doi: 10.56294/hl2022172
ORIGINAL
Global Best Practices in Healthcare Management: A Comparative Analysis
Buenas prácticas mundiales en gestión sanitaria: Un análisis comparativo
Satya Sundar Gajendra Mohapatra1
![]() , Nija Mani2
, Nija Mani2 ![]()
1Siksha ‘O’ Anusandhan (Deemed to be University), Department of Radiology, IMS and SUM Hospital. Bhubaneswar, India.
2Noida International University, School of Sciences. Greater Noida, India.
Cite as: Gajendra Mohapatra SS, Mani N. Global Best Practices in Healthcare Management: A Comparative Analysis. Health Leadership and Quality of Life. 2022; 1:172. https://doi.org/10.56294/hl2022172
Submitted: 29-07-2022 Revised: 07-10-2022 Accepted: 12-12-2022 Published: 13-12-2022
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: the whole of healthcare in a country is focused on the delivery of high-quality and efficient healthcare services, it will be essential to explore successful practices from abroad. Taking a comparative approach, this study finds several best practices across the globe in health system management, and identifying these core elements will help contribute to the success of healthcare systems.
Method: a literature review was performed to search for studies and reports on best practices in healthcare management from all over the world. We searched databases such as PubMed, Google Scholar, and WHO reports. The included studies were appraised for their relevance, credibility, and rigor. Through thematic and pattern identification and analysis, the findings were synthesized to produce the results.
Results: differences and similarities in healthcare management practices have been found, as evidenced by the results of the review. The key commonalities included the focus on patient-centered care, the importance of going beyond effective communication and leveraging technology to enhance the delivery of health services. Furthermore, the presence of an explicit healthcare policy and competent leadership were demonstrated to be critical elements of a successful health system in most countries.
Conclusions: implementing a student-approach-based clinical education. A strong and pragmatic policy, propelled by good leadership, is the formula for successful healthcare. Healthcare management practices vary across countries, pointing to the fact that there is no universal template or model for managing healthcare systems. This is an excellent benefit to healthcare professionals and planners because it will give them a broader outlook on effective practices in the world of healthcare delivery that can be adapted and implemented in the desired environment to enhance the efficient delivery of healthcare services.
Keywords: Leadership; Core Elements; Pattern Identification; Patient-Centered; Clinical Education.
RESUMEN
Introducción: el conjunto de la sanidad de un país se centra en la prestación de servicios sanitarios eficientes y de alta calidad, por lo que será esencial explorar prácticas de éxito procedentes del extranjero. Adoptando un enfoque comparativo, este estudio encuentra varias buenas prácticas en todo el mundo en materia de gestión de sistemas sanitarios, y la identificación de estos elementos básicos ayudará a contribuir al éxito de los sistemas sanitarios.
Método: se realizó una revisión bibliográfica para buscar estudios e informes sobre mejores prácticas en la gestión de la sanidad en todo el mundo. Se realizaron búsquedas en bases de datos como PubMed, Google Scholar e informes de la OMS. Se evaluó la pertinencia, la credibilidad y el rigor de los estudios incluidos. Los resultados se sintetizaron mediante la identificación y el análisis temático y de patrones.
Resultados: se han encontrado diferencias y similitudes en las prácticas de gestión sanitaria, tal y como evidencian los resultados de la revisión. Entre los principales puntos en común figuran la atención centrada en
el paciente, la importancia de ir más allá de una comunicación eficaz y el aprovechamiento de la tecnología para mejorar la prestación de servicios sanitarios. Además, la presencia de una política sanitaria explícita y un liderazgo competente demostraron ser elementos críticos de un sistema sanitario de éxito en la mayoría de los países.
Conclusiones: implantar una enseñanza clínica basada en el enfoque del estudiante. Una política sólida y pragmática, impulsada por un buen liderazgo, es la fórmula del éxito de la asistencia sanitaria. Las prácticas de gestión sanitaria varían de un país a otro, lo que indica que no existe una plantilla o modelo universal para gestionar los sistemas sanitarios. Los profesionales y planificadores de la sanidad se beneficiarán de este estudio, ya que les proporcionará una visión más amplia de las prácticas eficaces en el mundo de la prestación de servicios sanitarios que pueden adaptarse y aplicarse en el entorno deseado para mejorar la prestación eficiente de servicios sanitarios.
Palabras clave: Liderazgo; Elementos Básicos; Identificación de Patrones; Centrado en el Paciente; Educación Clínica.
