doi: 10.56294/hl2022173
ORIGINAL
Investigation of Scenario-Based Simulation for Communication Skills Development in Healthcare Education
Investigación de la simulación basada en escenarios para el desarrollo de habilidades de comunicación en la educación sanitaria
Shivangi Bansal1
![]() , Suraj Rajesh Karpe2
, Suraj Rajesh Karpe2
![]() , Swarup Kumar Bisoi3
, Swarup Kumar Bisoi3
![]()
1Noida International University, School of Engineering & Technology. Greater Noida, India.
2CSMSS Chh Shahu College of Engineering, Department of Electrical Engineering. Chh Sambhaji Nagar, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Paediatrics. Bhubaneswar, India.
Cite as: Bansal S, Rajesh Karpe S, Bisoi SK. Investigation of Scenario-Based Simulation for Communication Skills Development in Healthcare Education. Health Leadership and Quality of Life. 2022; 1:173. https://doi.org/10.56294/hl2022173
Submitted: 30-07-2022 Revised: 08-10-2022 Accepted: 12-12-2022 Published: 13-12-2022
Editor:
PhD. Prof. Neela Satheesh ![]()
ABSTRACT
In healthcare settings, effective communication is essential; it affects team relationships and patient outcomes. Scenario-based simulation has become a viable approach to enhancing communication skills in healthcare education. Research examines how scenario-based simulation can improve healthcare students’ communication skills. 250 participants were gathered and split into two groups: the Experimental Group (EG) (n=140), which consisted of healthcare students who participated in scenario-based simulations to enhance their communication skills, such as patient interaction and empathy, while a Control Group (CG) (n=110) received traditional classroom-based training, which focused on communication skills, without participating in the simulations. The goal of both groups was to enhance clinical communication abilities. Research used a mixed-methods technique to collect both quantitative and qualitative data. The IBM SPSS software version of 29.0 was utilized. Three statistical methods were used to analyse using Regression Analysis (RA) to ascertain the effect of the intervention on communication outcomes, ANOVA to compare the improvement between the EG and CG, and Paired t-tests to evaluate communication scores pre- and post-intervention. In comparison to the control group (CG), the experimental group (EG) exhibited significant improvements in communication skills, including empathy, clarity, and cultural sensitivity. The findings show that scenario-based simulation is a useful technique for improving clinical cooperation, communication skills, patient rapport, and confidence in managing interpersonal difficulties. Adding scenario-based simulations to healthcare education programs can result in more capable and sympathetic medical workers. This suggests that more investigation be done into the optimization and long-term impacts of simulation-based training.
Keywords: Healthcare Education; ANOVA; Regression Analysis; Paired T-Test; Scenario-Based Simulations; Traditional Classroom-Based Training.
RESUMEN
En los entornos sanitarios, la comunicación eficaz es esencial, ya que afecta a las relaciones del equipo y a los resultados de los pacientes. La simulación basada en escenarios se ha convertido en un enfoque viable para mejorar las habilidades comunicativas en la educación sanitaria. La investigación examina cómo la simulación basada en escenarios puede mejorar las habilidades comunicativas de los estudiantes sanitarios. Se reunieron 250 participantes y se dividieron en dos grupos: el grupo experimental (EG) (n=140), formado por estudiantes de asistencia sanitaria que participaron en simulaciones basadas en escenarios para mejorar sus habilidades comunicativas, como la interacción con el paciente y la empatía, mientras que un grupo de control (CG) (n=110) recibió formación tradicional en el aula, centrada en las habilidades comunicativas, sin participar en las simulaciones. El objetivo de ambos grupos era mejorar las habilidades de comunicación clínica. La investigación utilizó una técnica de métodos mixtos para recopilar datos cuantitativos y cualitativos. Se utilizó el programa informático IBM SPSS versión 29.0. Se utilizaron tres métodos estadísticos para el análisis: el análisis de regresión (AR) para determinar el efecto de la intervención en los resultados de comunicación, el ANOVA para comparar la mejora entre el GE y el GC, y las pruebas t pareadas para evaluar las puntuaciones de comunicación antes y después de la intervención. En comparación con el grupo de control (GC), el grupo experimental (GE) mostró mejoras significativas en las habilidades de comunicación, incluida la empatía, la claridad y la sensibilidad cultural. Los resultados muestran que la simulación basada en escenarios es una técnica útil para mejorar la cooperación clínica, las habilidades de comunicación, la relación con el paciente y la confianza en el manejo de las dificultades interpersonales. Añadir simulaciones basadas en escenarios a los programas de formación sanitaria puede dar lugar a trabajadores médicos más capaces y comprensivos. Esto sugiere que se investigue más sobre la optimización y las repercusiones a largo plazo de la formación basada en simulaciones.
Palabras clave: Educación Sanitaria; ANOVA; Análisis de Regresión; Prueba T Pareada; Simulaciones Basadas en Escenarios; Formación Tradicional en el Aula.
