doi: 10.56294/hl2024.367
ORIGINAL
Quality of Life Outcomes in Chronic Disease Management: A Leadership Perspective
Resultados de calidad de vida en la gestión de enfermedades crónicas: Una perspectiva de liderazgo
Shardha Purohit1
![]() ,
Dhruvin Chauhan2
,
Dhruvin Chauhan2 ![]() ,
Jitendriya Biswal3
,
Jitendriya Biswal3 ![]() ,
Simranjeet Nanda4
,
Simranjeet Nanda4 ![]() ,
Bharat Bhushan5
,
Bharat Bhushan5 ![]() ,
Bhupal Pujari6
,
Bhupal Pujari6 ![]()
1SJMC, Noida International University, Greater Noida, Uttar Pradesh, India.
2Parul Institute of Management and Research-MBA, Parul University, Vadodara, Gujarat, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Psychiatry, Bhubaneswar, Odisha, India.
4Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
5Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
6Krishna Institute of Medical Sciences, Krishna Vishwa Vidyapeeth “Deemed to be University”, Dept. of Medicine, Taluka-Karad, Dist-Satara, Maharashtra, India.
Cite as: Purohit S, Chauhan D, Biswal J, Nanda S, Bhushan B, Pujari B. Quality of Life Outcomes in Chronic Disease Management: A Leadership Perspective. Health Leadership and Quality of Life. 2024; 3:.367. https://doi.org/10.56294/hl2024.367
Submitted: 09-03-2024 Revised: 26-07-2024 Accepted: 21-11-2024 Published: 22-11-2024
Editor:
PhD. Prof. Neela Satheesh
![]()
ABSTRACT
Introduction: this study aimed to explore the perspectives of leaders in chronic disease management and the impact of their leadership practices on the quality of life outcomes for patients with chronic diseases.
Method: a sample of leaders working in chronic disease management were interviewed qualitatively, transcribed, and analysed thematically.
Results: leaders identified several key ways in which their leadership practices influenced the quality of life outcomes for chronic disease patients. These included providing support and resources for patients, implementing multidisciplinary care teams, promoting patient empowerment and self-management, and fostering a culture of collaboration and continuous improvement. Leaders also recognized the importance of their well-being and self-care in effectively managing chronic diseases and promoting quality of life for patients.
Conclusions: leaders play a critical role in shaping the quality of life outcomes for patients with chronic diseases. By implementing effective leadership practices, such as providing support and resources, promoting self-management, and fostering collaboration, leaders can help improve the overall well-being of patients with chronic diseases. Moreover, leaders should prioritize their well-being and self-care in order to better support and lead their care teams and ultimately improve the quality of life for chronic disease patients. This study highlights the importance of leadership in chronic disease management and provides valuable insights for leaders to enhance their practices and ultimately improve patient outcomes.
Keywords: Disease Management; Chronic Disease; Empowerment; Self-Management.
RESUMEN
Introducción: este estudio pretendía explorar las perspectivas de los líderes en la gestión de enfermedades crónicas y el impacto de sus prácticas de liderazgo en los resultados de la calidad de vida de los pacientes con enfermedades crónicas.
Método: una muestra de líderes que trabajan en la gestión de enfermedades crónicas fueron entrevistados cualitativamente, transcritos y analizados temáticamente.Resultados: los líderes identificaron varias formas clave en las que sus prácticas de liderazgo influían en los resultados de la calidad de vida de los pacientes con enfermedades crónicas. Entre ellas se incluían proporcionar apoyo y recursos a los pacientes, implantar equipos de atención multidisciplinares, promover la capacitación y la autogestión de los pacientes y fomentar una cultura de colaboración y mejora continua. Los líderes también reconocieron la importancia de su bienestar y autocuidado para gestionar eficazmente las enfermedades crónicas y promover la calidad de vida de los pacientes.
