doi: 10.56294/hl2024.369
ORIGINAL
Leadership Strategies for Enhancing Healthcare Workforce Resilience
Estrategias de liderazgo para mejorar la resistencia del personal sanitario
Jagtej Singh1
![]() , Mohammad Asif2
, Mohammad Asif2
![]() , Swati Ingale3
, Swati Ingale3
![]() , Snehanshu Dey4
, Snehanshu Dey4
![]() , Anoop Dev5
, Anoop Dev5
![]() , Bharat Patil6
, Bharat Patil6
1Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
2School of Liberal Arts, Noida International University. Greater Noida, Uttar Pradesh, India.
3Krishna Institute of Nursing Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”. Taluka-Karad, Dist-Satara, Maharashtra, India.
4IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Psychiatry. Bhubaneswar, Odisha, India.
5Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
6Parul Institute of Management and Research-MBA, Parul University. Vadodara, Gujarat, India.
Cite as: Singh J, Asif M, Ingale S, Dey S, Dev A, Patil B. Leadership Strategies for Enhancing Healthcare Workforce Resilience. Health Leadership and Quality of Life. 2024; 3:.369. https://doi.org/10.56294/hl2024.369
Submitted: 05-03-2024 Revised: 23-07-2024 Accepted: 07-11-2024 Published: 08-11-2024
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: maintaining a skilled and effective healthcare workforce is essential for providing quality care to patients. The pace and stress of the current environment can make it difficult for healthcare professionals to maintain their resilience. Effective leadership strategies are crucial for driving up workforce resilience and helping healthcare professionals thrive.
Method: so, we conducted a thorough literature search, looking for examples of effective leadership approaches to building healthcare workforce resilience. Multiple databases, including PubMed, CINAHL, and PSYC INFO, were used for the literature search.
Results: we found that several of the strategies that were found to be effective in promoting resilience among the healthcare workforce included fostering a culture of support, encouragement, and empowerment; providing opportunities for self-care, relaxation, and stress management; promoting work-life balance; and ultimately, implementing communication training and mentorship. 4. They were found to improve the resilience of healthcare professionals and mitigate the adverse effects of burnout and stress.
Conclusions: leadership in promoting and normalizing resilience in the healthcare Workforce Understanding and taking action on the identified strategies will help leaders build a supportive working environment focused on improving both employee well-being and the quality of care delivered to patients. More research is warranted to ascertain both the effectiveness of such approaches and create evidence-informed recommendations to support organizational leaders in enhancing workforce resilience.
Keywords: Healthcare Workforce; Environment; Environment; Databases; Empowerment; Effectiveness.
RESUMEN
Introducción: mantener un personal sanitario cualificado y eficaz es esencial para prestar una atención de calidad a los pacientes. El ritmo y el estrés del entorno actual pueden dificultar que los profesionales sanitarios mantengan su resiliencia. Las estrategias de liderazgo eficaces son cruciales para aumentar la resiliencia del personal y ayudar a los profesionales sanitarios a prosperar.
Método: se realizó una búsqueda bibliográfica exhaustiva de ejemplos de enfoques de liderazgo eficaces para fomentar la resiliencia del personal sanitario. Para ello se utilizaron varias bases de datos, como PubMed, CINAHL y PSYC INFO.
Resultados: encontramos que varias de las estrategias que resultaron eficaces para promover la resiliencia entre el personal sanitario incluían fomentar una cultura de apoyo, estímulo y empoderamiento; proporcionar oportunidades para el autocuidado, la relajación y la gestión del estrés; promover el equilibrio entre el trabajo y la vida personal; y, por último, implementar capacitación en comunicación y tutoría. 4. Se constató que mejoran la resiliencia de los profesionales sanitarios y mitigan los efectos adversos del agotamiento y el estrés.
Conclusiones: liderazgo en el fomento y la normalización de la resiliencia en el personal sanitario Comprender las estrategias identificadas y adoptar medidas al respecto ayudará a los directivos a crear un entorno de trabajo propicio centrado en mejorar tanto el bienestar de los empleados como la calidad de la atención prestada a los pacientes. Es preciso seguir investigando para determinar la eficacia de estos enfoques y elaborar recomendaciones basadas en pruebas que ayuden a los responsables de las organizaciones a mejorar la resiliencia del personal.