INTRODUCTION
Effective communication is essential to nursing education and is required to ensure patient safety. Patients and nurses have voiced frustration and anxiety when there is a lack of communication. Effective communication is essential for nurses. Nurses must recognize and communicate their patients’ problems as well as make sure they have access to all the information they require on their health.(1) Research indicates that by addressing symptoms and lowering psychological distress and anxiety, good communication enhances patient outcomes. Nonetheless, data indicates that nurses either lack communication skills as a result of insufficient training or undervalue the significance of person-centered communication. To completely grasp the required skills, learning communication techniques on the job is insufficient. Nurse competencies that are critical to patient care include interpersonal and communication skills.(2) Nursing competencies can be taught and evaluated with the help of simulation pedagogies. The goal of simulation is to replicate reality. Prewritten clinical scenarios according to the learner’s experience level are used to complete simulations. One of the core tenets of simulation is that realistic environments improve learning. One element of the simulation typology is the Standardized Patient (SP) technique. Through Objective Structured Clinical Examinations (OSCE), SPs evaluate competency. The OSCE is a clinical competency test that emphasizes results through observable actions. Furthermore, a key tactic for getting students interested in learning is structured guided debriefing, which is crucial for simulation training.(3)
After formative evaluation, debriefing is especially crucial because there is yet time to enhance performance before summative evaluation. For patients, caregivers, and medical personnel, hospital discharge is a complicated process. Communication was seen as a key element that either facilitated or hindered the discharge planning process. A key element of efficient discharge planning and continuity of care is communication between patients and medical staff on post-discharge needs.(4) Nurses, patients, and families’ impressions of patients’ discharge needs could not align for several reasons, including poor communication and a failure to include patients and families in the discharge planning process. Effective discharge planning has long been understood to depend on communication, which also shows a correlation between patients’ satisfaction with discharge planning and their general level of satisfaction.(5) While there are many researches on communication training for experienced nurses, there aren’t many on communication training for nurses just starting their careers. Some analyses are out of date, and others have poor design. Overall, few effects on patient outcomes, nurse behaviors, or nursing abilities were discovered.(6) Furthermore, evaluating oral communication skills using written tests could be challenging. As a result, OSCE has surpassed conventional written exams as the technique of choice for evaluating interpersonal and communication abilities. Simulations of patient care have been utilized in several research to improve students’ self-efficacy, learning satisfaction, and confidence. One key indicator of the effectiveness of training to enhance communication skills in the medical field is self-efficacy.(7)
To assess whether well scenario-based simulation improves the communication abilities of healthcare students, specifically in areas like patient engagement, empathy, clarity, and cultural sensitivity was the aim of this research. Research also aims to comprehend that clinical communication skills are developed in real-world healthcare contexts through immersive, experiential learning activities.
Research was conducted in the following order: Section 2 presents the related work, Section 3 outlines the methods, Section 4 presents the results, Section 5 illustrates the discussions, and Section 6 illustrates the conclusion.
Related Work
First-year nursing students’ development of patient safety behavior was impacted by Scenario-Based Learning (SBL) as opposed to the conventional demonstration method, which was investigated.(8) According to its findings, incorporating SBL into nursing skills training could be a useful teaching strategy for fostering the growth of patient safety abilities.
The performance and perceptions of fourth-level nursing students at the Faculty of Nursing regarding scenario-based learning were investigated in this analysis.(9) The results of the research offer credibility to the claim that SBL is a simple, dynamic, and successful teaching strategy. It improved nursing students’ capacity to learn and close the theory-practice gap.
Medical students’ observations of fully online education that featured COVID-19-pandemic-simulated clinical scenarios were evaluated in this investigation.(10) A significant percentage of apprentices encountered issues accessing this virtual reality platform online during this period.
The purpose of research was to examine and assess that computer-based scenarios affected the decision-making abilities of nursing undergraduates.(11) Compared to the CG, the research group’s decision-making scores were noticeably higher. Research group also stated that strongly felt that employing computer-based case scenarios enhanced both their general learning and specific nursing skills.
The purpose of research was to confirm the efficacy of a simulation-based learning program for nursing students responding in terms of teamwork, program satisfaction, response attitude, and triage accuracy.(12) Thirty-four university-bound nursing students who were about to graduate participated. Nursing students’ positive attitudes were effectively increased by the simulation-based program.
To improve second-year medical students’ error prevention, prospective error identification, and proactive communication abilities, research set out to create and apply digital patient safety case scenarios.(13) Enhancing students’ capacity to handle patient safety issues in actual healthcare environments was the ultimate objective. This research’s findings showed that in early Undergraduate Medical Education (UME), digital case analysis offered a creative way to convey important patient safety concepts and hands-on inter-professional communication practice.
Research examined how simulation training and problem-based scenarios affected nursing students’ propensity to report medication errors after graduation.(14) 93 nursing students who were about to graduate in their final semester were enlisted. Compared to problem-based scenarios, training through simulation showed more notable benefits. To increase medication safety, hospitals and nursing schools should use case-based scenarios or simulation training.
Research was conducted in a nursing course to determine how simulation exercises affected clinical practice satisfaction, clinical stress, and nursing students’ self-confidence.(15) The results of this research showed that simulation training interventions lower students’ stress levels and clinical satisfaction while not affecting their self-confidence. To help students in Obstetrics and Gynecology (OB-GYN) courses become more ready for clinical practice, nursing educators could offer scenario-based simulation training.