Conclusiones: los líderes desempeñan un papel fundamental en la configuración de los resultados de la calidad de vida de los pacientes con enfermedades crónicas. Mediante la aplicación de prácticas de liderazgo eficaces, como proporcionar apoyo y recursos, promover la autogestión y fomentar la colaboración, los líderes pueden ayudar a mejorar el bienestar general de los pacientes con enfermedades crónicas. Además, los líderes deben priorizar su bienestar y autocuidado para apoyar y liderar mejor a sus equipos asistenciales y, en última instancia, mejorar la calidad de vida de los pacientes con enfermedades crónicas. Este estudio pone de relieve la importancia del liderazgo en la gestión de las enfermedades crónicas y proporciona valiosas ideas para que los líderes mejoren sus prácticas y, en última instancia, mejoren los resultados de los pacientes.
Palabras clave: Gestión de enfermedades; Enfermedad crónica; Empoderamiento; Autogestión.
INTRODUCTION
Chronic diseases, such as diabetes, heart disease, and cancer, have become increasingly prevalent in our society.(1) These conditions have a significant impact not only on an individual’s physical health but also on their overall quality of life. Effective management of chronic diseases is essential to improve quality of life outcomes for individuals and reduce the burden on the healthcare system. In this essay, we will explore the role of leadership in chronic disease management and how it can contribute to improving quality of life outcomes.(2) Leadership plays a critical role in chronic disease management as it sets the direction, vision, and tone of a healthcare organization. Effective leadership in this context requires a strong understanding of the complexity of chronic diseases and the challenges associated with their management. It also requires skills such as communication, collaboration, and strategic thinking to identify and implement solutions that can improve quality of life outcomes for individuals with chronic diseases.(3) One of the key aspects of leadership in chronic disease management is creating an environment that promotes patient-centered care. This approach involves engaging patients in their own care and decision-making processes, understanding their unique needs and preferences, and providing support to help them manage their condition effectively.(4) It not only improves the overall quality of care but also empowers patients to take an active role in their health, leading to better health outcomes and an improved quality of life. Effective leadership in chronic disease management also involves a multi-disciplinary team approach.(5) Chronic diseases often require a holistic approach involving various healthcare professionals such as physicians, nurses, dieticians, and social workers. A strong leader can bring these professionals together and facilitate effective communication and collaboration to develop comprehensive care plans for patients. Such an approach improves coordination and continuity of care, leading to better health outcomes and an enhanced quality of life. Another crucial aspect of leadership in chronic disease management is the implementation of evidence-based practices and processes.(6) Chronic diseases are complex and require specific treatment plans tailored to each individual. Leaders must ensure that their healthcare organization stays up-to-date with the latest research and best practices in managing chronic diseases. It involves continuous education and training for healthcare professionals, as well as incorporating new technologies and tools that can facilitate effective chronic disease management. By staying current with evidence-based practices, leaders can ensure that their healthcare organization delivers high-quality care and ultimately improves the quality of life for individuals with chronic diseases. Effective leadership in chronic disease management involves a focus on prevention and early intervention.(7) Chronic diseases are often preventable or can be effectively managed if identified and treated early. Leaders play a crucial role in promoting population health and implementing preventative measures such as education, screenings, and lifestyle interventions. By identifying and addressing risk factors early on, leaders can prevent the development of chronic diseases and improve the overall quality of life for individuals and their communities. Leadership in chronic disease management must also address the social determinants of health that can impact an individual’s quality of life.(8) Factors such as income, education, and access to resources can have a significant impact on an individual’s ability to manage their chronic disease effectively. Leaders must advocate for policies and initiatives that address these social determinants of health and promote health equity for all individuals, regardless of their socioeconomic status. By addressing these fundamental issues, leaders can help create a more equitable healthcare system and improve quality of life outcomes for individuals with chronic diseases.(9) Leadership plays a critical role in chronic disease management and has a significant impact on quality of life outcomes. By creating patient-centered, multi-disciplinary, evidence-based, and preventative approaches to chronic disease management, leaders can improve the overall quality of care and empower individuals to take an active role in their health. Additionally, addressing social determinants of health and promoting health equity are essential aspects of effective leadership in this context.(10) As we continue to face the challenges of managing chronic diseases, strong leadership is crucial in improving quality of life outcomes for individuals and creating a healthier society. The main contribution of the paper has the following:
• The patient’s overall quality of life rather than just their specific disease or symptoms, healthcare providers can ensure comprehensive and tailored care that addresses all aspects of the patient’s well-being. It can lead to better disease management, reduced hospital readmissions, and improved overall health and satisfaction for patients.