Palabras clave: Personal Sanitario; Entorno; Bases de Datos; Empoderamiento; Eficacia.
INTRODUCTION
Unprecedented challenges, including the ongoing COVID-19 pandemic, workforce shortages, and rising pressure for quality care, mark the current healthcare landscape. Such challenges have put significant pressure on healthcare practitioners, contributing to high levels of stress, burnout, and turnover.(1) This indicates an increasing awareness of the importance of effective leadership strategies to help ensure the resilience of the healthcare workforce to safeguard their well-being and maintain the delivery of high-quality care. In this essay, we will discuss a few leadership strategies to leverage healthcare workforce resiliency.(2) Leaders are called to select and create a place for a culture of self-care in their organizations. Self-care is the steps that one takes—affirmatively— to take care of their mental, emotional, physical, and spiritual needs. Healthcare workers often prioritize the needs of others but at the cost of their well-being, resulting in burnout and lower job satisfaction.(3) Leaders have the opportunity to make a difference in this area by encouraging a culture of self-care, which helps employees strike a healthy balance between the demands of work and life, practice self-care, and nurture their well-being.(4) Giving wellness courses, making availability to mental health services available, and flexible working hours to support people on an individual basis can help. A key strategy to improving workforce resilience is leading and communicating well. Leadership is all about communication because effective communication is the basis for creating a positive relationship between managers and employees as well as among employees.(5) Team Communication Breakdown (In a crisis or under high-stress situations, communication can break down.(6) Leaders should promote an open communication environment where team members feel safe to express their concerns, feedback, and ideas. It enables the team to tackle problems in a team setting and make each other more resilient with a unified approach.(7) By cultivating a culture of ongoing learning and growth, leaders can foster resilience. As healthcare continues to evolve, employees need to grow and develop new skills to meet rapidly changing demands. Leaders can do this by creating opportunities for training, mentorship, and career development.(8) It increases the knowledge and assurance of the worker as well as provides a specific goal and satisfaction with their jobs. Leaders may also foster an environment that is innovative and creative so that workers are inspired to generate ideas to find solutions to problems.(9) Recognizing and finding ways to mitigate workplace stressors is also an act of leadership. It may be because of the workload, long working hours, and emotionally intense encounters with patients in the healthcare setting. Leaders should be conscious of these stressors and take steps to minimize their effects on the workforce.(10) This may involve uplifting work-life balance policies, appropriate staffing and resources, and creating a supportive and collaborative culture. Leaders could also offer debriefing sessions and ensure access to psychological in-house support services to help employee’s process burnout and compassion fatigue.(11) Best practices in leadership involve building a healthy and equitable working environment. A positive work culture increases the satisfaction, engagement, and general well-being of employees.(12) A thriving workplace culture instills a sense of psychological safety among employees, encouraging them to voice their opinions and take risks that result in greater levels of innovation and resilience. The main contribution of the paper has the following:
· Effective leaders can help enhance the emotional intelligence of healthcare workers by promoting self-awareness, empathy, and effective communication. This allows workers to better manage their emotions and respond healthily to stress, leading to increased resilience.(13)
· Good leaders can further increase the emotional intelligence of healthcare workers through self-awareness, empathy and effective communication. When workers manage their emotions and respond to stress constructively, they build resilience.(14)