The use of Augmented Reality (AR) in medical education and training, as well as its impact on students’ experiences and learning results, were examined in Research.(16) This covers AR-based learning’s primary objectives, which include making complicated knowledge easier to understand and simplifying its delivery. Additionally, by enhancing medical students’ knowledge and comprehension, practical abilities, and social skills, AR can improve their educational experience.
METHOD
Research examines how scenario-based simulation affects healthcare students’ communication skills. Two groups of 250 nursing students were formed: the Experimental Group (EG) engaged in scenario-based simulations, while the Control Group (CG) was instructed in a conventional classroom setting. To evaluate gains in communication skills, factors such as nursing specialization, clinical experience, and demographic information were taken into account. Surveys and exams were used for pre-and post-intervention studies to assess that well scenario-based simulations improved communication skills. Figure 1 represents the overall research flow.
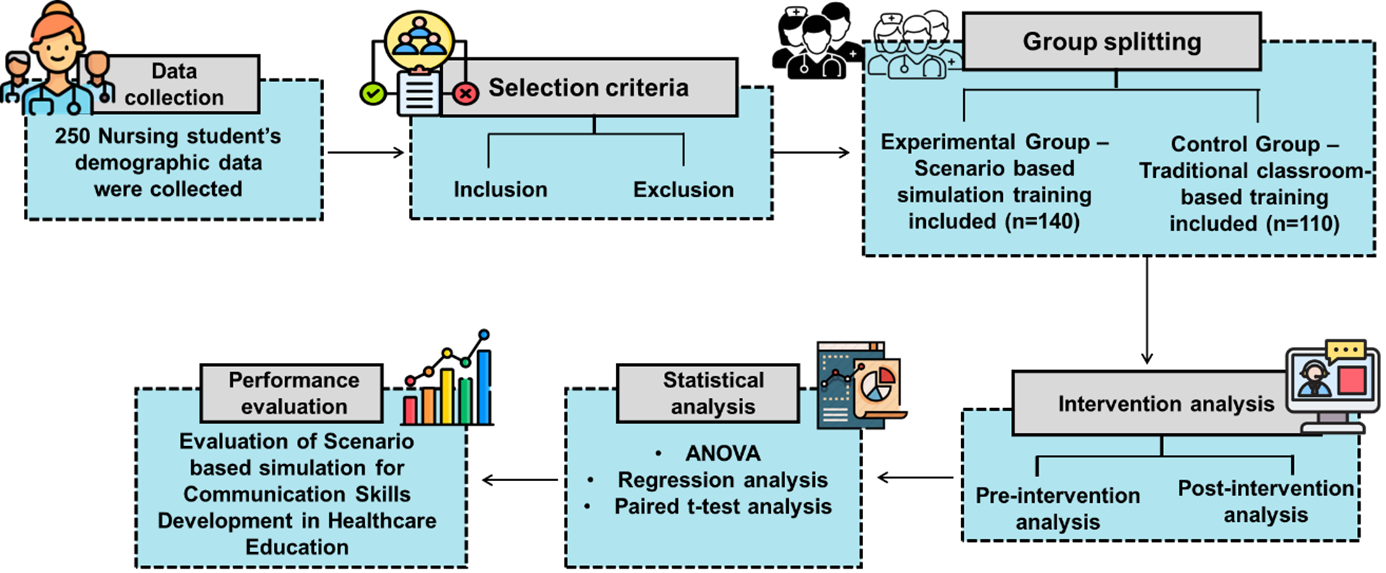
Figure 1. Research flow
Data collection
The demographics and characteristics of the individuals in the EG and CG are shown in table 1, with particular attention paid to gender, age, educational attainment, clinical experience, and nursing specialty. To assess that previous exposure to actual healthcare, environments affect the efficacy of scenario-based simulation in improving communication skills, clinical experience is incorporated. Because different nursing specialties call for varied interpersonal and empathetic approaches, the field of nursing specialization is taken into consideration to determine whether advances in communication skills vary depending on the participants’ important area.
|
Table 1. Demographic data |
|||
|
Variables |
Control Group (n=110) |
Experimental Group (n=140) |
Total (n=250) (%) |
|
Gender |
|||
|
Male |
35 (32 %) |
45 (32 %) |
80 (32 %) |
|
Female |
75 (68 %) |
95 (68 %) |
170 (68 %) |
|
Age |
|||
|
20-22 |
50 (45 %) |
65 (46 %) |
115 (46 %) |
|
23-25 |
45 (41 %) |
60 (43 %) |
105 (42 %) |
|
26-30 |
15 (14 %) |
15 (11 %) |
30 (12 %) |
|
Educational level |
|||
|
Undergraduate |
60 (55 %) |
85 (61 %) |
145 (58 %) |
|
Postgraduate |
50 (45 %) |
55 (39 %) |
105 (42 %) |
|
Clinical experience |
|||
|
None |
45 (41 %) |
40 (29 %) |
85 (34 %) |
|
>1 year |
50 (46 %) |
70 (50 %) |
120 (48 %) |
|
1-2 year |
15 (13 %) |
30 (21 %) |
45 (18 %) |
|
Field of Nursing specialization |
|||
|
Pediatric |
40 (36 %) |
45 (32 %) |
85 (34 %) |
|
Surgical |
35 (32 %) |
50 (36 %) |
85 (34 %) |
|
Community Health |
25 (23 %) |
30 (21 %) |
55 (22 %) |
|
Mental health nursing |
10 (9 %) |
15 (11 %) |
25 (10 %) |
|
Initial communication level |
|||
|
Low |
40 (36 %) |
45 (32 %) |
85 (34 %) |
|
Moderate |
50 (46 %) |
65 (46 %) |
115 (46 %) |
|
High |
20 (18 %) |
30 (21 %) |
50 (20 %) |
Selection criteria
Participants were designated based on precise criteria to guarantee the analysis’s validity and applicability.
