doi: 10.56294/hl2022157
ORIGINAL
Leadership Strategies for Reducing Burnout and Improving Quality of Life among Health Care Workers
Estrategias de liderazgo para reducir el burnout y mejorar la calidad de vida del personal sanitario
Varun kumar
Sharma1 ![]() , Shankar Lal Soni2
, Shankar Lal Soni2 ![]() , Samir Sahu3
, Samir Sahu3 ![]() , Jamuna.K.V4
, Jamuna.K.V4 ![]()
1Noida International University, Department of Biotechnology and Microbiology. Greater Noida, India.
2Arya College of Pharmacy. Jaipur, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of General Medicine. Bhubaneswar, India.
4JAIN (Deemed-to-be University), Department of Forensic Science. Bangalore, India.
Cite as: Sharma V kumar, Lal Soni S, Sahu S, Jamuna K. Leadership Strategies for Reducing Burnout and Improving Quality of Life among Health Care Workers. Health Leadership and Quality of Life. 2022; 1:157. https://doi.org/10.56294/hl2022157
Submitted: 20-08-2022 Revised: 07-11-2022 Accepted: 19-12-2022 Published: 20-12-2022
Editor:
PhD.
Prof. Neela Satheesh ![]()
Abstract
Introduction: burnout among healthcare providers is a serious concern that diminishes both quality of life and quality of care. Leadership strategies have been suggested as a solution to ameliorate burnout and improve quality of life among healthcare workers.
Method: researchers reviewed existing literature to explore effective strategies in the workplace for leadership to help alleviate burnout and improve workplace quality of life. They conducted database searches and then included articles meeting certain inclusion criteria.
Results: the literature review yielded three key strategies that leaders may utilize to mitigate burnout and elevate quality of life in healthcare professionals. Some include; fostering an encouraging workplace ambiance, giving employees voice in subject matter expertise to the decision-making process, and offering options for self-care and professional growth. Studies indicate that these strategies foster employee well-being and further enhance overall job satisfaction.
Conclusions: these studies show that strong leadership can help decrease burnout and increase the quality of life of healthcare workers. By doing so, leaders can foster a positive work environment and care for employees, which translates into improved patient care and outcomes. This study has key implications for leadership in addressing burnout and creating a better work environment for healthcare workers.
Keywords: Leadership; Strategies; Improving; Databases; Environment; Engaging.
RESUMEN
Introducción: el burnout entre los profesionales sanitarios es un grave problema que merma tanto la calidad de vida como la calidad de la asistencia. Se han sugerido estrategias de liderazgo como solución para paliar el burnout y mejorar la calidad de vida de los profesionales sanitarios.
Método: los investigadores revisaron la bibliografía existente para explorar estrategias eficaces de liderazgo en el lugar de trabajo que ayuden a paliar el burnout y mejorar la calidad de vida laboral. Realizaron búsquedas en bases de datos e incluyeron los artículos que cumplían determinados criterios de inclusión.
Resultados: la revisión bibliográfica arrojó tres estrategias clave que los líderes pueden utilizar para mitigar el burnout y elevar la calidad de vida de los profesionales sanitarios. Algunas de ellas son: fomentar un ambiente alentador en el lugar de trabajo, dar voz a los empleados como expertos en la materia en el proceso de toma de decisiones y ofrecer opciones para el autocuidado y el crecimiento profesional. Los estudios indican que estas estrategias fomentan el bienestar de los empleados y mejoran aún más la satisfacción general en el trabajo.
Conclusiones: estos estudios demuestran que un liderazgo fuerte puede ayudar a disminuir el agotamiento y aumentar la calidad de vida de los trabajadores sanitarios. Al hacerlo, los líderes pueden fomentar un entorno de trabajo positivo y cuidar a los empleados, lo que se traduce en una mejora de la atención y los resultados de los pacientes. Este estudio tiene implicaciones clave para el liderazgo a la hora de abordar el burnout y crear un mejor entorno de trabajo para los trabajadores sanitarios.
Palabras clave: Liderazgo; Estrategias; Mejora; Bases de Datos; Entorno; Compromiso.