· Leaders can also facilitate a supportive work environment. Providing access to resources, including counseling and other mental health services, enables healthcare workers to process experiences and build resilience. Leaders may also take initiatives and practices to encourage work-life balance and maintain a healthy work environment. Collective healthcare worker resilience is predicated upon effective team collaboration and teamwork. You can encourage this as a leader by creating a culture that promotes inclusivity, open dialogue, group collaboration, and recognizing and valuing the effort of every team member. It gives healthcare workers a sense of belonging and support, as well as an increased capacity to cope and recover from challenging situations.(15)
METHOD
Psychological resilience, which is the individual’s ability to deal with and recover from stressful situations such as COVID-19, has been discussed. Healthcare workers can keep their minds fit with coping behavior, seeking support from others, and self-care. Colleagues, friends, and family support can also help take stress off during this testing time. Thomas, S., et al. Strengthening health system resilience has been discussed by a study. It can be realized through strong infrastructure, sufficient resources, an agile management structure, and strategic partnerships. Albott, C. S., et al. Seek & discuss context among healthcare workers facing the expectations of battle buddies as a rapid response intervention geared towards bolstering the mental health and resilience of healthcare workers during the COVID-19 pandemic. It involves pairing or assigning partners or “battle buddies” for social support and coping strategies. The goal of this intervention is to reduce the potential adverse psychological consequences of hostile work conditions. Crane, M. F., et, al. with: Developing resilience of first responders is a process of equipping first responders with psychoeducation services that allow them to handle the stresses and trauma encountered during their job duration. This can be in terms of learning self-care practices, stress management skills, or finding their balance in healthy social connections while improving their mental and emotional health. A study have explored how Innovation leadership is instrumental in leveraging big data analytics for creating resilient healthcare supply chains in the context of the COVID-19 pandemic. In this way, processes of data-driven strategies will be improved, opportunities for innovations will be identified, and solutions will be developed to achieve maximized supply chain efficiency, which will also contribute to effective management and response during a pandemic situation.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Labrague, L. J. et,al. |
2021 |
One advantage is that it decreases the negative impact of stress and improves the overall well-being of health care workers. |
Potential influence of individual characteristics and resources on the effectiveness of coping mechanisms. |
|
Thomas, S., et,al. |
2020 |
Improved preparedness for unexpected events and ability to adapt and respond effectively to health challenges, leading to better overall health outcomes. |
Possible overemphasis on infrastructure rather than addressing underlying social and economic determinants of health. |
|
Albott, C. S., et,al. |
2020 |
Constant emotional support and companionship to help reduce stress and improve mental health of health care workers. |
Lack of personalized approach due to group interventions may not address individualized needs and experiences. |
|
Crane, M. F., et,al. |
2022 |
Increased ability to cope with high levels of stress and maintain mental health, resulting in more effective and efficient service delivery. |
Overcoming cultural and personal barriers to accessing and utilizing psychoeducational services. |
|
Bag, S., et,al. |
2021 |
More efficient and effective allocation of resources and identification of potential supply chain disruptions. |
Potential lack of access to necessary technology or data among certain healthcare systems or regions. |
|
Finstad, G. L., et,al. |
2021 |
Improved employee well-being and productivity through enhanced ability to handle challenges and bounce back from adversity. |
Subjectivity of individual experiences and effectiveness of strategies may vary, leading to inconsistent outcomes. |
|
Everly Jr, G. S., et,al. |
2022 |