INTRODUCTION
Healthcare management is a critical component of the healthcare system, focusing on the planning, organization, direction, and control of healthcare services and facilities. Healthcare management works towards improving the quality, accessibility and effectiveness of healthcare delivery and striking a balance between cost management and patient satisfaction.(1) In recent years there has been an increased focus on global best practices in health care management as the health care systems and the challenges they face have come to critical juncture. Hence this essay will explore the global best practices in regard to healthcare management in various nations.(2) One of the main global best practices in healthcare administration is technology. By using technology, healthcare systems have been able to improve patient care delivery and efficiency. Better data means better outcomes for patients and at least avoid unnecessary tests and procedures.(3) Another powerful component is the use of data and analytics. These tools allow healthcare managers to identify new trends and patterns of patients so they can deliver more targeted, efficient care solutions.(4) This has been done effectively in the UK, where National Health Service (NHS) data is used to track patients’ outcomes and better healthcare delivery. Data-driven analysis, for example, has been used to predict outbreaks and target resource allocation in countries such as South Korea and Taiwan. Promoting preventive care and managing diseases can be one of the best practices of healthcare management in the world.(5) But we have already seen successful preventative care programs, such as those existing in Japan or Switzerland or Australia which improved overall health outcomes and reduced healthcare costs. These include regular health screenings, promoting healthy living and detecting and treating chronic conditions early on.(6) Not only does this paradigm lead to better health outcomes, but it also eases the burden on healthcare systems. Primary care is the foundation of health care systems in many nations. It is critical to view a patient’s medical history from the big-picture viewpoint, and for patients to have a single entry point for coordinating their care and getting referred to other specialists as warranted — which happens in primary care.(7) Such countries included Canada, France, and Germany, which have robust primary care systems and that correlate with lower spending on healthcare and improved patient care outcomes. They also prioritize training and education of primary care providers, so they are ready to treat patients as holistically as possible. Likewise, patient engagement and empowerment have been widely acknowledged as crucial factors of global standards and best practices in the management of health care.(8) Most other countries, including Denmark, involve patients in decision-making and give them the information they need to make an informed choice about their care. Such an approach enhances not only patient satisfaction, but also patient involvement in his/her health and health outcomes. Last but not least, finance is one of the core pillars and is critical to healthcare management, with hospital budgets and spending soaring across the globe, alongside successful cost containment initiatives in Germany, Australia, and Japan.(9) And that includes stricter healthcare price controls and negotiations with big pharma to reduce drug prices. Such practices have been shown to improve healthcare outcomes, increase the efficiency with which the care is delivered, and better control costs. These best practices could be a way forward in the face of countries struggling in the health systems. These models of care provide lessons to continue shaping health care delivery for improved health outcomes.(10)
A research gap is the “the amount of knowledge with no equivalent systems, without information on structures for a similar health administration.
Most global health opportunities need data for resource-rich settings, however developing or under-resourced country are rarely included in studies and analysis of management practices. Inevitably this leads to greater attention to developed world & discounting very relevant perspectives & lessons from elsewhere.
Cultural context is an element commonly overlooked in comparative studies, however, is one of the main determinants for successful healthcare management strategies. This open question offers ample opportunity for future exploration and research regarding how diversity in cultural values, beliefs, and assumptions impact the success of different management strategies.
There is no long-term assessment of the global management of health care, which makes it difficult to assess the sustainability and effectiveness of global management over time.
While technology into healthcare management and usage is fast-emerging, there is limited research of technology in different countries.