Inclusion criteria
· Nursing Students: to guarantee a pertinent participant experience, only nursing students participating in undergraduate or graduate programs were included.
· Clinical Experience: individuals who had been exposed to clinical environments for at least six months were thought to have a foundational comprehension of them.
· Age Range: to standardize learning and developmental capacities, only individuals between the ages of 20 and 30 were chosen.
· Willingness to Participate: to take part in the scenario-based simulation and the research’s pre/post assessments, participants had to voluntarily assent.
Exclusion criteria
· Non-Nursing Students: to concentrate on communication skills unique to nursing, students from other healthcare fields were not allowed to participate.
· Severe Health Conditions: participants were not allowed to participate in simulations if they had serious chronic conditions that would interfere with their capacity to ensure.
· Clinical Experience: to guarantee sufficient baseline knowledge and comprehension of healthcare environments, participants with less than six months of clinical experience were disqualified.
Group splitting
250 participants were split into two groups at random: Researchers divided 250 participants into 2 distinct groups: 110 students in the CG received standard classroom studies and 140 participants in the EG practiced clinical communications through scenario-based simulations. The research used this group splitting to examine if simulation methods worked better than regular instruction.
Experimental Group (EG)
This group consisted of 140 healthcare students who took part in scenario-based simulations specifically designed to help them develop better clinical communication skills in both patient relations and empathy. Students developed communication expertise through simulator use, which let them work in real-life patient scenarios. The analysis trained students to feel confident in their abilities while growing better in interpersonal and patient empathy. The main goal of research program focused on teaching students through immersed training with instant feedback. Research needed to develop their core communication skills during actual clinical work.
Control Group (CG)
A total of 110 healthcare students learned communication abilities through regular classroom sessions, which did not include scenario-based simulations. The program used lectures and seminars plus role-play scenarios to teach communication concepts and theory to students. The CG learned patient communication basics but students in EG gained practical experience through simulations. It did not get comparable hands-on training opportunities in medical facilities. Trained staff wished to boost students’ knowledge of theoretical communication lessons.
Intervention analysis
The main purpose of this investigation was to measure that well immersive simulations teach better communication techniques. The EG conducted simulation exercises to develop improved methods for patients to engage while fostering greater empathy in healthcare interactions. This research considered that students had mastered clinical communication skills in real medical scenarios.
Pre-intervention analysis
Pre-intervention analysis measured how well healthcare students from both groups communicated at the start. The baseline measurements included surveys and tests to track key aspects including patient contact quality and both emotional and verbal communication skills. This research set up a solid method to understand scenario-based simulation impacts on outcomes. The team aimed to determine each group’s strengths and areas for improvement in communication skills prior to the training. Training results for these two groups were evaluated by referencing their pre-training performance data.
Post-intervention analysis
This research’s goal was to measure the impact scenario-based simulations had on the EG’s communication skills versus those of the CG. The groups completed evaluation tests after training on communication clarity, empathy, and patient interactions. With notable gains in their ability to manage cultural differences and communicate effectively with patients, the EG performed better in a variety of skill areas. After the intervention, results show that hands-on immersive learning produces superior communication outcomes.
Statistical analysis
Research uses IBM SPSS version 29.0 to show that scenario-based simulations boost healthcare student communication competency. It analyses the use of Paired t-tests to assess the way that EG and CG participants developed their communication skills during the intervention period. It will use ANOVA to compare communication skill progress between the groups to show if scenario training provides significant benefits over standard classroom education. Research uses Regression Analysis to find relations between communication skills and participant characteristics such as age, educational levels and clinical experience. It can be observed from these statistical models that medical students’ communication abilities improve with carefully planned scenario training.
RESULTS
This research evaluated the extent to which scenario-based simulation enhances healthcare students’ communication skills, particularly in areas such as patient engagement, empathy, clarity, and cultural sensitivity. The research aims to compare the communication benefits between an EG that engaged in scenario-based simulations and a CG that received traditional classroom-based instruction.