Effective leadership can instill a sense of hope, stability, and motivation, leading to decreased levels of anxiety and stress among individuals. |
Inability to address individual variations in response to stress and trauma. |
|
Grimm, P. Y., et,al. |
2021 |
Improved ability to identify and address key factors contributing to resilience and ultimately improve health outcomes. |
Limited access to data and resources on health systems in low-and middle-income countries. |
|
Schreiber, M., et,al. |
2019 |
Reducing staff burnout and improving job satisfaction, leading to a more sustainable and effective healthcare workforce. |
Lack of adequate resources to implement and sustain comprehensive resilience programs for healthcare workers. |
|
Henshall, C., et,al. |
2020 |
Enhancing emotional and mental well-being, leading to improved job satisfaction and retention rates among nurses. |
Insufficient evidence on long-term effectiveness and scalability of resilience interventions in diverse healthcare settings. |
Finstad, G. L., et,al. Resilience is the ability of individuals to adapt and recover from challenges or traumatic experiences. Coping strategies are techniques people use to deal with and cope with stressors. Posttraumatic growth refers to the positive psychological changes that may arise in a workplace environment after experiencing a traumatic event, such as the COVID-19 pandemic. A study have discussed The fear and uncertainty related to disasters like COVID-19 can automatically result in psychological casualties: anxiety, trauma, and depression. To reduce these, one can have clear and accurate information, promote social support and resilience and provide mental health services for those in need. Grimm P. Y. et al. highlighted that the one aspect of resilience in low- and middle-income country healthcare systems is essential to pragmatism to respond to shocks and function. This includes understanding the capacity of these systems, considering their strengths and vulnerabilities, and determining the way(s) in which they can be adapted and sustained. Schreiber, M., et,al. Scholars such as Brubaker et al. have argued that building the resilience of healthcare workers during multi-hazard events requires systematic efforts to provide both social and structural resources, including access to mental health support, training and resources, effective communication and coordination systems, and contingency plans. It prepares them to cope with multiple hazards, thus protecting their well-being and ensuring the ability to provide quality care. Henshall, C., et, al. Nursing resilience interventions involve the use of various efforts and interventions that empower and safeguard nurses in challenging healthcare environments such as highly demanding, highly stressful and high-risk environments. Nurse coping interventions are intended to help nurses cope with challenging scenarios as well as provide pathways for optimal functioning during care provision to ensure patient needs are adequately met.
DEVELOPMENT
Leadership Strategies for Enhancing Healthcare Workforce Resilience Overview. The development would provide current and future healthcare leaders with the knowledge and skills needed to guide their teams through difficult times successfully. Thus, creating resilience in the healthcare workforce, which is vital considering the need faced by COVID-19 and similar potential crises in the near future, will be the focus of this development program. The completion of the program will allow leaders to be well-versed in the concept of resilience and its significance in a healthcare setting, along with their hands-on experience with the tools and methods to shape and develop resilience in their healthcare teams. Topics will cover creating a supportive and psychologically safe environment, communicating and solving problems through a crisis and leader self-care, to name a few. The development program will be executed through virtual and in-person workshops, interactive movements, and case studies. It will also include personalized coaching and mentoring so that leaders can implement what they learned on the job in their particular workspace. Healthcare leaders who build resilience in their teams will be better able to meet the challenges and uncertainties that lie ahead, ultimately enhancing the ability of our institutions to deliver quality care to our patients while creating a more positive and supportive work environment for our staff. Figure 1 shows the Proposed Development Model.
