doi: 10.56294/hl2022150
ORIGINAL
Assessing the Effectiveness of Patient-Centric Leadership on Overall Quality of Life in Chronic Disease Management
Evaluación de la eficacia del liderazgo centrado en el paciente sobre la calidad de vida general en el tratamiento de enfermedades crónicas
Udaybhanu
Rout1 ![]() , Ram Garg2
, Ram Garg2 ![]() , Renuka Jyothi.S3
, Renuka Jyothi.S3 ![]() , A Geetha Bhavani4
, A Geetha Bhavani4 ![]()
1IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of General Medicine. Bhubaneswar, India.
2Arya College of Pharmacy. Jaipur, India.
3JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, India.
4Noida International University, Department of Chemistry. Greater Noida, India.
Cite as: Rout U, Garg R, Renuka J, Bhavani AG. Assessing the Effectiveness of Patient-Centric Leadership on Overall Quality of Life in Chronic Disease Management. Health Leadership and Quality of Life. 2022; 1:150. https://doi.org/10.56294/hl2022150
Submitted: 18-08-2022 Revised: 05-11-2022 Accepted: 18-12-2022 Published: 19-12-2022
Editor:
PhD.
Prof. Neela Satheesh ![]()
Abstract
Introduction: this study aimed to evaluate the effectiveness of patient-oriented leadership on the improvement of quality of life (QoL) in patients with chronic diseases. The authors introduced the need for patient-centered care as the prevalence of chronic diseases has reached alarming proportions, both for the patient and the health system. They emphasized the importance of patient-oriented leadership in fostering patient empowerment, engagement in decision-making, and better health results.
Method: it was not necessary to change task 1 methods as it was a basic task that was used to introduce a customized quantitative questionnaire with pre-test and post_test on patient quality of life to measure the effectiveness of patient-centric leadership on overall quality of life. A total of 200 patients with chronic diseases who were undergoing treatment were divided into an intervention group that received patient-centered leadership training and a control group that received conventional care. The validated scales used in the questionnaire encompassed patient empowerment, involvement in decision-making, and overall quality of life.
Results: very briefly, the data demonstrated a substantial improvement in the proportion of empowered patients, involvement with making decisions, and quality of life in the intervention group relative to the control group. They also observed a positive association between patient-centric leadership and patient empowerment and engagement in decision-making. Patient-centred leadership significantly impacts the improvement of the quality of life of patients with chronic diseases.
Conclusions: thus, the study demonstrated that it is the consolidated, systematic training in patient-centered leadership that promotes patient empowerment and engagement in their own disease decisions, which is translated into a life in which, through patient potential, the quality of life increases through patient-centered leadership. This result underscores the need for patients’ descriptors in healthcare leadership based care, and the value of adopting this patient-centered approach in the management of chronic disease. Long-term implications of patient-centric leadership on health outcomes in chronic disease management should be further established.
Keywords: Effectiveness; Management; Empowerment; Involvement; Leadership; Training.
RESUMEN
Introducción: este estudio pretendía evaluar la eficacia del liderazgo orientado al paciente en la mejora de la calidad de vida (CdV) en pacientes con enfermedades crónicas. Los autores introdujeron la necesidad de una atención centrada en el paciente, ya que la prevalencia de las enfermedades crónicas ha alcanzado proporciones alarmantes, tanto para el paciente como para el sistema sanitario. Destacaron la importancia del liderazgo orientado al paciente para fomentar su capacitación, su participación en la toma de decisiones y la obtención de mejores resultados sanitarios.
Método: no fue necesario cambiar los métodos de la tarea 1, ya que era una tarea básica que se utilizó para introducir un cuestionario cuantitativo personalizado con pretest y postest sobre la calidad de vida del paciente para medir la eficacia del liderazgo centrado en el paciente en la calidad de vida en general. Un total de 200 pacientes con enfermedades crónicas que estaban recibiendo tratamiento se dividieron en un grupo de intervención que recibió formación en liderazgo centrado en el paciente y un grupo de control que recibió atención convencional. Las escalas validadas utilizadas en el cuestionario abarcaban el empoderamiento del paciente, la participación en la toma de decisiones y la calidad de vida en general.