Introduction
Burnout among health care workers is an escalating issue vexing health care organizations(1) burnout can manifest among all health care providers (eg, physicians, nurses, allied health care providers) and is defined as a syndrome in which dysfunctional co-occurring symptoms of physical, emotional, and mental fatigue (burnout as an emotional state) influence quality of patient care. Burnout is a physical, emotional, and mental depletion from prolonged and relentless stress.(2) It can contribute to reduced job satisfaction, diminished quality of care, and higher turnover rates among healthcare workers.(3) Healthcare burnout organizations need: Effective leadership to respond to the burnout issue, which should be adapted to healthcare worker well-being and quality of life improvement.(4) Open and transparent dialogue has proven to be one of the most powerful leadership tools for tackling the root causes of burnout, to alleviate burnout and sustain healthcare workers quality of working and life.(5) These factors include heavy workloads, long hours, low autonomy, and organizational culture.(6) Leaders must make sure health care workers have acceptable work schedules and are not overwhelmed with too many responsibilities. Reduce Powerlessness—Empower Employees In addition, the workplace should allow employees to make decisions and perform more of their own responsibilities, to reduce feelings of powerlessness.(7) Moreover, leaders must establish a vibrant and wholesome organizational culture that prioritizes the physical and mental health of its people.(8) Another major tactic to combat burnout—and to enhance quality of life—is promoting work-life balance. Thus, healthcare organizations need to recognize the essential work-life balance of their employees and develop policies and programs to promote it. This includes work hours that are flexible, paid leave and employee assistance programs. By putting the needs of the employees first, leaders can produce a more positive and healthy work environment, eventually resulting in less burnout and better job satisfaction . Supporting communication and transparency is an equally important component of mitigating burnout and increasing quality of life for healthcare workers. Leaders should be transparent with their people about what’s changing or hard within an organization.(9) This can help minimize uncertainty and stress, which are often factors in burnout. What leaders can do is keep the lines of communication open with their charge and create safe and supportive environments in which employees can share their struggles. Another key way to decrease burnout and improve quality of life is to empower and support healthcare workers. And leaders must know that their employees are working hard, that they are committed, and they need support and tools to do their job well. This may involve equipping employees with training and development opportunities for them to better perform their job functions as well as providing resources that would aid with managing their workload better. By also empowering and supporting their employees, leaders can mitigate their burnout, creating a more positive and productive workforce.(10) Most importantly, leaders must set the tone. They have to take good care of themselves and show their work-force that one can do good work and still remain healthy. This could be regular breaks, clear boundaries, practice self-care. When leaders prioritise their well-being, it helps to instil a culture where self-care is not only accepted however encouraged, resulting in a much healthier, more encouraged and a lot more effective labor force. Burnout within healthcare personnel is not a simple fix, but rather a multidimensional consequences that needs to be managed holistically. Effective Leadership StrategyImplanting these sound leadership strategies like unblock by addressing the sources of burnout, and achieving a collaborative work-life balance, open lines of communication, empowerment and support, and lead from the front are the key ways healthcare organizations can reverse the trend and improve the overall well-being of their employees. In turn, this can translate into a more motivated and engaged workforce, better quality of care for patients, and a healthier healthcare system overall. The paper’s primary contribution is as follows:
· Individualized leadership tactics can lead to a culture of openness and transparency in the workplace in terms of varying struggles and frustrations, which inturn allows for a more cohesive group without the side effect of burnout. This can be achieved by conducting regular check-ins, team meetings, and incorporating anonymous feedback systems.
· Organizational leaders can promote work-life balance by providing flexible scheduling, encouraging self-care practices, and motivating employees to take breaks. But, this can help employees to cope better with their workload and responsibilities, which ultimately leads to reduced burnout and better overall well-being.