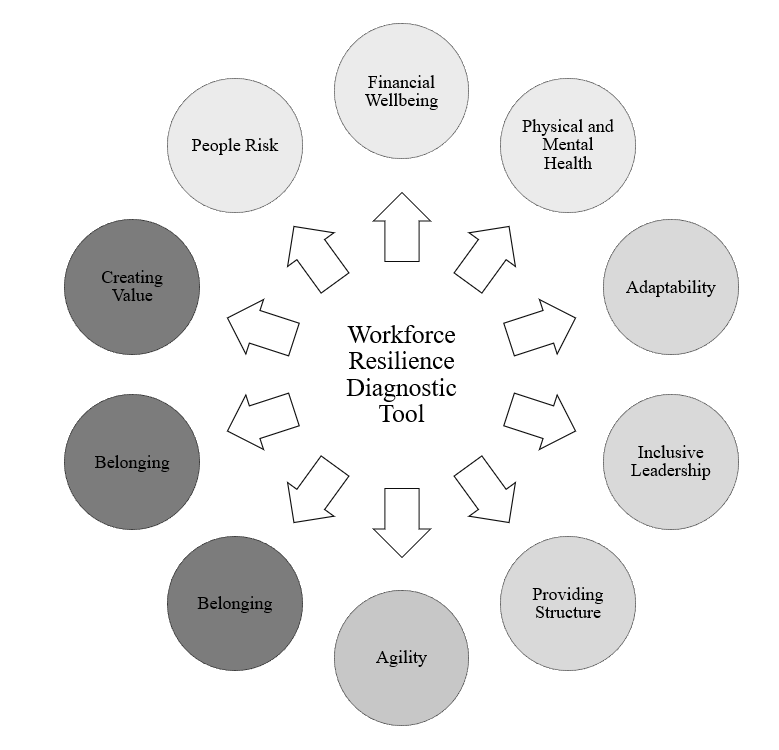
Figure 1. Proposed Development Model
The Workforce Resilience Diagnostic Tool is a thorough and organized method for measuring and enhancing the overall robustness of a workforce. It is held to assist organizations in pinpointing the key areas of strength and the potential problems that they face. It helps them in developing a more resilient and adaptive workforce. The tool has five primary dimensions: Financial well-being, physical and mental health, value creation, belonging, and adaptability. Understanding the economic conditions and securities (such as salaries, benefits and opportunities for economic growth and stability) of employees falls under the purview of Financial Well-being. This factor also takes into account whether resources are available for employees to oversee their finances and strategize for their financial future. Physical and Mental Health the physical and psychological well-being of employees. It includes their physical health access to health care, the opportunity for exercise — and their mental health support for managing stress and time for work-life balance. Creating Value concentrates on the enterprise’s culture and leadership and what they do to create a feeling of purpose and meaning for employees. This dimension also measures the organization’s dedication toward diversity, inclusion, employee recognition, and development. Belonging measures the sense of community and togetherness within the organization, including trust and collaboration between team members. This includes the extent to which policies and practices are inclusive. Adaptability and Agility are essential attributes in building a resilient workforce; the world is changing, and so should organizations. This dimension measures the organization’s agility to change and adapt swiftly and to what extent employees are supported and resourced during change initiatives.
RESULTS AND DISCUSSION
This study used a descriptive qualitative method to examine leadership strategies to strengthen resilience among healthcare workers based on a review of the literature. Revelations in favor of how impactful leadership can improve resilience in clinical staff. The results were discussed with a great emphasis on the potential benefits of strong and supportive leadership in the workplace and how this ultimately creates a positive culture in which employees feel valued and empowered. This includes clear lines of communication, resources for dealing with stress and burnout and building a supportive and team-oriented culture. A key challenge faced by healthcare leaders was a need to acknowledge and address the challenges and stressors that are unique to healthcare workers, including long working hours and high workloads, exposure to traumatic events, workload stressors and signs of burnout. These strategies included implementing employee wellness programs, providing mental health support, promoting work-life balance and demonstrating success in building resilience. This illustrates the need for strong leadership, thus promoting resilience within healthcare workers, enhancing workplace job satisfaction and retention, and ultimately resulting in improved quality patient care.
Employee Retention Rate
The employee retention rate refers to the percentage of employees retained in an organization over some time. This rate reflects the effectiveness of leadership strategies related to improving healthcare workforce resilience and retaining employees in the healthcare workforce. You can calculate it by taking the Number of employees retained by a company and dividing it by the total employees at the beginning of the period.
|
Table 2. Comparison of Employee Retention Rate |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
RHCM |
RLM |
BRM |
PORM |
Proposed Model |
|
|
30 |
29 |
33 |
42 |
58 |
63 |
|
60 |
25 |
32 |
47 |
50 |
68 |
|
90 |
28 |
34 |
52 |
61 |
80 |
|
120 |
21 |
38 |
45 |
57 |
86 |
|
150 |
27 |
31 |
46 |
54 |
87 |
Such strategies could involve improving the organizational environment, creating career development opportunities, or encouraging a healthy work-life balance to increase the resilience of the healthcare workforce. Figure 2 shows the computation of Employee Retention Rate.