• Quality-of-Life measures into their decision-making processes, leaders can better understand their patients’ needs and priorities and implement strategies for optimal disease management. This can lead to improved patient trust and satisfaction and a more positive and supportive healthcare culture.
• Focusing on quality of life outcomes in chronic disease management can also lead to cost savings for healthcare systems. By effectively managing chronic conditions and improving overall patient health, healthcare organizations can reduce the need for expensive interventions and treatments.
Researchers(1) have discussed the COVID-19 pandemic and subsequent social distancing measures have significantly impacted the economic well-being and quality of life of Vietnamese citizens. Many have lost their jobs or experienced reduced income, leading to financial struggles and increased poverty. Social isolation and disrupted routines have also affected mental health and social connections. A research(2) discuss that the Geriatric Cardiology Section Leadership Council is a committee within the American College of Cardiology that focuses on issues related to cardiovascular care in older adults. Comprised of experts in the field, the council works to advance research, education, and advocacy efforts to improve the care of older patients with heart disease. Neuhouser, (3)have discussed that a balanced and nutritious diet plays a crucial role in preventing chronic diseases such as obesity, heart disease, and diabetes. A healthy dietary pattern consisting of a variety of whole foods can help maintain a healthy weight, lower blood pressure and cholesterol levels, and reduce the risk of developing lifestyle-related chronic illnesses. (4)have discussed measuring and improving the quality of mental health care, which involves evaluating the effectiveness, safety, timeliness, efficiency, and patient-centeredness of services. It is done through various measures such as patient outcome measures, system-level audits, and patient satisfaction surveys. Continuous efforts are made to enhance the quality of care and ensure it meets global standards. (5)have discussed the durability of clinical and quality-of-life outcomes of closed-loop spinal cord stimulation for chronic back and leg pain, which was evaluated in a secondary analysis of the evoke randomized clinical trial. The results showed that the treatment provided long-term benefits for patients and improved their overall quality of life.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Tran, B. X et al.(1) |
2018 |
Greater appreciation for local businesses and self-sufficiency as people turn to domestic products and services during the lockdown. |
Reduced income and job losses led to financial insecurity and stress for Vietnamese citizens during the national social distancing period. |
|
Gorodeski, E. Z et al.(2) |
2020 |
Expert oversight and guidance in promoting quality care for elderly patients with cardiovascular disease. |
Limited inclusion of geriatric specialists in leadership positions may hinder a comprehensive understanding of issues affecting older cardiovascular patients. |
|
Neuhouser, M. L et al.(3) |
2019 |
Preventing chronic diseases through healthy diets can improve overall health and reduce the risk of developing life-threatening conditions. |
Difficulty in implementing and maintaining healthier dietary habits due to individual preferences, cultural influences, and affordability. |
|
Kilbourne, A. M et al.(4) |
2018 |
Enhanced and more effective treatment outcomes for individuals suffering from mental health issues worldwide. |
One limitation is that quality standards may vary across different cultures and may not be readily applicable globally. |
|
Mekhail, N et al.(5) |
2022 |
Long-term effectiveness of pain relief and improved quality of life for individuals with chronic back and leg pain. |
Limited long-term data on the effectiveness and durability of closed-loop spinal cord stimulation for chronic pain management. |
|
Poot, C. C et al.(6) |
2021 |
The use of multiple treatment approaches can improve symptom management and overall quality of life for COPD patients. |
Integration of interventions may not be feasible or favorable for all individuals, limiting effectiveness and patient adherence. |
|
Ysrraelit, M. C et al.(7) |
2018 |
Identifying areas of discrepancy between patients and neurologists can lead to more personalized and effective treatment plans. |