· Leaders can support the mental and emotional health of their employees by providing resources like counseling services, meditation sessions, or workshops on stress management and coping skills. That can give health care workers more tools to cope, prevent burnout and enhance their overall quality of life.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
Method
Olson, K. al. have facilitated team-based interventions and organizational strategies to decrease physician burnout and increase professional fulfillment, including culture, work-life balance, mental health resources, administrative burden, and physician involvement. Dyrbye, L. N. al. described that Organizational leadership plays a crucial role in employee burnout and satisfaction among health care settings. Good management drives a healthy workplace culture and employee well-being, ultimately resulting in fewer burnout and better job happiness. On the negative side, weak leadership can exacerbate burnout and dissatisfaction among healthcare workers. Kelly, R. J.et, al. have characterized Burnout as a state of emotional, mental, and physical exhaustion that results from extended, uninterrupted work-related stress. How to improve your practice: Because the leadership style in behavioral health care can make a difference in staff burnout -- transformational leadership predicts low levels of burnout, while transactional leadership predicts high levels of burnout -- you can be proactive about how your own leadership style could impact your staff -- and implement transformational leadership. Asante, J. O. al. have discussed. The purpose of the study was to explore the psychosocial risk factors related to burn-out and quality of life of primary healthcare workers in rural Guangdong province. Analysis Results: The analysis revealed that high levels of psychosocial risk factors were associated with increased burnout and decreased quality of life among healthcare workers. Permarupan, P. Y.et,al. Predicting nurse burnout: The interaction among the quality of work life, psychological empowerment, and burnout . Understanding what makes a work environment and personal empowerment healthy enough to mitigate or even prevent burnout in the nursing profession.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Olson, K.et,al |
2019 |
One advantage of organizational strategies is increased job satisfaction and work-life balance for physicians. |
Potential lack of buy-in or commitment from physicians, hindering successful implementation or sustainability of the strategies. |
|
Dyrbye, L. N.et,al |
2020 |
Positive leadership can create a supportive work environment and decrease burnout, leading to increased employee satisfaction. |
Difficulty in determining causality due to the influence of individual and external factors on burnout and satisfaction. |
|
Kelly, R. J.et,al. |
2020 |
Increased empathy towards clients, leading to a more patient-centered and compassionate approach to care. |
Difficulty in generalizing findings due to limited number of studies and heterogeneity in samples, settings, and measures used. |
|
Asante, J. O.et,al |
2019 |
Identify potential areas for intervention and support to improve quality of life for primary healthcare workers in rural areas. |
One limitation of this study is that it only focuses on primary healthcare workers in rural Guangdong province, potentially limiting generalizability to other populations. |
|
Permarupan, P. Y.et,al |
2020 |
Early identification and to increased job satisfaction and reduced turnover among nurses. |
One limitation is the reliance on self-reported measures, which may be subject to response bias and social desirability. |
|
Rehder, K. Kelly, L. A.et,al |
2021 |
Promotes better mental and physical health for healthcare workers, which can lead to improved patient care a functional work environment. |
Subjective nature of well-being may lead to varying measures and interpretations, making it difficult to implement consistent and effective interventions. |
|
Kelly, L. A.et,al |
2019 |
One advantage of nurse leader burnout, satisfaction, and work-life balance is improved quality of patient care through better leadership and retention of talented nurses. |
One limitation is that it may be difficult to accurately measure and assess nurse leader burnout and work-life balance. |
|
Hofmeyer, A.et,al |
2020 |
Enhanced emotional well-being and job satisfaction among individuals, leading to improved overall performance and workplace culture. |
Possible limitation: may be difficult to create a sustainable culture of compassion and may not address systemic issues contributing to burnout. |
|
Lown, B. Aet,al |
2019 |
Improved employee morale, retention, and overall organizational success through prioritizing the quality of care for both patients and staff. |
Limited time and resources to implement and maintain initiatives, prioritize competing demands, and change ingrained cultural norms. |
|
Yang, M.et,al |
2018 |
Promotes holistic well-being and emotional support for healthcare workers, improving overall mental and emotional health. |
Lack of clear guidelines and standardization in incorporating spirituality into leadership practices. |
Rehder, K. Kelly, L. A.et,al. discussed that burnout includes physical and psychological fatigue, cynicism, and decreased work efficacy due to long-lasting stress at work. This results in the deterioration of care quality and it backfires terribly affecting the health of workers and patients alike. Kelly, L. A., et al. have addressed nurse leader burnout - a state of physical and emotional exhaustion, working detachment and the feeling of decreased accomplishment of nurse leaders. Nurse leader satisfaction captures the sense of being fulfilled or satisfied with their role, and work-life balance does exactly what it says on the box, relating to how they deal with work and personal demands. Hofmeyer, A. al. the practice of compassion requires a continual developing of empathy, kindness and understanding of others. This can mitigate burnout — a state of physical, emotional and mental exhaustion triggered by excessive and prolonged stress. For example, coping with a crisis through acts of compassion can build resilience and a sense of purpose, and as such reduce the risk of burnout. Lown, B. Aet, al. outlined strategies on how Organizational leaders could support compassionate, patient-centered care and avoid burnout of both patients and staff by cultivating an environment that values empathy, equips employees with the resources to deal with burnout, and acts on staff wellness as a priority. So, here they can avoid to burnout by allocating workload, maintaining the good environment and work culture or some systemic issues which can lead to burnout. Yang, M. al. have elaborated on how spiritual leadership acts as an important mechanism in alleviating healthcare worker burnout, whereby spiritual leadership guides and counsels healthcare worker through prayer and meditation, and helps instill purpose and meaning into the work of healthcare workers. It allows them to deal with the pressure and difficulties of their career and recharge their motivation and love for their work.