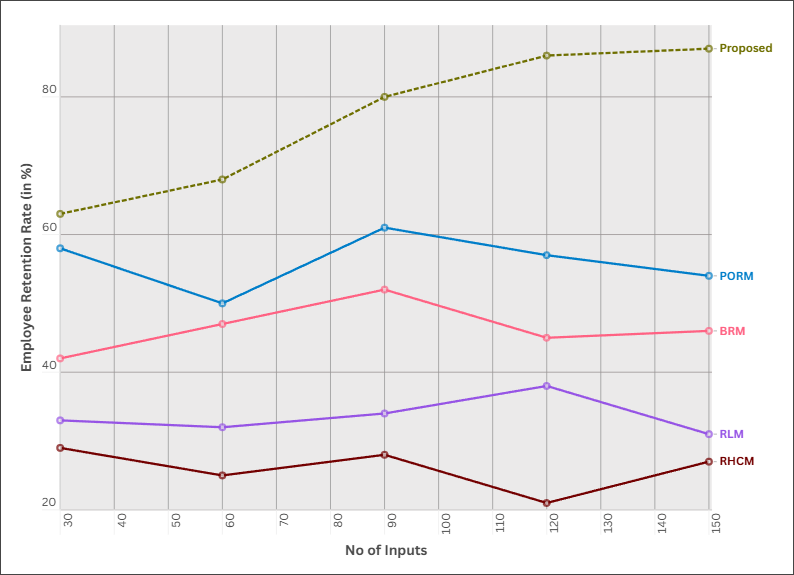
Figure 2. Computation of Employee Retention Rate
These approaches foster greater job satisfaction and lower turnover rates as employees feel valued, motivated, and supported. One example of this can be seen in retaining a higher percentage of employees, as they feel more motivated through continuous training, which allows employees to deal with complex scenarios that will arise in the workplace.
Employee Engagement
Employee engagement is defined as the emotional and intellectual commitment an employee has to their work, coworkers, and the company. Healthcare workers who feel engaged with their work are able to maintain a sense of purpose, which, according to this study, is just one way of promoting resilience in the healthcare workforce.
|
Table 3. Comparison of Employee Engagement |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
RHCM |
RLM |
BRM |
PORM |
Proposed Model |
|
|
100 |
100 |
4 |
18 |
10 |
13 |
|
200 |
200 |
5 |
22 |
12 |
14 |
|
300 |
300 |
6 |
23 |
11 |
16 |
|
400 |
400 |
7 |
21 |
15 |
17 |
|
500 |
500 |
8 |
25 |
19 |
20 |
Leadership strategies to improve resilience in the healthcare workforce often include fostering a positive work environment, promoting open communication and collaboration among staff, offering opportunities for professional development and growth, and recognizing and rewarding individuals for their contributions to the organization. Figure 3 shows the computation of Employee Engagement.
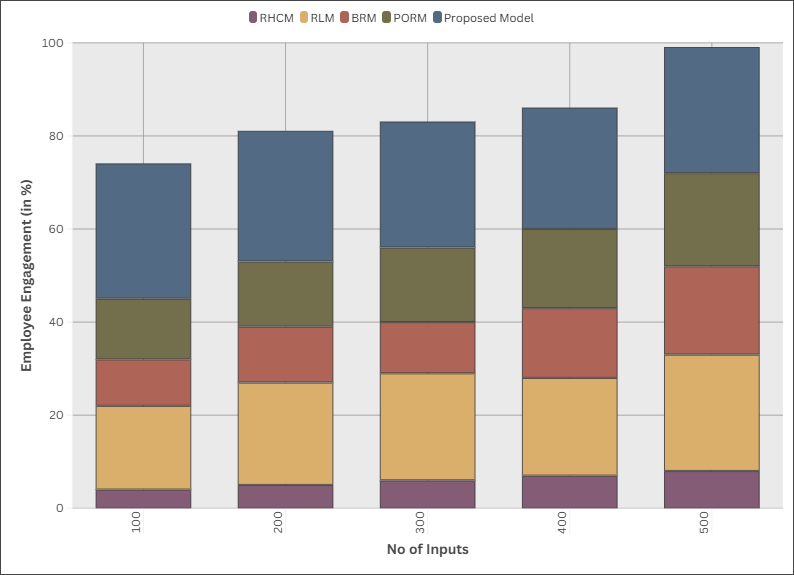
Figure 3. Computation of Employee Engagement
By engaging employees to co-create workplace strategies in alignment with the culture they are building, they foster trust and a sense of shared responsibility, which, in turn, engenders even higher levels of engagement and resilience. In addition, employee feedback in times of crisis and during the recovery phase has equal contributions toward a resilient workforce.