Comparing groups using ANOVA analyses based on Scenario-Based Simulation to improve communication skills
Research uses ANOVA testing to compare that communication skills changed between participants after receiving experimental treatment. By comparing simulation to regular practice, the analysis shows if scenario-based learning helped the EG obtain better patient interaction and communication results. It conducts the ANOVA test to determine if the improvements in multiple communication areas are substantive and differ between groups. Table 2 and figure 2 show that the EG’s communication skills in empathy, clarity, cultural sensitivity and patient contact developed distinctly. Statistics demonstrate significant improvement at a 0,001 percent confidence level for all factors. The EG made substantial progress with its communication skills compared to the CG. Research outcome demonstrates that scenario-based simulation builds stronger teamwork and better communication abilities while helping nurses’ bond better with patients and feel more resolved to handle patient-related challenges.
|
Table 2. Outcomes of the ANOVA test |
|||||||
|
Communication skills |
df |
Sum of squares |
F-value |
p-value |
Effect Size (η²) |
Significant
|
|
|
Between groups |
Within groups |
||||||
|
Empathy |
1 |
248 |
105,50 |
23,75 |
<0,001 |
0,087 |
Significant |
|
Clarity |
1 |
248 |
98,75 |
21,45 |
<0,001 |
0,079 |
Significant |
|
Cultural sensitivity |
1 |
248 |
112,30 |
24,50 |
<0,001 |
0,090 |
Significant |
|
Patient interaction |
1 |
248 |
120,40 |
26,00 |
<0,001 |
0,095 |
Significant |
|
Overall communication improvement |
1 |
248 |
135,60 |
28,20 |
<0,001 |
0,102 |
Significant |
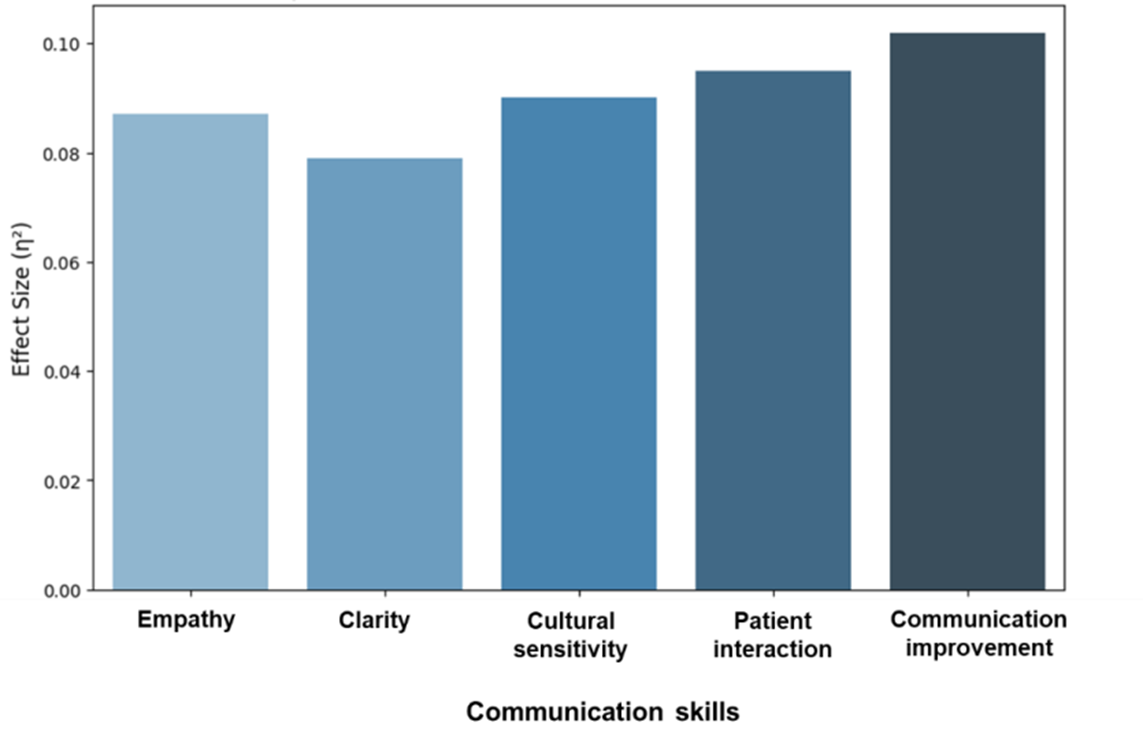
Figure 2. Effect Size (η²) of communication skills in post-intervention
Regression Analysis of Scenario-Based Simulation for Enhancements in Communication Skills
Research used Regression Analysis to show that scenario-based simulation sessions helped students improve their communication skills. Research aimed to contrast EG and CG results while evaluating exercise effects on communication performance. The outcomes of the scenario-based simulation intervention on healthcare students’ enhanced communication abilities are shown in table 3 and figure 3. The intervention raised scenario-based simulation use that explained 70 % of the communication skill improvement within the EG. Performance evaluation for every communication skill dimension revealed improvements including empathy (β=0,65, p<0,001), clarity (β=0,68, p<0,001), cultural sensitivity (β=0,62, p<0,001), and patient interaction (β=0,64, p<0,001) through the EG. Total communication performance improved by 70 % as measured on all tests (β = 0,70, p < 00,001). The sample receiving training displayed better results for communication than the CG. The findings demonstrate that scenario-based simulation methods effectively improve healthcare team communication and relationship skills along with patient engagement and personal confidence during interpersonal challenges.