The difference in perception may not always reflect the true impact of the disease on the patient’s life. |
|
Yu, C. P et al.(8) |
2018 |
Increased economic opportunities and potential for growth, leading to a stronger and more sustainable local economy. |
One limitation is that residents’ perception of tourism impacts may not accurately reflect the actual effect on community quality of life. |
|
Arsenault-Lapierre, G et al.(9) |
2021 |
Hospital-at-home interventions result in lower hospital readmission rates and reduced risk of hospital-acquired infections, resulting in cost savings. |
Lack of long-term follow-up data on patient outcomes after returning to their home environment. |
|
Javaid, Z. K et al.(10) |
2023 |
Reduces workplace stress and improves quality of life, leading to better mental and physical health. |
Difficulty generalizing findings; the sample may not represent all working women or different professional fields. |
(6)have discussed integrated disease management interventions for patients with chronic obstructive pulmonary disease, which involve a multi-faceted approach that combines pharmacological treatments, non-pharmacological therapies, and self-management strategies. These interventions address the physical, psychological, and social aspects of COPD, aiming to improve symptoms, reduce exacerbations, and enhance the overall quality of life for patients. (7)have discussed that quality of life assessment in multiple sclerosis is a way to evaluate the physical, mental, and emotional well-being of patients with this chronic neurological disease. However, studies have shown that patients and neurologists have different perceptions of what constitutes a good quality of life, which can affect treatment plans and overall management of the disease. (8)have discussed that many rural communities in the Midwest (USA) are increasingly turning to tourism as a means of economic development. The support of residents for this development is crucial, as their perception of the impacts of tourism and its effects on their overall quality of life can significantly influence the success of tourism initiatives. (9)have discussed this systematic review and meta-analysis, comparing the effectiveness of hospital-at-home interventions versus in-hospital stays for patients with chronic diseases who are presented to the emergency department. The findings suggest that HAH interventions may have potential benefits in terms of patient satisfaction, costs, and outcomes compared to traditional in-hospital care. (10)have discussed the mediating role of mindfulness, which refers to how the practice of being present and self-aware can help working women cope with workplace stress and improve their overall quality of life. Mindfulness acts as a mediator by reducing the negative impact of stress on a woman’s well-being and allowing her to maintain a healthier work-life balance.
METHOD
The proposed methods aim to address the need for improved quality-of-life outcomes in chronic disease management through a leadership perspective. It will focus on developing the skills, knowledge, and attitudes of healthcare leaders in effectively managing chronic diseases to improve patients’ overall well-being and quality of life. The development will involve conducting educational programs, workshops, and training sessions for healthcare leaders to gain a better understanding of chronic diseases, their impact on patients, and the importance of taking a patient-centered approach to managing them. These programs will also equip leaders with the necessary skills to effectively communicate with patients, set realistic goals, and develop personalized care plans. The development will provide resources and tools for healthcare leaders to implement evidence-based practices in chronic disease management, such as patient education, self-management techniques, and collaborative care approaches. It will also emphasize the need for continuous monitoring and evaluation of patient outcomes to identify areas for improvement and adjust care plans accordingly. The development will focus on building a supportive and collaborative healthcare team involving not only clinicians but also patients, caregivers, and community resources. This approach will foster a holistic and patient-centered approach to chronic disease management, which has been shown to improve quality of life outcomes. Figure 1 shows the development model.