METHOD
Wing, C.,et,al. During the last years, the methodology behind difference in difference studies has been discussed, for example in reference . In the design of difference in difference studies, a treatment group and some control group is identified, followed by a measurement of the outcome of interest before and after the treatment starts, and finally, a comparison of the change in outcomes between the two groups. Cohen, S. P.,et,al. Chronic pain: Chronic pain is defined as any ongoing pain that persists for longer than 3 months . It can be caused by diverse conditions, including arthritis, fibromyalgia and nerve damage. Lin, I. M.,et,al. and Best practice care for musculoskeletal pain includes comprehensive assessment and diagnosis, and the formulation of a therapeutic plan tailored to the individual which may include a combination of medication, physical therapy and lifestyle changes. Boulanger, J. M.,et,al. venouseThe Canadian Stroke Best Practice Recommendations for Acute Stroke Management are evidence-based guidelines that outline the best available practices for healthcare professionals in the management of acute stroke patients. Leoni, S.,et,al. Current guidelines for managing non-alcoholic fatty liver disease (NAFLD) recommend lifestyle modifications including weight loss, physical activity, and a healthy diet . Sebestyén, V.,et,al. Introduction What are Focal points for sustainable dev. strategies. Text mining-based comparative analysis of voluntary national reviews can unveil patterns and trends to help craft effectively targeted sustainable development policies. Khan, S.,et,al. Deep learning in SHM has been discussed in several papers . It reviews different uses of deep learning in SHM, including fault diagnosis, prognostics, and outlier detection. Kahwati, L. C.,et,al. Qualitative comparative analysis (QCA) Crosson et al. It consists of comparing cases or groups to see how different variables causate certain outcomes. Vogl, G. W.,et,al. describes the diagnostic and prognostic capabilities of Industrial Internet of Things (IIoT) components are critical to ensure manufacturers identify as well as mitigate against impending issues, preventing the huge costs of downtimes. Some best practices involve the use of advanced technology, data analytics, and continuous improvement processes to improve efficiency, quality, and cost-effectiveness. Kerzner, H.,et,al. , project management best practices project management best practices are set of concepts and processes, recommended by experts, for the management and execution of project.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Wing, C.,et,al. |
2018 |
“Designing difference in difference studies allows for a comparison of treatment effects over time, reducing the influence of external factors.” |
Difficulty in finding a proper control group or finding a suitable control group with similar characteristics as the treatment group. |
|
Cohen, S. P.,et,al. |
2021 |
It signals a problem in the body, potentially leading to early detection and treatment of an underlying condition. |
Difficulty in finding effective treatment and management strategies, leading to reduced quality of life and psychological distress. |
|
Lin, I. M.,et,al. |
2020 |
Best practice care for musculoskeletal pain prioritizes evidence-based treatment, leading to better outcomes and improved patient satisfaction. |
“Best practice care for musculoskeletal pain may not be accessible or affordable for all patients due to financial, geographical, or cultural barriers.” |
|
Boulanger, J. M.,et,al. |
2018 |
Comprehensive and evidence-based guidelines to support standardized and effective stroke treatment, leading to improved patient outcomes and quality of care. |
The recommendations may not account for individual patient preferences or comorbidities. |
|
Leoni, S.,et,al. |
2018 |
One advantage is improved diagnosis and treatment of non-alcoholic fatty liver disease, leading to better outcomes for patients. |
Individualized treatment recommendations based on disease severity and comorbidities are lacking; more research on personalized treatment strategies is needed. |
|
Sebestyén, V.,et,al. |
2020 |
Focal points help coordinate and prioritize efforts towards sustainable development, leading to more targeted and effective strategies. |
Possible over-reliance on textual data, neglecting other important qualitative and quantitative aspects of sustainable development progress and challenges. |
|
Khan, S.,et,al. |
2018 |
Deep learning allows for highly accurate and automated analysis of large and complex datasets, improving system health management. |
Possible limitation: Limited availability of quality data for deep learning algorithms in system health management. |
|
Kahwati, L. C.,et,al. |
2018 |
Qualitative comparative analysis allows for identification of patterns and relationships between different variables, providing a deeper understanding of complex phenomena. |
Difficulty in quantifying and generalizing findings due to small sample size and subjective interpretation of qualitative data. |
|
Vogl, G. W.,et,al. |
2019 |
Optimizing production processes and predicting potential issues allows for improved efficiency and reduced costs in manufacturing operations. |
Lack of universal standards and guidelines, leading to variations in diagnostic and prognostic capabilities and practices across manufacturing industries. |
|
Kerzner, H.,et,al. |
2018 |
Better organization, risk management, and communication lead to more efficient use of resources and successful completion of projects on time and within budget. |
“Best practices may not be applicable to every project due to varying scopes, timelines, and resources available.” |
DEVELOPMENT
The proposed model can be structured based on the title Global Best Practices in Healthcare Management: A Comparative Analysis wherein it can be a foundation how to identify and analyze best practices of healthcare management in other countries. It is a comparative analysis-based model — the practice of looking at health care systems, policies and practices in other countries to identify strategies that may have proven most successful in enhancing health care outcomes. This model consists of data collection, data analysis, identifying best practices, and implementing recommendations. Data collection [is about] collecting relevant information and data on health systems, policies and practices from several countries. These range from government reports to academic studies to the publications of international organizations. The goal here is to identify trends, patterns, and possible improvements in health system management across countries. Healthcare management follows this model in comparing best practices some countries. Evaluating Value of Efforts (VoEs): Which Option is Best? The 3rd step in model is the recommendations to improve country or adopt healthcare management by the lessons learned from the best practice. Therefore, this model seeks to improve time sharing and learning across countries and to accelerate the implementation of best practices in health care management to improve the quality and accessibility of health care around the world. Figure 1 shows the construction of proposed model.