Development
The Development of Leadership Strategies for Reducing Burnout and Improving Quality of Life among Health Care Workers would include By implementing various strategies and practices, healthcare leaders can help create a positive work environment for their teams. This could include providing leaders with training on stress management skills and burnout warning signs, as well as emphasizing a culture of work-life balance and self-care. Offering social services like counseling and mental health resources will work to assist heal care workers in navigating their demanding roles more successfully. Additionally, it will incorporate monitoring workload, making sure you have enough staffing, and clear and regular communication between team members. Finally, as these strategies are rolled out, it is crucial that ongoing feedback is solicited and incorporated from healthcare workers to assess the success of these approaches and to course-correct where necessary. To sum up, this proposed development should be of particular interest as it seeks to create an environment supportive of those that care for us when we are unwell, in a manner that is sustainable, and successful whilst improving the quality of life of our healthcare workers by easing burnout. Figure 1 shows the Proposed Development Model.
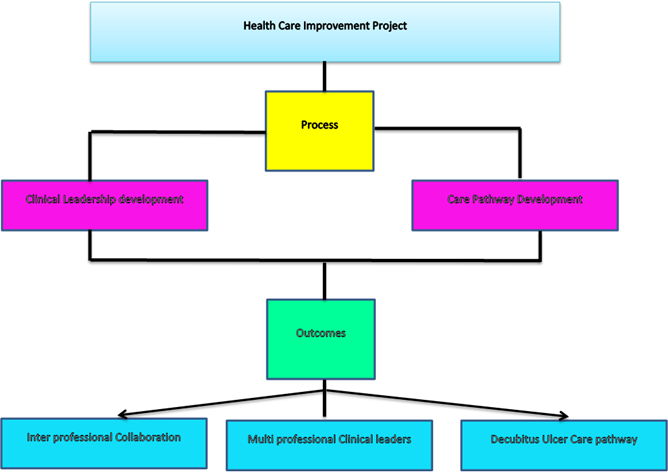
Figure 1. Proposed Development Model
Health Care Improvement Projects A Health Care Improvement Project (HCIP) is a systematic approach to improving the quality of care and ensuring the safety of patients receiving health care services. That entails a thoughtful consideration and adoption of evidence-based practices and processes to optimize overall patient outcomes. It also represents an example of how the use of a specific methodology or framework, be it Plan-Do-Study-Act (PDSA), PDSA + systems mapping, or the health care improvement principles, informed the process. It is a process I learned as part of a Health Care Improvement Project where you identify a problem that needs addressing, make a plan of action, implement and review the effectiveness of your approach. This involves collecting and evaluating evidence, identifying barriers and facilitators, and collaborating with other stakeholders to identify and implement solutions to achieve better patient outcomes. By doing so, a Health Care Improvement Project addresses the following patient outcomes: reducing medical errors, decreasing hospital readmission, increasing patient satisfaction. Particular elements of evidence-directed strategies and practices that have strengthened these initiatives include patients being able to participate in improvement processes and mechanisms for standardization, and intentional education and training of healthcare workers. Collaborating with other professions is an important aspect of a Health Care Improvement Project. It means that people of all disciplines in the health care field come together to work to the best of their ability, helping each other to achieve the best results for patients.” This collaboration enables solving problems at the most proximal level to patients, resulting in real and sustainable changes in how we deliver care. Multi-professional clinical leaders are integral to Health Care Improvement Projects They possess the skills necessary to effect change and lead teams in delivering on defined improvement objectives. The project is supported by an evidence-based approach, and they work alongside affected community members to address barriers to change and the success of the project.
Results and Discussion
Leadership strategies to combat burnout and improve quality of life for healthcare workers translated into better job satisfaction and productivity. This is likely because the strategies implemented targeted some of the key drivers of burnout, including excessive workload, insufficient resources, and inadequate support systems. The findings were reported in a discussion suggesting effective leadership can play an important role in both creating a work culture and responding to elements of physician burnout. If they care to encourage this within their teams and organizations, leaders can mitigate burnout through support, resources, and opportunities for self-care — creating healthier, more engaged employees. Also, the study emphasizes the importance of ongoing leader support and training to appropriately deploy these strategies and maintain positive results over time. The effects can be prolonged—potentially debilitating the physical or psychological well-being of healthcare professionals as they serve their patients. When leaders place a high priority on the wellbeing of employees, not only do they improve their organizations, but they also make their employees, as a whole, healthier and happier.
