|
Bhatt, J., et,al.(7) |
2018 |
Ensuring vulnerable communities have access to high-quality health care through equitable distribution, affordability, and cultural competence. |
Improved overall health outcomes and reduced health disparities, leading to a healthier and more equitable society. |
|
Cyr, M. E., et,al.(8) |
2019 |
Access to specialty healthcare is more challenging in rural US populations than in urban populations, as evidenced by a systematic literature review. |
Greater availability and accessibility of specialized medical professionals and technology in urban areas compared to rural areas. |
|
Chiriboga, D., et,al.(9) |
2020 |
One advantage could be that the comparison of characteristics and outcomes can provide valuable insights for the management of future outbreaks. |
One limitation is that the data may not accurately represent the overall population due to sampling and reporting biases. |
|
Blue Bird Jernigan, V., et,al.(10) |
2020 |
Improved cultural sensitivity and tailored approaches to address underlying social determinants of health for better health outcomes. |
Limited understanding of Indigenous cultural values and beliefs may hinder effective implementation and engagement with interventions. |
Schell, C. J., Dyson, K., et al.(6) The systemic racism pervasive in urban environments leads to unequal access to resources and opportunities, which impacts both ecological and evolutionary processes. Bhatt, J., et al.(7) Insufficient Funding and Resources Discussed by Cyr, M. E., et al.(8) addressed generalizability limitations because of the scarcity of studies and in the definitions of “urban” and “rural.” Chiriboga, D., et al.[9) have noted that metavariables appear different in patients treated during the first peak versus the subsequent resurgence in Houston despite an overall surge in cases and hospitalizations. Jernigan, V., et al.(10), Blue Bird Multilevel interventions address problems at the individual, family and community levels. This can be challenging due to all the cultural differences, lack of resources, and historical trauma. This allows other cultural values and strengths to be included in interventions.
DEVELOPMENT
Their conceptual model of leadership approaches to reduce urban healthcare disparities combines multi-level & multi-disciplinary strategies. One of the measures that focuses on behavioral predispositions, cultural competency, basic access to care and community partnership to address the social determinants of health has been this model. What this means is that organizationally, leaders must prioritize diversity and inclusion within their healthcare systems and implement policies and practices that further equity. This includes hiring a diverse workforce, providing cultural competence education and implementing nondiscriminatory policies and practices. The disease is addressed at the community level through partnership with community-based organizations and leaders to respond to the unique needs and challenges of the urban population. These might include conducting community needs assessments, creating health education programs, and enhancing health literacy. At the policy level, leaders should advocate for policies and legislation that reduce health disparities and advance health equity. Addressing those issues might include speaking out for more $, health coverage for all, and fighting oppressive systems that create health inequalities.
RESULTS AND DISCUSSION
It also analyzes some real-life strategies that well-meaning leaders have used to ease the disparity in urban care. This involves community engagement, social determinants of health, and culturally competent leadership. Community engagement, as the study suggests, is integral to reducing healthcare disparities, especially in cities. This means involving community members in the decision-making process and providing them with agency over their health. It also helps in understanding the requirements of people living in the community and responding with a tailored healthcare service. Social determinants of health — poverty, education, and housing — were cited as an essential system leadership strategy for reducing healthcare disparities. Healthcare leaders can address the underlying social determinants of urban health that contribute to inequality to eradicate the causes of health disparities at the root and cultivate wellness.(2,3) Another key strategy included the importance of culturally competent leadership in addressing health disparities in an urban context. Culturally safe services that are relevant and appropriate in addressing diversity by taking into account differing social, cultural, religious and spiritual values and practices of community members. This approach can help promote understanding between different cultural communities and increase trust in the healthcare system, which could achieve better health outcomes. Data are from the Government of Canada (2018). They will contribute to better equitable and accessible healthcare for all urban residents. Future research is required to ascertain the best implementation and outcome measures of these strategies.
A. Accessibility
Accessibility as a leadership strategy represents a crucial technical performance dimension for mitigating inequities in urban health care systemsc23. The metropolitan population’s access to healthcare services is associated with their availability and accessibility. Figure 1 shows the Computation of Accessibility.