Burnout Rates
Healthcare worker burnout remains a serious problem, with an estimated 40 % of doctors and 35 % of nurses burning out. Fighting with long working times, high patient volume, under-resourced and under-supported, it can be a jungle book. Research indicates that implementing leadership strategies can help bolster healthcare workforce resilience and address burnout.
|
Table 4. Comparison of Burnout Rates |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
RHCM |
RLM |
BRM |
PORM |
Proposed Model |
|
|
5 |
49 |
44 |
71 |
96 |
13 |
|
10 |
53 |
37 |
77 |
94 |
25 |
|
15 |
36 |
29 |
39 |
89 |
48 |
|
20 |
43 |
41 |
80 |
91 |
76 |
|
25 |
51 |
45 |
66 |
87 |
98 |
Such strategies involve encouraging a healthy work-life balance, creating a constructive work environment, offering career advancement opportunities, and ensuring stress-relief programs. Figure 4 shows the computation of Burnout Rates.
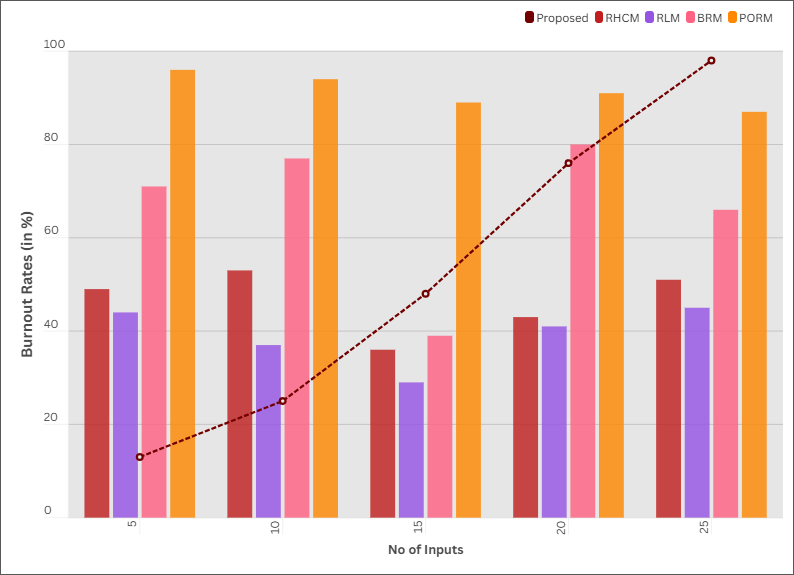
Figure 4. Computation of Burnout Rates
Asking employees to help make decisions and noting work factors that induce stress can boost resilience and reduce burnout rates. Patient care quality depends on these organizational leadership ways of working, which are top agenda items.
CONCLUSIONS
Leadership strategies are key in fortifying the resilience of the healthcare workforce. Resilience is the power to recover from obstacles and adapt to new situations. It is essential to lakhs of healthcare workers who enter high-stress and burn-out healthcare set-up every day. Strategies for effective leadership to promote resilience may include creating a positive work culture, providing support and resources to staff, encouraging self-care, and implementing strategies for managing work-related stress. A positive work culture also contributes towards a supportive environment for healthcare workers, which may be encouraged through leadership. This is accomplished by providing channels for open communication, promoting cooperation, and acknowledging the efforts of the employees. Show Support and Encourage Self-Care: To reduce burnout and improve well-being, support individual self-care through mental health resources and flexible work schedules. Additionally, these can be collected in the form of debriefings and coping mechanisms training, which strengthens the resiliency of the HCWs. They should also help establish a safe and inclusive workplace to foster trust and decrease stigma on mental health. Leadership strategies that promote a healthy work culture, support for self-care, and work-related stress management contribute to the resilience of the healthcare workforce, which directly impacts the quality of care provided to our patients.
BIBLIOGRAPHIC REFERENCES
1. Labrague, L. J. (2021). Psychological resilience, coping behaviours and social support among health care workers during the COVID‐19 pandemic: A systematic review of quantitative studies. Journal of nursing management, 29(7), 1893-1905.