|
Table 3. Analysis of Regression outcomes |
||||||
|
Communication skills |
Group |
B |
β |
t-value |
p-value |
R2 |
|
Empathy |
Experimental |
3,80 |
0,65 |
12,50 |
<0,001
|
0,42 |
|
Control |
2,50 |
0,45 |
8,30 |
0,28 |
||
|
Clarity |
Experimental |
3,90 |
0,68 |
13,20 |
<0,001 |
0,44 |
|
Control |
2,60 |
0,48 |
8,90 |
0,30 |
||
|
Cultural sensitivity |
Experimental |
3,50 |
0,62 |
11,80 |
<0,001 |
0,40 |
|
Control |
2,40 |
0,43 |
7,90 |
0,26 |
||
|
Patient interaction |
Experimental |
3,60 |
0,64 |
12,0 |
<0,001 |
0,41 |
|
Control |
2,30 |
0,42 |
7,60 |
0,25 |
||
|
Overall communication improvement |
Experimental |
4,10 |
0,70 |
14,0 |
<0,001 |
0,50 |
|
Control |
2,80 |
0,50 |
9,50 |
0,32 |
||
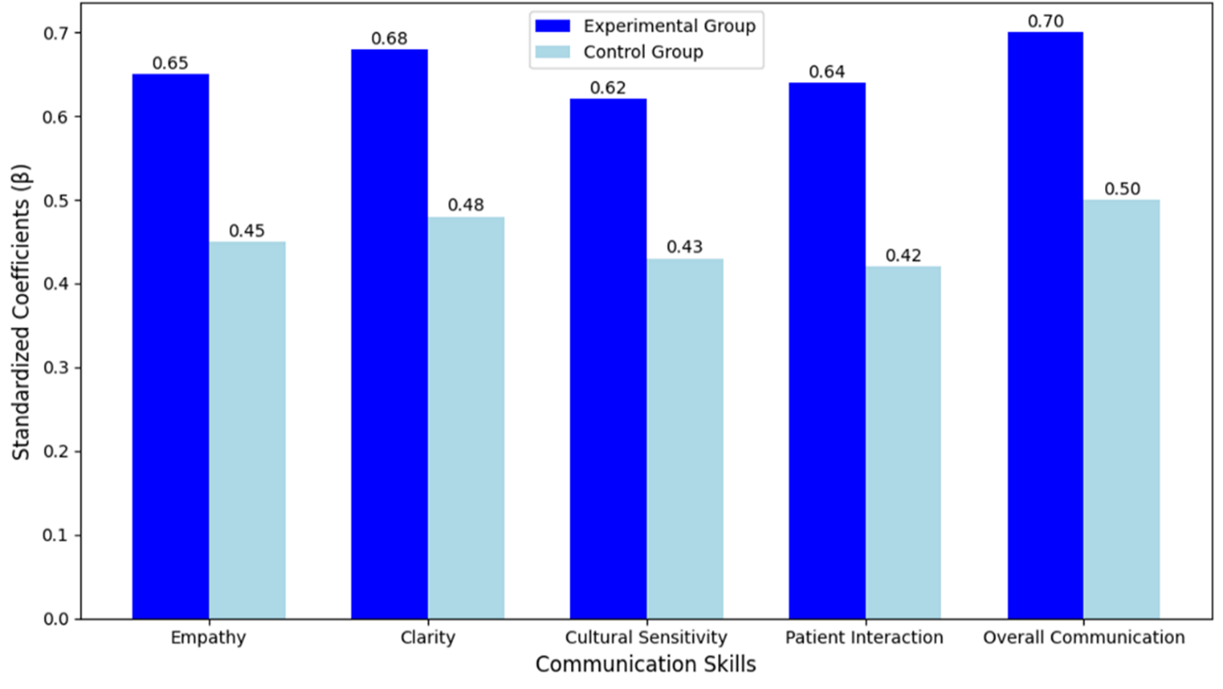
Figure 3. Communication skills outcomes
Analysis of the Improvement of Communication Skills in Healthcare Students using Paired t-Tests following Scenario-Based Simulation
This research uses a paired t-test to examine differences between communication score changes for both groups following this intervention. This research checks to see if EG members gained larger improvements in their communication skills during and after simulation training than CG participants. The main thing this research evaluates is the mean differences between ratings from before and after the intervention period. Table 4 and figure 4 show the statistical significance values. Research shows major improvements across all communication skills because the p-values registered under 0,001. Participants in the EG improved their empathy and clear communication skills plus cultural understanding compared to the comparison group results. Results show that scenario-based simulation helps students become better at patient interactions along with their communication skills and social confidence.