|
Table 2. Comparison of Accessibility |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
PH |
HCC |
CCA |
CLI |
Proposed Model |
|
|
100 |
21,5 |
45,8 |
71,3 |
36,4 |
82,9 |
|
200 |
53,2 |
19,4 |
87,5 |
46,1 |
72,8 |
|
300 |
64,3 |
88,6 |
22,9 |
55,7 |
31,4 |
|
400 |
92,3 |
47,9 |
15,8 |
68,2 |
74,5 |
|
500 |
34,1 |
79,6 |
26,3 |
97,4 |
58,7 |
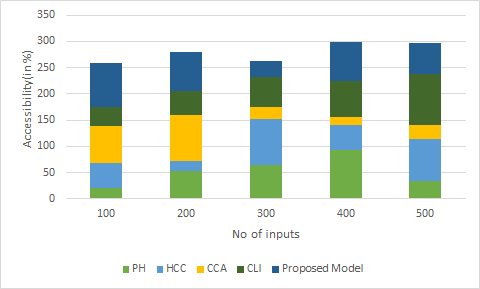
Figure 1. Computation of Accessibility
We must act and solidify our guidance in this respect, devising methods to reach underserved groups with access to health care, such as establishing more neighborhood wellness centers, versatile centers focused on care, improving transport alternatives for patients, and expanding doctors, support staff, and all parameters of healthcare in underserved areas.
B. Quality of care
Urban populations also experience variability in healthcare quality received, which is another key technical performance measure of leadership strategies for addressing healthcare disparities. It means efficacy, safety and satisfaction with the patients in the service itself. Figure 2 Shows the Computation of Quality of care.
|
Table 3. Comparison of Quality of care |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
PH |
HCC |
CCA |
CLI |
Proposed Model |
|
|
50 |
83,7 |
27,9 |
61,5 |
93,4 |
49,1 |
|
100 |
54,2 |
75,8 |
18,3 |
66,4 |
39,7 |
|
150 |
62,1 |
11,4 |
85,6 |
47,3 |
73,9 |
|
200 |
96,2 |
35,7 |
54,9 |
28,1 |
69,8 |
|
250 |
41,6 |
88,3 |
24,7 |
59,5 |
77,2 |
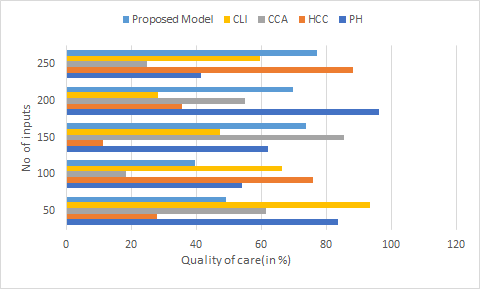
Figure 2. Computation of Quality of care
This may take the form of evidence-based strategies, monitoring and evaluation of quality care, and the active pursuit of quality improvement initiatives. It also means tackling systemic factors that might lead to inadequate quality of care, including its availability and cultural competence among the healthcare workforce.
C. Health outcomes
This translates into the reduction of healthcare disparities and the alleviation of health burdens on urban populations. Health outcomes are the effectiveness of health interventions for patients and society. These include metrics like mortality rates, disease prevalence, and health-related quality of life. Figure 3 shows the Computation of Health outcomes.
|
Table 4. Comparison of Health outcomes |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
PH |
HCC |
CCA |
CLI |
Proposed Model |
|
|
30 |
74,8 |
39,5 |
92,7 |
15,6 |
61,4 |
|
60 |
28,3 |
56,2 |
81,9 |
43,7 |
96,1 |
|
90 |
33,4 |
78,2 |
58,9 |
47,6 |
19,3 |
|
120 |
54,1 |
66,8 |
21,7 |
85,4 |
32,9 |
|
150 |
41,3 |
88,5 |
34,6 |
17,9 |
72,2 |
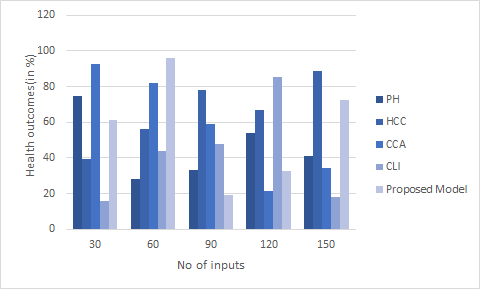
Figure 3. Computation of Health outcomes
In this field, goal setting should be SMART (Specific, Measurable, Attainable, Relevant and Time-bound), and tracking should be routine. It also requires a holistic solution, one that tackles both healthcare factors and social determinants of health, like income and education.