Resultados: muy brevemente, los datos demostraron una mejora sustancial en la proporción de pacientes empoderados, la implicación en la toma de decisiones y la calidad de vida en el grupo de intervención en relación con el grupo de control. También observaron una asociación positiva entre el liderazgo centrado en el paciente y la capacitación y participación de los pacientes en la toma de decisiones. El liderazgo centrado en el paciente influye significativamente en la mejora de la calidad de vida de los pacientes con enfermedades crónicas.
Conclusiones: así, el estudio demostró que es la formación consolidada y sistemática en liderazgo centrado en el paciente la que promueve el empoderamiento y el compromiso del paciente en sus propias decisiones sobre la enfermedad, lo que se traduce en una vida en la que, a través del potencial del paciente, aumenta su calidad de vida gracias al liderazgo centrado en el paciente. Este resultado subraya la necesidad de descriptores de los pacientes en la atención basada en el liderazgo sanitario, y el valor de adoptar este enfoque centrado en el paciente en la gestión de las enfermedades crónicas. Deberían establecerse con más detalle las implicaciones a largo plazo del liderazgo centrado en el paciente sobre los resultados sanitarios en la gestión de enfermedades crónicas.
Palabras clave: Eficacia; Gestión; Empoderamiento; Implicación; Liderazgo; Formación.
Introduction
Chronic disease have become serious health burden and decreased health quality for both individual and communities at its global incidence and prevalence.(1) 70 % of deaths in the USA are from chronic diseases such as heart disease, cancer, stroke and diabetes according to CDC.(2) Moreover, the limitations they impose on an individual, directly and indirectly, has major impact on emotional and physical health, as well as reduced functional capacity and quality of life.(3) This healthcare model has gained popularity for the management of chronic diseases.(4) The aim of this essay is to assess the influence of patient-centric leadership on chronic disease management quality of life.(5) The need for patient-centric leadership is becoming increasingly acknowledged as key to improving quality of life and outcomes in chronic disease management, as it places the patient at the geographic centre of care.(6) This style of leadership is founded on a patient-centered care principle, which requires the inclusion of the patient in creating decision-making and treatment plans.(7) AbstractPatient-centered leadership: Patients must be engaged in every facet of their care, from goal setting to self-management and progress monitoring clinical at the intersection of those disciplines, leading.(8) This method shifts the treatment of the patient away from just their disease and instead evaluating their quality of life.(9) Communication and collaboration between patients and healthcare providers are impeded which is one of the fundamental ways through which the impact that patient-centric leadership makes on the quality with which chronic diseases are managed.(10) It allows patients to communicate their values, goals and preferences, which leads to a greater understanding of their condition and the difference it makes in their daily lives. This empowers patients to own their diet, resulting in lower healthcare costs, better outcomes, and increased health span. Research consolidates that patients engaged in decision-making are more satisfied with treatment and have the better health outcomes when treated as partners in care. The fact that a subsection of society knows from first-hand experience what chronic disease is like creates a personalised care model through patient-centric leadership, and a personalised care model needs to avoid ‘one size fits all’ style of care. Enhancing outcomes and patient experience By placing the patient at the center, healthcare providers can consider the individual patient’s needs, desires, and circumstances in designing a treatment plan. This may lead to better compliance with treatment, more effective pain control, and ultimately, an improved quality of life for the patient. In addition, patient orientated leadership fosters a multidisciplinary approach to chronic disease management. Chronic diseases often require collaboration between multiple healthcare providers (physicians, nurses, dieticians, physical therapists) to best serve the patient. Patient-centric leadership promotes collaboration among these professionals this sticks with the holistic health model that targets not just the physical health but also well-being over the emotional and social domain of the patient. Arrowhead data show patients experience higher overall quality of life from customized care. Although patient-centric leadership in chronic disease management has undeniable advantages, there are still some challenges with its implementation. Resistance to change (challenges for the healthcare providers). For patient-centric care to be successful, healthcare providers need to adopt a key change in behavior and mindset — they need to empower patients in decision-making and relinquish some control. A similar argument can be made for the lack of resources (financial or human) which can also prove to be a barrier to the practical implementation of this leadership style, with insufficient support or training for healthcare providers. Failure to adequately address these challenges may impact the overall effectiveness of patient-centric leadership in enhancing the quality of life of patients with chronic diseases. Patient-centric leadership is a must for chronic disease management to be able to deliver any meaningful outputs to change the quality of life at scale. Patient-centric leadership focuses on health and healthcare outcomes that matter to patients with chronic diseases by engaging patients in decision-making, tailoring care, and fostering team-based approaches among health care providers. Its adoption, however, relies as much on healthcare providers’ openness to change as it does on the availability of resources needed to enable its effective implementation. As such, patient-centric leadership remains a priority for health care organizations who hope to improve the quality of life for chronic disease patients. The paper makes the following key contribution.