|
Table 4. Outcomes of Paired t-test |
||||||
|
Communication skills |
Group |
Mean of Pre-intervention |
Mean of post-intervention |
Mean difference |
t-value |
p-value |
|
Empathy |
Experimental |
6,80 ± 1,20 |
9,20 ± 1,10 |
2,40 ± 0,90 |
12,80 |
<0,001 |
|
Control |
6,70 ± 1,30 |
7,80 ± 1,20 |
1,10 ± 0,80 |
7,90 |
||
|
Clarity |
Experimental |
6,90 ± 1,10 |
9,50 ± 1,00 |
2,60 ± 0,90 |
13,20 |
<0,001 |
|
Control |
6,80 ± 1,20 |
8,10 ± 1,1 |
1,30 ± 0,80 |
8,40 |
||
|
Cultural sensitivity |
Experimental |
6,70 ± 1,30 |
9,00 ± 1,10 |
2,30 ± 0,90 |
12,40 |
<0,001 |
|
Control |
6,60 ± 1,20 |
7,70 ± 1,10 |
1,10 ± 0,80 |
7,80 |
||
|
Patient interaction |
Experimental |
6,80 ± 1,20 |
9,30 ± 1,00 |
2,50 ± 0,90 |
12,90 |
<0,001 |
|
Control |
6,70 ± 1,30 |
8,00 ± 1,10 |
1,30 ± 0,80 |
8,20 |
||
|
Overall communication improvement |
Experimental |
6,80 ± 1,10 |
9,50 ± 1,00 |
2,70 ± 0,80 |
13,40 |
<0,001 |
|
Control |
6,70 ± 1,20 |
8,10 ± 1,10 |
1,40 ± 0,80 |
8,50 |
||
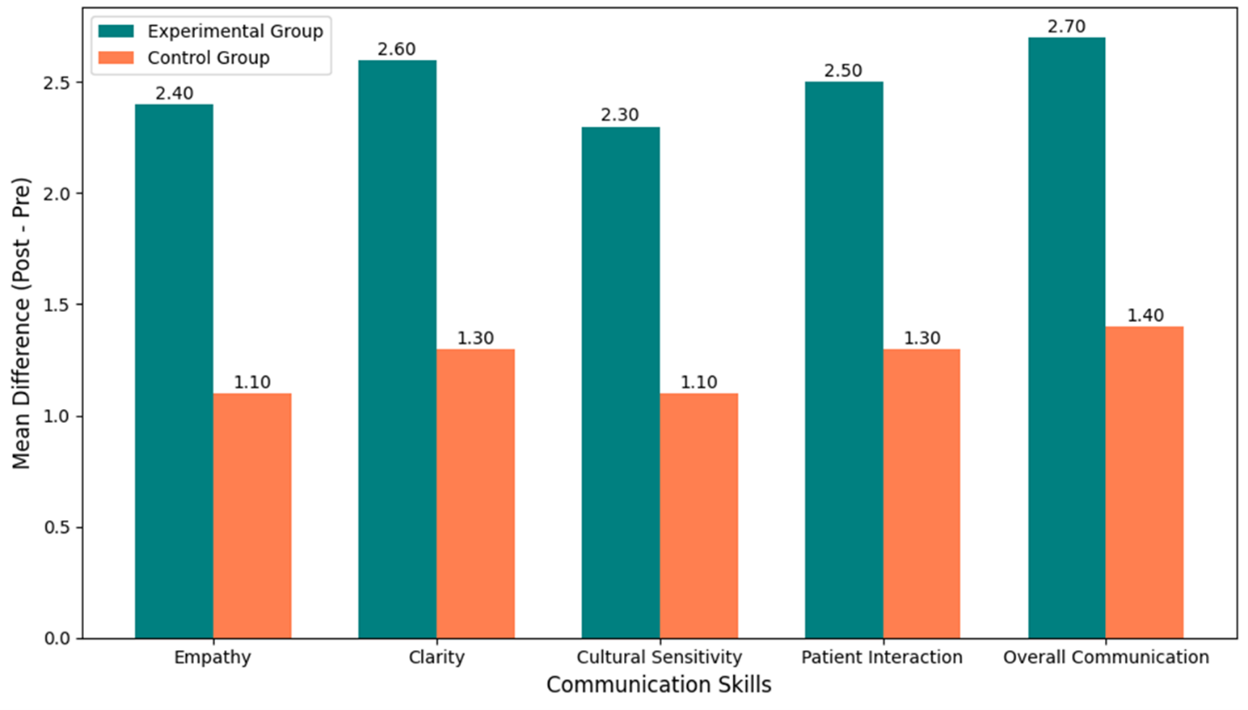
Figure 4. Paired t-test result for communication skills
DISCUSSION
Research analyzed healthcare student communication development from scenario-based simulation, specifically in empathy skills and cultural sensitivity. The EG achieved better results than the CG across all communication areas with test outcomes confirmed by statistical methods. The participants in the experimental group (EG) demonstrated improved communication skills during patient care and engaged in practicing empathy together. These results show that scenario-based simulations effectively increase clinical communication performance. This research demonstrates that useful immersive learning helps healthcare students develop better social skills. According to the research, scenario-based interventions promote both skill acquisition and long-term confidence in managing complex patient interactions, which emphasizes the value of incorporating experiential learning through healthcare education programs to train students for practical difficulties.
CONCLUSIONS
Scenario-based simulation changed healthcare students’ communication abilities, especially in terms of their effectiveness in expressing themselves while displaying empathy and cultural sensitivity were determined in this research. The results supported by ANOVA tests revealed EG participants achieved stronger communication outcomes than CG participants across all test domains. The analysis of variance results showed that all factors reached very high levels of statistical significance when their p-values fell below 0,001. showed that the EG improved its communication skills in all areas including empathy (0,65 enhancement with P<0,001) clarity (0,68 gain with P≤0,001), cultural sensitivity (0,62 gain with P≤0,001), and patient interaction (0,64 betterment with P<0,001). It shows that members. It shows that members of the EG developed better communication skills than the CG, achieving statistical significance at or below 0,001. Its findings show that scenario-based simulations effectively increase clinical communication performance. The results of this research couldn’t be as broadly applicable as could be due to its narrow emphasis on a particular geographic area and cohort of nursing students. Future research should examine a range of demographics and the long-term effects of scenario-based simulations on medical results. Inter professional education expansion could also improve cooperative communication and teamwork abilities.