It includes functions such as breathing, digestion, circulation, elimination, and hormone regulation. These functions are controlled by the body’s nervous, endocrine, and immune systems, which work together to maintain balance and keep the body functioning optimally. If any of these systems are not functioning correctly, it can lead to various health issues and impairments. A person’s social interaction can be impacted by their physical, psychological, and cognitive health. Someone with a physical disability may have difficulty participating in certain social activities. Someone with a mental health disorder may struggle with emotional regulation and forming connections with others. Factors such as access to healthcare, employment opportunities, social support, and personal fulfillment play a significant role in determining one’s quality of life. Changes in any of these areas can impact a person’s overall sense of well-being. Various factors, including congenital conditions, injuries, or chronic health conditions, can cause these disabilities. Functional disabilities can impact a person’s mobility, communication, cognition, and self-care abilities, making it challenging to navigate their daily lives independently. Symptoms vary in severity and can impact an individual’s daily functioning and quality of life. They are often used to diagnose and monitor health conditions and can be managed through various interventions such as medication, therapy, or lifestyle changes.
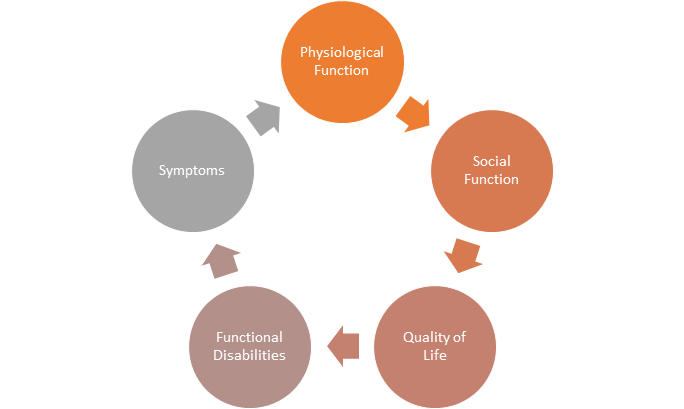
Figure 1. Development model
RESULTS AND DISCUSSION
The study found that effective leadership in healthcare organizations plays a crucial role in ensuring better quality-of-life outcomes for patients with chronic diseases. The results of the study showed that leaders who prioritized patient-centered care, effective communication, and collaboration among healthcare professionals were able to improve treatment outcomes and overall quality of life for patients. Furthermore, the study highlighted the importance of providing resources and support to patients, such as education about their condition and access to community resources, which can also positively impact their quality of life. The discussion highlights the significance of leadership in healthcare and its impact on chronic disease management. The findings suggest that a patient-centered approach to care, where the needs and preferences of patients are prioritized, can lead to improved outcomes and better quality of life. This study adds to the growing body of research on the importance of effective leadership in healthcare. It emphasizes the need for leaders to continuously evaluate and improve their practices to provide the best possible care for patients with chronic diseases.
Impact of chronic diseases
Chronic diseases refer to health conditions that persist or progress over a long period, such as heart disease, diabetes, and cancer. These conditions not only impact the physical health of individuals but also have significant effects on their psychological, social, and economic well-being. This burden can result in lower quality of life outcomes for individuals, affecting their overall satisfaction, productivity, and ability to engage in daily activities.
Effective chronic disease management is essential in mitigating this burden, and a strong leadership perspective is crucial in promoting positive health outcomes for individuals living with chronic diseases. Figure 2 shows the computation of Impact of chronic diseases.
It can include implementing evidence-based interventions, promoting self-management skills, and creating supportive environments that address the holistic needs of individuals. By addressing the impact of chronic diseases from a leadership perspective, we can improve the quality of life of individuals living with chronic diseases and effectively manage the burden they face.