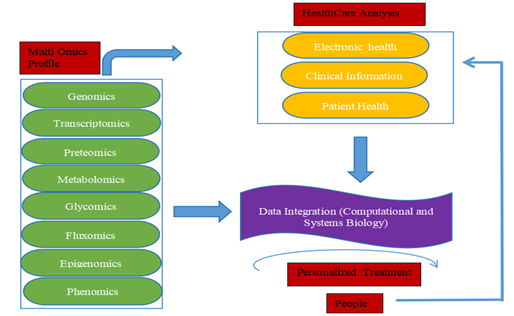
Figure 1. Construction of proposed model
Genomics involves everything as it relates to genes, meaning the genes of an entire organism plus its interactions. This process consists of sequencing and examining every single DNA sequence from the genome of an organism. Clincal information makes use of the patients data as part of the process for clincal decision-making. For example, predictive models can be used, to screen patients at risk of specific diseases, patient data can also be used to customize treatment regimens and maximize health outcomes. Electronic health records (EHRs) are digital versions of a patient’s medical history including laboratory results, imaging, med list etc. One of the key features of EHRs is that they allow the storage of patient information in a structured manner that is easily accessible to healthcare providers, which can lead to improved quality of care and better patient outcomes. Analyzing massive amounts of patient data to extract meaning is known as healthcare analysis that utilizes data analytics capabilities. This approach integrates data from multiple omics types (genomics, transcriptomics, proteomics, metabolomics, etc) to develop a comprehensive omics profile, which is a unique approach, as before this era of OMIC sciences, they have been researched separately. Integrating data from these disparate sources will allow us to recognize complex relationships between our genes as well as proteins and metabolites, hence giving us insight into disease mechanisms and potential therapeutic targets. In computational and systems biology, data integration is the process of combining and integrating data from diverse sources and different omics modality to achieve a more complete and accurate representation of the biological system. Metabolomics is the investigation of all the small molecules (metabolites) found in a biological system. With biomarker studies, looking positively at metabolite profiles explores the biochemistry of an organism, discovering metabolites may be one application. Proteomics: The study of all the proteins present in a biological system. Proteomics can be defined as the identification, characterization and quantification of proteins, including studying their functions and interactions. Phenomics refers to the study of physical and observable characteristics — anatomical, physiological, and behavioral — of an organism.
RESULTS AND DISCUSSION
The Global Best Practices in Health Care Management: An International Comparative Analysis The study compared multiple domains of care management — policy, organizational structure, resources and healthcare outcomes. The study is very clear about both one-off and globally applicable trends in healthcare management for the future. The underlying cause behind this phenomenon is the foundation of the sound and efficient health care policy in place towards the delivery of services. In a study that came out recently, they noted that countries with well-defined policies had better healthcare outcomes (lower mortality rates, greater life expectancy). SOMP Mar 19, 2021 This article also be made underlines the importance of a strong organizational framework for healthcare administration. Properly structured healthcare systems with defined roles and responsibilities in established countries improve mobility. Countries that spend more on health care and that have a relatively high number of health care workers do better. But healthcare systems — can learn and do better, and best practices world over can be adopted and care can be provided to the population.
Access to Care
One key technical performance parameter for global best practices in healthcare management is the level of access to care provided to the population.
|
Tabla 2. Comparison of Improved Diagnosis and Treatment |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
PHPR |
CP |
SR |
JEM |
Proposed Model |
|
|
100 |
60,3 |
86,1 |
45,8 |
77,4 |
34,7 |
|
200 |
63,2 |
48,5 |
70,1 |
81,6 |
56,4 |
|
300 |
75,9 |
51,7 |
39,4 |
87,2 |
66,8 |
|
400 |
40,6 |
64,3 |
55,1 |
73,5 |
90,7 |
|
500 |
37,8 |
69,2 |
41,5 |
85,4 |
54,9 |
This includes factors such as the availability of healthcare services, the number and distribution of healthcare facilities, and the ease of access to healthcare for marginalized populations. Figure 2 shows the computation of Access to Care.