BIBLIOGRAPHIC REFERENCES
1. Paranjape K, Schinkel M, Panday RN, Car J, Nanayakkara P. Introducing artificial intelligence training in medical education. JMIR medical education. 2019 Dec 3;5(2):e16048. https://doi.org/10.2196/16048
2. Bloomfield JG, Schneider CR, Lane S, Stehlik P, Frotjold A. Evaluating a large-scale introductory interprofessional education workshop for developing interprofessional socialization in medical, nursing and pharmacy students: A quasi-experimental pre-test post-test study. Nurse Education Today. 2021 Apr 1;99:104777. https://doi.org/10.1016/j.nedt.2021.104777
3. Ezhumalai G, Jayashree M, Nallasamy K, Bansal A, Bharti B. Referrals to a pediatric emergency department of a tertiary care teaching hospital before and after the introduction of a referral education module-a quality improvement study. BMC Health Services Research. 2020 Dec;20:1-7. https://doi.org/10.1186/s12913-020-05649-w
4. So HY, Chen PP, Wong GK, Chan TT. Simulation in medical education. Journalofthe Royal CollegeofPhysiciansof Edinburgh. 2019 Mar;49(1):52-7. https://doi.org/10.4997/jrcpe.2019.112
5. Roth CG, Eldin KW, Padmanabhan V, Friedman EM. Twelve tips for the introduction of emotional intelligence in medical education. Medical teacher. 2019 Jul 3;41(7):746-9. https://doi.org/10.1080/0142159X.2018.1481499
6. Mukhalalati BA, Taylor A. Adult learning theories in context: a quick guide for healthcare professional educators. Journal of medical education and curricular development. 2019 Apr;6:2382120519840332. https://doi.org/10.1177/2382120519840332
7. Watts PI, McDermott DS, Alinier G, Charnetski M, Ludlow J, Horsley E, Meakim C, Nawathe PA. Healthcare simulation standards of best practiceTM simulation design. Clinical Simulation in Nursing. 2021 Sep 1;58:14-21. https://doi.org/10.1016/j.ecns.2021.08.009
8. Yilmaz DU, Palandoken EA, Ceylan B, Akbiyik A. The effectiveness of scenario-based learning to develop patient safety behavior in first-year nursing students. International Journal of Nursing Education Scholarship. 2020 Jan 28;17(1):20200011. https://doi.org/10.1515/ijnes-2020-0011
9. Ahmed HH. Adopting scenario-based learning in critical care nursing education: students’ achievement and feedback. Am J Nurs. 2019 Jun;7(4):581-8. Doi:10.12691/ajnr-7-4-20.
10. De Ponti R, Marazzato J, Maresca AM, Rovera F, Carcano G, Ferrario MM. Pre-graduation medical training including virtual realityduring COVID-19 pandemic: a reportonstudents’ perception. BMC medical education. 2020 Dec;20:1-7. https://doi.org/10.1186/s12909-020-02245-8
11. La Cerra C, Dante A, Caponnetto V, Franconi I, Gaxhja E, Petrucci C, Alfes CM, Lancia L. Effects of high-fidelity simulation based on life-threatening clinical condition scenarios on learning outcomes of undergraduate and postgraduate nursing students: a systematic review and meta-analysis. BMJ open. 2019 Feb 1;9(2):e025306. https://doi.org/10.1136/bmjopen-2018-025306
12. Kim J, Lee O. Effects of a simulation-based education program for nursing students responding to mass casualty incidents: A pre-post intervention study. Nurse education today. 2020 Feb 1;85:104297. https://doi.org/10.1016/j.nedt.2019.104297
13. McCoy L, Lewis JH, Simon H, Sackett D, Dajani T, Morgan C, Hunt A. Learning to speak up for patient safety: interprofessional scenarios for training future healthcare professionals. Journal of medical education and curricular development. 2020 Jun;7:2382120520935469. https://doi.org/10.1177/2382120520935469
14. Kuo SY, Wu JC, Chen HW, Chen CJ, Hu SH. Comparison of the effects of simulation training and problem-based scenarios on the improvement of graduating nursing students to speak up about medication errors: A quasi-experimental study. Nurse Education Today. 2020 Apr 1;87:104359. https://doi.org/10.1016/j.nedt.2020.104359
15. Erenel AŞ, Sözbir ŞY, Aksoy MU, Gürcüoğlu EA, Aksu SP, Toprak FÜ, Asalioğlu CU. Effect of scenario-based simulation training on the obstetrics and gynecology nursing clinical practicum. Journal of Nursing Research. 2021 Apr 1;29(2):e142. DOI: 10.1097/jnr.0000000000000417
16. Dhar P, Rocks T, Samarasinghe RM, Stephenson G, Smith C. Augmented reality in medical education: students’ experiences and learning outcomes. Medical education online. 2021 Jan 1;26(1):1953953. https://doi.org/10.1080/10872981.2021.1953953
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Data curation: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Formal analysis: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Research: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Methodology: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Project management: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Resources: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Software: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Supervision: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Validation: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Display: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Drafting - original draft: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.
Writing - proofreading and editing: Shivangi Bansal, Suraj Rajesh Karpe, Swarup Kumar Bisoi.