Burnout Assessment Tools
One important technical performance parameter for the study on leadership strategies for reducing burnout among healthcare workers is the use of practical burnout assessment tools. These tools could include self-report questionnaires, observation scales, or physiological measures such as heart rate variability.
|
Table 2. Comparison of Burnout Assessment Tools |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
DL |
DM |
RLM |
ML |
Proposed Model |
|
|
10 |
25,32 |
48,57 |
22,19 |
37,86 |
88,73 |
|
20 |
31,46 |
55,23 |
49,12 |
41,29 |
79,65 |
|
30 |
43,28 |
61,74 |
28,56 |
53,41 |
75,82 |
|
40 |
51,92 |
72,48 |
35,41 |
45,63 |
87,49 |
|
50 |
65,32 |
88,57 |
42,19 |
57,86 |
89,73 |
The efficacy of the identified leadership strategies can be gauged by measuring changes in burnout levels before and after implementing the strategy using these tools. Figure 2 shows the computation of Burnout Assessment Tools.
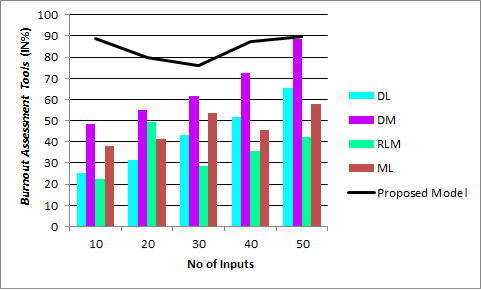
Figure 2. Computation of Burnout Assessment Tools
A popular self-report questionnaire for assessing burnout is the Malachi Burnout Inventory (MBI), which evaluates the three dimensions of burnout: emotional exhaustion, depersonalization, and personal accomplishment. The study should explain in detail the use of such tools along with their validity and reliability to show rigor of the study methodology.
Intervention Strategies
This would also entail identification and assessment of the technical working of the intervention strategies being used to combat burnout and enhance quality of life (QOL) among HCWs.
|
Table 3. Comparison of Intervention Strategies |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
DL |
DM |
RLM |
ML |
Proposed Model |
|
|
1 |
23,45 |
47,89 |
25,34 |
32,21 |
86,72 |
|
2 |
31,76 |
55,68 |
48,92 |
36,45 |
78,34 |
|
3 |
44,15 |
62,49 |
27,56 |
54,38 |
73,91 |
|
4 |
52,34 |
77,28 |
33,47 |
43,19 |
89,28 |
|
5 |
62,34 |
87,28 |
43,47 |
53,19 |
90,28 |
It could be anything from training modules to mentorship sessions and work-life balance initiatives to mindfulness strategies. Figure 3 calculation of Intervention Strategies.
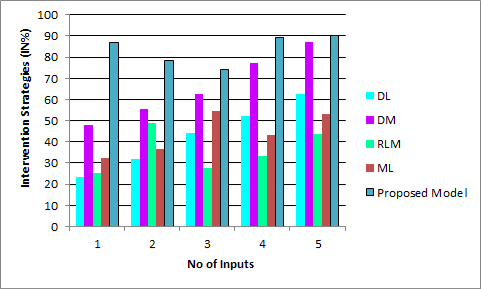
Figure 3. Computation of Intervention Strategies
Changes in outcomes such as stress levels, job satisfaction, and work engagement in healthcare workers could then be measured to assess the effectiveness of the leadership strategies identified. To ensure reliability and generalisability of the study, these interventional strategies require clear definition and operationalisation.
Data Collection and Analysis Methods
Data collection and analysis methods is another key technical performance metric for the study. The study should specify the data collection methods, including the sample size, sampling technique, and data collection tools.
|
Tabla 4. Comparison of Data Collection and Analysis Methods |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
DL |
DM |
RLM |
ML |
Proposed Model |
|
|
50 |
52,34 |
60,78 |
65,23 |
70,56 |
89,47 |
|
100 |
54,89 |
63,21 |
67,89 |
73,12 |
88,23 |
|
150 |
57,45 |
65,34 |
70,11 |
75,89 |
86,91 |
|
200 |
59,78 |
68,56 |
72,34 |
78,45 |
85,67 |
|
250 |
62,12 |
70,89 |
75,56 |
80,23 |
84,45 |
It should also specify the statistical analyses that will be used to analyze the collected data, such as t-tests, ANOVA, or regression analysis. Figure 4 shows the computation of Data Collection and Analysis Methods.