|
Table 2. Comparison of Impact of chronic diseases |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
RCM |
CCM |
HMSM |
DHSM |
Proposed Model |
|
|
21 |
7,23 |
12,81 |
15,36 |
20,19 |
26,78 |
|
23 |
9,76 |
14,29 |
17,47 |
22,68 |
27,36 |
|
25 |
8,89 |
11,93 |
18,19 |
23,47 |
26,29 |
|
27 |
11,34 |
13,47 |
16,92 |
21,61 |
27,47 |
|
29 |
10,19 |
15,26 |
19,78 |
22,83 |
26,14 |
+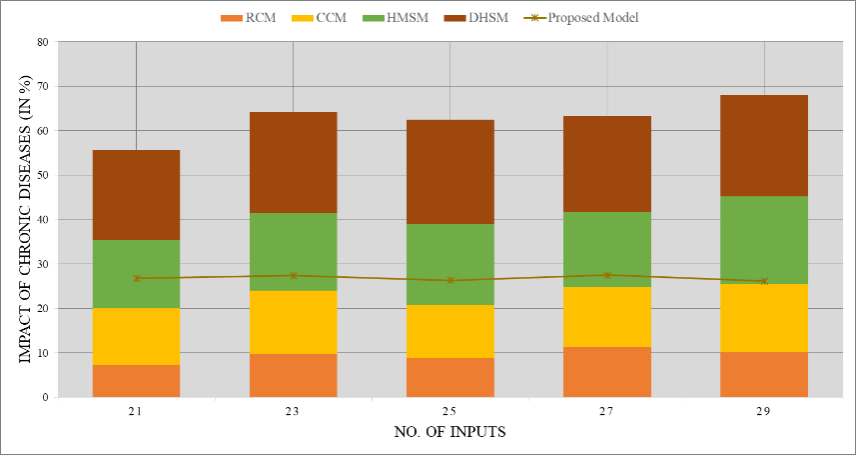
Figure 2. Computation of Impact of chronic diseases
Importance of decision-making
Decision-making is a crucial aspect of daily life that affects individuals, organizations, and society as a whole. It involves identifying and evaluating available options, considering potential consequences, and selecting the best course of action. This process becomes even more critical in the context of chronic disease management, where effective decision-making can lead to better quality-of-life outcomes for patients.
|
Table 3. Comparison of Importance of decision-making |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
RCM |
CCM |
HMSM |
DHSM |
Proposed Model |
|
|
41 |
6,36 |
11,19 |
14,42 |
19,68 |
56,93 |
|
42 |
7,74 |
13,47 |
18,19 |
22,84 |
57,56 |
|
43 |
12,28 |
10,36 |
16,64 |
21,31 |
56,12 |
|
44 |
9,62 |
12,14 |
19,37 |
22,49 |
67,29 |
|
45 |
8,91 |
15,74 |
17,83 |
24,29 |
46,74 |
A leadership perspective is essential in this process, as it involves balancing various factors such as medical expertise, patient preferences, and resource allocation. Figure 3 shows the computation of Importance of decision-making.
Adopting a patient-centered approach in decision-making can result in improved outcomes, including enhanced physical and mental health, increased satisfaction, and reduced healthcare costs. Ultimately, focusing on making informed and inclusive decisions can positively impact the quality of life for those living with chronic diseases.
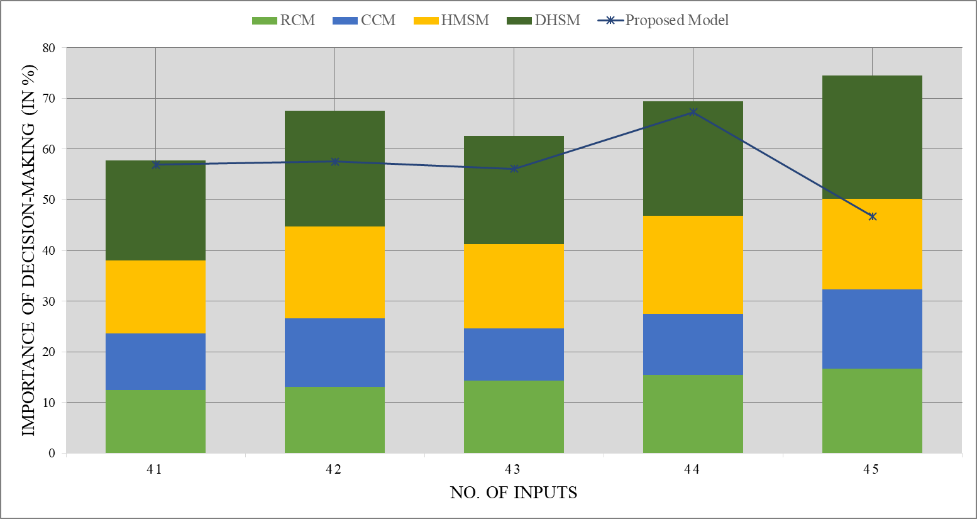
Figure 3. Computation of Importance of decision-making
Evidence-Based Interventions
Evidence-based interventions are scientifically proven strategies used to improve patient outcomes in chronic disease management. These interventions are based on the most up-to-date research and clinical evidence. They include various methods such as medication management, behavior change interventions, patient education, and self-management support.