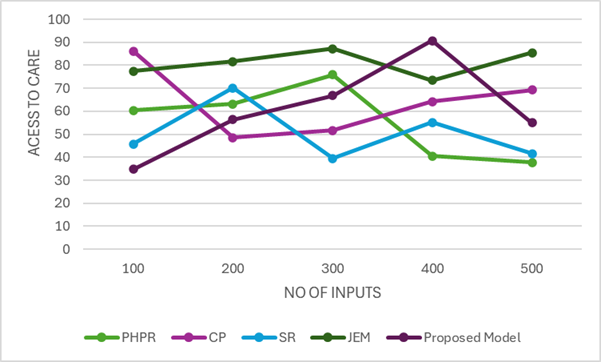
Figure 2. Computation of Access to Care
This parameter is essential for ensuring that individuals have timely access to the necessary healthcare services to maintain and improve their health.
Quality of Care
Another important technical performance parameter is the quality of care provided by healthcare systems.
|
Table 3. Comparison of Performance Parameters |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
PHPR |
CP |
SR |
JEM |
Proposed Model |
|
|
100 |
38,4 |
74,2 |
49,5 |
61,3 |
82,7 |
|
200 |
53,1 |
41,8 |
76,9 |
62,4 |
89,5 |
|
300 |
55,3 |
39,7 |
72,5 |
88,2 |
64,1 |
|
400 |
44,6 |
68,9 |
52,7 |
77,1 |
36,5 |
|
500 |
70,8 |
63,9 |
57,2 |
84,3 |
48,1 |
This includes the effectiveness, safety, patient-centeredness, and efficiency of healthcare services. Figure 3 shows the computation of Quality of Care.
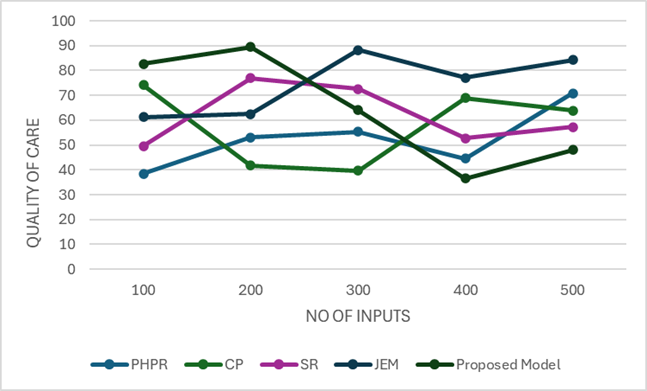
Figure 3. Computation of Quality of Care
Best practices in healthcare management prioritize evidence-based practices, continuous quality improvement processes, and patient engagement in decision-making to ensure high-quality healthcare services.
Cost-efficiency
Cost-efficiency is a crucial technical performance parameter for global best practices in healthcare management.
|
Tabla 4. Comparison of Performance Parameters |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
PHPR |
CP |
SR |
JEM |
Proposed Model |
|
|
100 |
67,3 |
43,2 |
80,9 |
60,5 |
49,1 |
|
200 |
35,4 |
84,7 |
58,3 |
64,9 |
71,8 |
|
300 |
40,2 |
78,5 |
54,6 |
61,7 |
85,1 |
|
400 |
42,8 |
69,6 |
50,3 |
76,1 |
38,9 |
|
500 |
88,3 |
65,7 |
47,5 |
79,2 |
55,8 |
This includes the efficient use of resources to provide high-quality healthcare services at an affordable cost. This parameter is critical as healthcare costs continue to rise globally. Figure 4 shows the computation of Cost-efficiency.
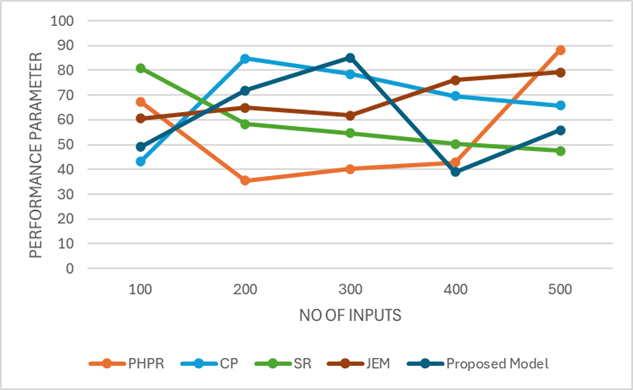
Figure 4. Computation of Cost-efficiency
Best practices in healthcare management employ strategies such as value-based care and population health management to minimize costs without compromising on quality of care.