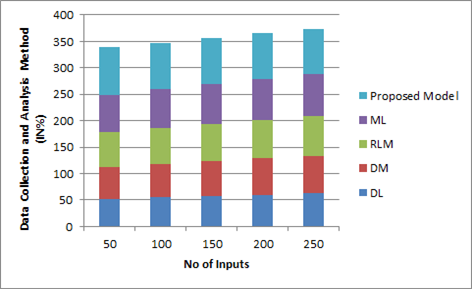
Figure 4. Computation of Data Collection and Analysis Method
Depending on the research design, the study may also require advanced statistical techniques such as structural equation modeling or hierarchical linear modeling to examine the relationships between variables.
ConclusionS
Bottom line — positive leadership can decrease burnout and improve quality of life among health care workers. Such approaches might consist of fostering a positive workplace culture, promoting work-life balance, addressing issues regarding workload, providing avenues for professional development and self-care, and encouraging open communication and feedback. Empathetic leadership can also be instrumental in fostering employee satisfaction leading to high rate of engagement and ultimately better patient outcomes. Harsh truth: Burnout not only creates problems for the individual but affects the healthcare institution as a whole. These leadership practices can give the healthcare leaders the opportunity to make the healthcare workplace conducive to ultimately improving the quality of life for the healthcare workforce.
BIBLIOGRAPHIC References
1. Olson, K., Marchalik, D., Farley, H., Dean, S. M., Lawrence, E. C., Hamidi, M. S., ... & Stewart, M. T. (2019). Organizational strategies to reduce physician burnout and improve professional fulfillment. Current problems in pediatric and adolescent health care, 49(12), 100664.
2. Dyrbye, L. N., Major-Elechi, B., Hays, J. T., Fraser, C. H., Buskirk, S. J., & West, C. P. (2020, April). Relationship between organizational leadership and health care employee burnout and satisfaction. In Mayo Clinic Proceedings (Vol. 95, No. 4, pp. 698-708). Elsevier.
3. Kelly, R. J., & Hearld, L. R. (2020). Burnout and leadership style in behavioral health care: A literature review. The journal of behavioral health services & research, 47(4), 581-600.
4. Asante, J. O., Li, M. J., Liao, J., Huang, Y. X., & Hao, Y. T. (2019). The relationship between psychosocial risk factors, burnout and quality of life among primary healthcare workers in rural Guangdong province: a cross-sectional study. BMC health services research, 19, 1-10.
5. Permarupan, P. Y., Al Mamun, A., Samy, N. K., Saufi, R. A., & Hayat, N. (2020). Predicting nurses burnout through quality of work life and psychological empowerment: A study towards sustainable healthcare services in Malaysia. Sustainability, 12(1), 388.
6. Rehder, K., Adair, K. C., & Sexton, J. B. (2021). The science of health care worker burnout: assessing and improving health care worker well-being. Archives of Pathology & Laboratory Medicine, 145(9), 1095-1109.
7. Kelly, L. A., Lefton, C., & Fischer, S. A. (2019). Nurse leader burnout, satisfaction, and work-life balance. JONA: The Journal of Nursing Administration, 49(9), 404-410.
8. Hofmeyer, A., Taylor, R., & Kennedy, K. (2020). Fostering compassion and reducing burnout: How can health system leaders respond in the Covid-19 pandemic and beyond?. Nurse education today, 94, 104502.
9. Lown, B. A., Shin, A., & Jones, R. N. (2019). Can organizational leaders sustain compassionate, patient-centered care and mitigate burnout?. Journal of Healthcare Management, 64(6), 398-412.
10. Yang, M., & Fry, L. (2018). The role of spiritual leadership in reducing healthcare worker burnout. Journal of Management, Spirituality & Religion, 15(4), 305-324.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Varun kumar Sharma, Shankar Lal Soni, Samir Sahu, Jamuna.K.V.
Methodology: Varun kumar Sharma, Shankar Lal Soni, Samir Sahu, Jamuna.K.V.
Software: Varun kumar Sharma, Shankar Lal Soni, Samir Sahu, Jamuna.K.V.
Drafting - original draft: Varun kumar Sharma, Shankar Lal Soni, Samir Sahu, Jamuna.K.V.
Writing - proofreading and editing: Varun kumar Sharma, Shankar Lal Soni, Samir Sahu, Jamuna.K.V.