|
Table 4. Comparison of Evidence-Based Interventions |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
RCM |
CCM |
HMSM |
DHSM |
Proposed Model |
|
|
30 |
10,74 |
13,29 |
17,17 |
22,58 |
46,34 |
|
60 |
7,15 |
14,41 |
16,36 |
21,21 |
67,82 |
|
90 |
11,23 |
15,87 |
18,36 |
23,78 |
56,94 |
|
120 |
9,16 |
12,47 |
19,34 |
24,89 |
77,12 |
|
150 |
8,63 |
11,12 |
14,74 |
21,34 |
56,19 |
These interventions aim to enhance the quality of life of patients by helping them manage their chronic conditions effectively and prevent complications. Figure 4 shows the computation of Evidence-Based Interventions.
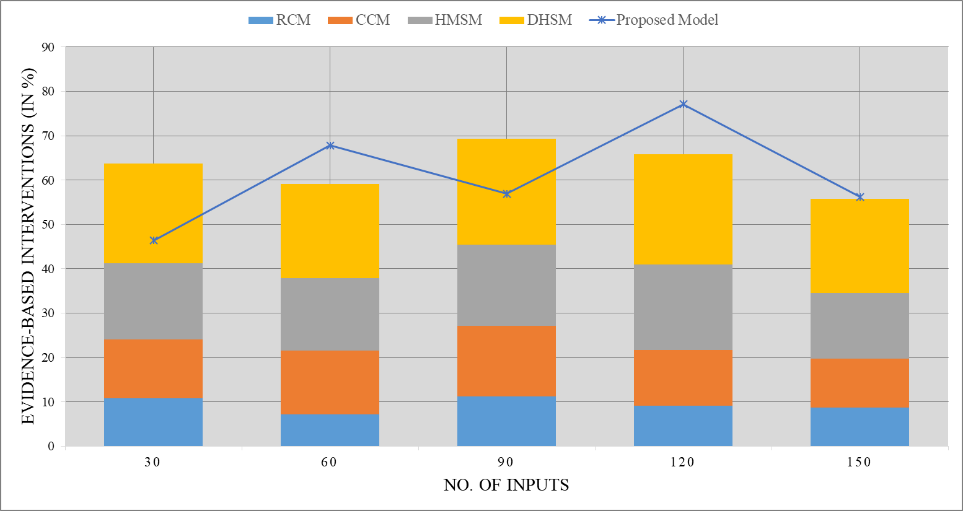
Figure 4. Computation of Evidence-Based Interventions
A leadership perspective is crucial in implementing these interventions as it involves strategic planning, training and support of healthcare professionals, and continuous evaluation and improvement of interventions. It ensures that the interventions are aligned with the needs of patients and are delivered sustainably and efficiently.