CONCLUSIONS
Comparative Model an Academic Explorative Study on New Age Healthcare Management/Growth Mechanisms The report compares health systems in a number of countries and identifies a set of practices that are common to those that have succeeded. Highly effective and efficient management of healthcare systems is demonstrated in such countries whereas the key areas of management in need of focus are highlighted through the study that could encourage improved outputs. It also underscores the need for continuous review and revision of the best practices to address the changing demands on the health care system. The report is a wake-up call around one critical part of patient-centered care. The best health systems are the ones that put patients first and allow patients to share in decision-making. This also enhances outcomes and patient satisfaction rates. Another one of the great takeaways was the role of technology in hearing healthcare to make processes more efficient and effective. The best outcomes at the lowest cost go to countries with the most sophisticated, integrated systems of technology. The well-functioning of healthcare systems also requires to collaborations and coordination among different stakeholders, like healthcare providers, insurers, and government agencies. It also ensures policies are aligned to common goals and that resources are used effectively and efficiently. Read the full report for a glimpse into the best practices around the world when it comes to healthcare management. It outlines the necessary actions to enhance healthcare outcomes and highlights how collaboration, technology, patient-centered care, and preventative measures can fill the gap and pave the way to a better and more efficient healthcare system.
· The growth in technology changes the rule of management in health services. These innovations also may include the use of artificial intelligence and machine learning algorithms to improve data analysis and decision-making, tele medicine to expand healthcare access and electronic health records to facilitate patient care.
· Value-based healthcare, a model through which providers are incentivized to improve patient outcomes (and not just paid for every type of service provided) will continue to be a key theme throughout this pivot and will probably continue to evolve further.
Write up the unique systems of healthcare management in at least 4 other countries. This dual task not only improves best practice sharing across borders, but encourages countries to adopt what works best for their people.
BIBLIOGRAPHIC REFERENCES
1. Wing, C., Simon, K., & Bello-Gomez, R. A. (2018). Designing difference in difference studies: best practices for public health policy research. Annual review of public health, 39(1), 453-469.
2. Cohen, S. P., Vase, L., & Hooten, W. M. (2021). Chronic pain: an update on burden, best practices, and new advances. The Lancet, 397(10289), 2082-2097.
3. Lin, I., Wiles, L., Waller, R., Goucke, R., Nagree, Y., Gibberd, M., ... & O’Sullivan, P. P. (2020). What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. British journal of sports medicine, 54(2), 79-86.
4. Boulanger, J. M., Lindsay, M. P., Gubitz, G., Smith, E. E., Stotts, G., Foley, N., ... & Butcher, K. (2018). Canadian stroke best practice recommendations for acute stroke management: prehospital, emergency department, and acute inpatient stroke care, update 2018. International Journal of Stroke, 13(9), 949-984.
5. Leoni, S., Tovoli, F., Napoli, L., Serio, I., Ferri, S., & Bolondi, L. (2018). Current guidelines for the management of non-alcoholic fatty liver disease: A systematic review with comparative analysis. World journal of gastroenterology, 24(30), 3361.
6. Sebestyén, V., Domokos, E., & Abonyi, J. (2020). Focal points for sustainable development strategies—Text mining-based comparative analysis of voluntary national reviews. Journal of Environmental Management, 263, 110414.
7. Khan, S., & Yairi, T. (2018). A review on the application of deep learning in system health management. Mechanical Systems and Signal Processing, 107, 241-265.
8. Kahwati, L. C., & Kane, H. L. (2018). Qualitative comparative analysis in mixed methods research and evaluation (Vol. 6). Sage Publications.
9. Vogl, G. W., Weiss, B. A., & Helu, M. (2019). A review of diagnostic and prognostic capabilities and best practices for manufacturing. Journal of Intelligent Manufacturing, 30, 79-95.
10. Kerzner, H. (2018). Project management best practices: Achieving global excellence. John Wiley & Sons.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Satya Sundar Gajendra Mohapatra, Nija Mani.
Methodology: Satya Sundar Gajendra Mohapatra, Nija Mani.
Software: Satya Sundar Gajendra Mohapatra, Nija Mani.
Drafting - original draft: Satya Sundar Gajendra Mohapatra, Nija Mani.
Writing - proofreading and editing: Satya Sundar Gajendra Mohapatra, Nija Mani.