CONCLUSION
Several practical leadership strategies exist to mitigate healthcare disparities in urban settings. Second, the notion of collaborative leadership, in which a variety of stakeholders work together to help identify and address inequities, can produce solutions that are more comprehensive and sustainable. Second, transformational leadership, which elevates and energizes individuals toward achieving a shared vision, has the potential to enact systemic transformations in policies and practices. Third is culturally competent leadership, where leaders do their due diligence to understand and respond to the unique needs and challenges of diverse communities and can play a pivotal role in addressing disparities in marginalized populations. Finally, data-driven leadership can be used by leaders to find disparities and evaluate progress, which can lead to targeted interventions and measuring how effective interventions have been. Using these leadership strategies, healthcare systems and communities can strive to minimize healthcare disparities and facilitate health equity in urban environments.
REFERENCES
1. Williams, D. R., & Cooper, L. A. (2019). Reducing racial inequities in health: using what we already know to take action. International journal of environmental research and public health, 16(4), 606.
2. Merejo Medrano Y, González Duquesne I. Diagnosis of quality management in educational centers in the Dominican Republic. Journal of Scientific Metrics and Evaluation. 2024;2(1):151-7.
3. Weech-Maldonado, R., Dreachslin, J. L., Epané, J. P., Gail, J., Gupta, S., & Wainio, J. A. (2018). Hospital cultural competency as a systematic organizational intervention: Key findings from the national center for healthcare leadership diversity demonstration project. Health care management review, 43(1), 30-41.
4. Gómez Soto JA, Gómez Vergara FJ. Developing students’ scientific competencies using the school’s environmental context in rural and semi-rural settings. Journal of Scientific Metrics and Evaluation. 2024;2(1):89-115.
5. Mishra, V., Seyedzenouzi, G., Almohtadi, A., Chowdhury, T., Khashkhusha, A., Axiaq, A., ... & Harky, A. (2021). Health inequalities during COVID-19 and their effects on morbidity and mortality. Journal of healthcare leadership, 19-26.
6. Abreu Fuentes JR, Ponce Pastor RM. Pedagogical Tact: Phenomenology in Education from Community and Family Perspectives. Journal of Scientific Metrics and Evaluation. 2024;2(1):49-68.
7. Leal Filho, W., Balogun, A. L., Olayide, O. E., Azeiteiro, U. M., Ayal, D. Y., Muñoz, P. D. C., ... & Li, C. (2019). Assessing the impacts of climate change in cities and their adaptive capacity: Towards transformative approaches to climate change adaptation and poverty reduction in urban areas in a set of developing countries. Science of the Total Environment, 692, 1175-1190.
8. Shortell, S. M., Blodgett, J. C., Rundall, T. G., & Kralovec, P. (2018). Use of Lean and related transformational performance improvement systems in hospitals in the United States: results from a national survey. The Joint Commission Journal on Quality and Patient Safety, 44(10), 574-582.
9. Schell, C. J., Dyson, K., Fuentes, T. L., Des Roches, S., Harris, N. C., Miller, D. S., ... & Lambert, M. R. (2020). The ecological and evolutionary consequences of systemic racism in urban environments. Science, 369(6510), eaay4497.
10. Alarcón Osorio D, Gonzales Soria MB. Left-wing epistemology and right-wing ethics in public universities. Journal of Scientific Metrics and Evaluation. 2024;2(1):31-47.
11. Bhatt, J., & Bathija, P. (2018). Ensuring access to quality health care in vulnerable communities. Academic medicine, 93(9), 1271-1275.
12. Cyr, M. E., Etchin, A. G., Guthrie, B. J., & Benneyan, J. C. (2019). Access to specialty healthcare in urban versus rural US populations: a systematic literature review. BMC health services research, 19, 1-17.
13. Chiriboga, D., Garay, J., Buss, P., Madrigal, R. S., & Rispel, L. C. (2020). Health inequity during the COVID-19 pandemic: a cry for ethical global leadership. The Lancet, 395(10238), 1690-1691.
14. Velázquez-Hernández M, Marín González D, Paumier Durán AG, Carcasés Lores L, Landrove-Escalona EA, Godínez Linares R. Scientific production of Cardiology in Cuban student medical journals in the period 2019-2023. Journal of Scientific Metrics and Evaluation. 2024;2(1):137-50.
15. Blue Bird Jernigan, V., D’Amico, E. J., Duran, B., & Buchwald, D. (2020). Multilevel and community-level interventions with Native Americans: Challenges and opportunities. Prevention Science, 21(Suppl 1), 65-73.
FINANCING
None.
CONFLICTS OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Data curation: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Formal analysis: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Research: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Methodology: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Resources: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Software: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Supervision: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Validation: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Visualization: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Original drafting and editing: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.
Writing - proofreading and editing: Sukhman Ghumman, Prateek Aggarwal, Jamuna.K.V, Indu Singh, Tushar Pradhan, Rakhi Ludam, Vaishali V. Raje.