2. Acevedo-Osorio GO, Trujillo-Trejos I, Ramírez-Echeverry MY. Knowledge, attitudes, and practices regarding the prevention of human papillomavirus in school students, Pereira-Colombia. Scientific Journal Care & Tech. 2024;2(2):23-39.
3. Thomas, S., Sagan, A., Larkin, J., Cylus, J., Figueras, J., & Karanikolos, M. (2020). Strengthening health systems resilience: key concepts and strategies.
4. Cano Turnes MA. Multidimensional Strategies to Promote and Sustain Exclusive Breastfeeding in Clinical Practice. Scientific Journal Care & Tech. 2024;2(2):52-63.
5. Albott, C. S., Wozniak, J. R., McGlinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020). Battle buddies: rapid deployment of a psychological resilience intervention for health care workers during the COVID-19 pandemic. Anesthesia & Analgesia, 131(1), 43-54.
6. Crane, M. F., Falon, S. L., Kho, M., Moss, A., & Adler, A. B. (2022). Developing resilience in first responders: Strategies for enhancing psychoeducational service delivery. Psychological services, 19(S2), 17.
7. Martínez Barra CA. Personal and Technical Profile of Psychotherapists: An Analysis of Competencies and Challenges. Scientific Journal Care & Tech. 2024;2(2):80-104.
8. Bag, S., Gupta, S., Choi, T. M., & Kumar, A. (2021). Roles of innovation leadership on using big data analytics to establish resilient healthcare supply chains to combat the COVID-19 pandemic: A multimethodological study. IEEE Transactions on Engineering Management.
9. Finstad, G. L., Giorgi, G., Lulli, L. G., Pandolfi, C., Foti, G., León-Perez, J. M., ... & Mucci, N. (2021). Resilience, coping strategies and posttraumatic growth in the workplace following COVID-19: A narrative review on the positive aspects of trauma. International journal of environmental research and public health, 18(18), 9453.
10. Alastre Arape YJ. Systematization of the nursing care process. Scientific Journal Care & Tech. 2024; 2(1):19-3.
11. Everly Jr, G. S., Wu, A. W., Cumpsty-Fowler, C. J., Dang, D., & Potash, J. B. (2022). Leadership principles to decrease psychological casualties in COVID-19 and other disasters of uncertainty. Disaster Medicine and Public Health Preparedness, 16(2), 767-769.
12. Grimm, P. Y., Oliver, S., Merten, S., Han, W. W., & Wyss, K. (2021). Enhancing the understanding of resilience in health systems of low-and middle-income countries: a qualitative evidence synthesis. International Journal of Health Policy and Management, 11(7), 899.
13. Sánchez MB. Nursing Care in the Management of Patients with Chronic Diseases . Scientific Journal Care & Tech. 2024; 2(1):40-58
14. Schreiber, M., Cates, D. S., Formanski, S., & King, M. (2019). Maximizing the resilience of healthcare workers in multi-hazard events: lessons from the 2014–2015 Ebola response in Africa. Military medicine, 184(Supplement_1), 114-120.
15. Henshall, C., Davey, Z., & Jackson, D. (2020). Nursing resilience interventions–A way forward in challenging healthcare territories. Journal of Clinical Nursing, 29(19-20), 3597.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Jagtej Singh, Mohammad Asif, Swati Ingale, Snehanshu Dey, Anoop Dev, Bharat Patil.
Methodology: Jagtej Singh, Mohammad Asif, Swati Ingale, Snehanshu Dey, Anoop Dev, Bharat Patil.
Software: Jagtej Singh, Mohammad Asif, Swati Ingale, Snehanshu Dey, Anoop Dev, Bharat Patil.
Drafting - original draft: Jagtej Singh, Mohammad Asif, Swati Ingale, Snehanshu Dey, Anoop Dev, Bharat Patil.
Writing - proofreading and editing: Jagtej Singh, Mohammad Asif, Swati Ingale, Snehanshu Dey, Anoop Dev, Bharat Patil.