CONCLUSION
Chronic disease management is a complex and continuous process that requires effective leadership to improve patient outcomes and quality of life. Leadership plays a crucial role in promoting patient-centered care, care coordination, and interdisciplinary collaboration. This review aims to highlight the impact of effective leadership on the quality of life outcomes of patients with chronic diseases. Studies have shown that strong and effective leadership in chronic disease management leads to improved patient satisfaction, medication adherence, and health outcomes, such as reduced hospitalizations and complications. Leadership also facilitates the implementation of evidence-based practices and encourages a culture of continuous improvement. Effective leadership in chronic disease management involves setting clear goals, promoting team-based care, and ensuring open communication. It also requires a strong understanding of the unique needs of patients with chronic diseases and the ability to address social determinants of health. Leadership plays a critical role in improving quality of life outcomes in chronic disease management. Healthcare organizations should invest in developing strong leadership skills among their healthcare providers to enhance the overall care and well-being of patients with chronic diseases.
REFERENCES
1. Tran BX, Nguyen HT, Le HT, Latkin CA, Pham HQ, Vu LG, et al. Impact of COVID-19 on economic well-being and quality of life of the Vietnamese during the national social distancing. Frontiers in Psychology. 2020;11:565153.
2. Gorodeski EZ, Goyal P, Hummel SL, Krishnaswami A, Goodlin SJ, Hart LL, et al.; Geriatric Cardiology Section Leadership Council, American College of Cardiology. Domain management approach to heart failure in the geriatric patient: present and future. Journal of the American College of Cardiology. 2018;71(17):1921–36.
3. Neuhouser ML. The importance of healthy dietary patterns in chronic disease prevention. Nutrition Research. 2019;70:3–6.
4. Kilbourne AM, Beck K, Spaeth‐Rublee B, Ramanuj P, O’Brien RW, Tomoyasu N, et al. Measuring and improving the quality of mental health care: a global perspective. World Psychiatry. 2018;17(1):30–8.
5. Mekhail N, Levy RM, Deer TR, Kapural L, Li S, Amirdelfan K, et al.; Evoke Study Group. Durability of clinical and quality-of-life outcomes of closed-loop spinal cord stimulation for chronic back and leg pain: a secondary analysis of the Evoke randomized clinical trial. JAMA Neurology. 2022;79(3):251–60.
6. Poot CC, Meijer E, Kruis AL, Smidt N, Chavannes NH, Honkoop PJ. Integrated disease management interventions for patients with chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews. 2021;(9).
7. Ysrraelit MC, Fiol MP, Gaitán MI, Correale J. Quality of life assessment in multiple sclerosis: different perception between patients and neurologists. Frontiers in Neurology. 2018;8:729.
8. Yu CP, Cole ST, Chancellor C. Resident support for tourism development in rural Midwestern (USA) communities: perceived tourism impacts and community quality of life perspective. Sustainability. 2018;10(3):802.
9. Arsenault-Lapierre G, Henein M, Gaid D, Le Berre M, Gore G, Vedel I. Hospital-at-home interventions vs in-hospital stay for patients with chronic disease who present to the emergency department: a systematic review and meta-analysis. JAMA Network Open. 2021;4(6):e2111568.
10. Javaid ZK, Ali AA. Mediating role of mindfulness between quality of life and workplace stress among working women. Journal of Workplace Behavior. 2023;4(1).
FUNDING
The authors did not receive funding for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Shardha Purohit, Dhruvin Chauhan, Jitendriya Biswal, Simranjeet Nanda, Bharat Bhushan, Bhupal Pujari.
Research: Shardha Purohit, Dhruvin Chauhan, Jitendriya Biswal, Simranjeet Nanda, Bharat Bhushan, Bhupal Pujari.
Methodology: Shardha Purohit, Dhruvin Chauhan, Jitendriya Biswal, Simranjeet Nanda, Bharat Bhushan, Bhupal Pujari.
Writing - original draft: Shardha Purohit, Dhruvin Chauhan, Jitendriya Biswal, Simranjeet Nanda, Bharat Bhushan, Bhupal Pujari.
Writing - proofreading and editing: Shardha Purohit, Dhruvin Chauhan, Jitendriya Biswal, Simranjeet Nanda, Bharat Bhushan, Bhupal Pujari.