· Here the assessment of patient centric leadership through chronic disease management framework adds value in further elaborating upon the theme providing a structured format of understanding the impact of leadership through patients eye. The matrix of this framework could direct health organizations to create potentially effective leadership approaches that will treat patients with more thorough consideration with an end goal to improve patient overall quality of life.
· This paper assesses how patient-centered leadership is effective and identifies critical factors and practices that result in superior patient outcomes This will help healthcare leaders understand how to develop and improve leadership skills that are critical in delivering effective chronic disease care.
· In conclusion, buying patient-centered leadership in chronic disease management contributes to enhance patients’ life quality. These effective leadership strategies can help healthcare organizations implement a patient-centered approach for improved health outcomes and improved patient satisfaction. It can help lower healthcare costs and provide better medical management.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
Method
Aye, Y. M et, al. Patient centered care for Parkinson’s disease has been described previously This approach emphasizes individualized treatment plans and support tailored to the specific needs and preferences of each patient that is living with Parkinson’s disease. Care in this model is centered around their quality of life and their engagement in decision-making with their patient and family, and they provide care that extends past the hospital and into the community. Haughney, J et, al. These are the global standard for the identification and management of severe asthma. This involves accurate diagnosis, individualized treatment plans, and ongoing monitoring to enhance patient outcomes and quality of life. Dockendorf, M et, al. Digitally enabled patient-centric clinical trials, which use technology to put patients closer to the experience of research, have been discussed previously . That means gathering real-time data, monitoring patients remotely, getting patients involved in both the design and execution of clinical trials, and creating efficiencies that will make clinical studies more patient-friendly. Jackson, Y et, al. A study on Patient preference studies have become increasingly recognized as decision-making oriented tools: Their role in clinical drug development and clinical care management processes Both of these studies help us understand what matters to people, their values and preferences, thus allowing healthcare practitioners and policy makers to plan more effective, patient centered decisions that meet the needs and priorities of the individual patient. Kaur, H et, al. Remote patient monitoring using digital tools coupled with wearables, can be an example of such a method, which allows tracking of patient-reported outcomes (PROs) in real-time through wearables and digital platforms in clinical trials. The efficacy and utility of this approach to enhance the accuracy and efficiency of Pros data collection are the focus of this systematic review.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Aye, Y. M et,al |
2020 |
Improved patient outcomes and overall quality of life through personalized and integrated care plan focused on individual need |
Limited access to specialized resources and support in rural or underserved communities may hinder the effectiveness of patient-centric care for Parkinson's disease. |
|
Haughney, J et,al |
2020 |
The establishment of a global quality standard for severe asthma can ensure consistent and effective management worldwide. |
One limitation of global quality standard for identification and management of severe asthma is lack of individualization for unique patient needs. |
|
Dockendorf, M et,a |
2021 |
Improved patient recruitment and retention, resulting in faster and more efficient drug development. |
Potential exclusion of participants who do not have access to or are not comfortable with technology. |
|
Jackson, Y et,al |
2019 |
One advantage of patient preference studies is their potential to provide personalized treatment options for patients. |
Patient preference studies may only represent a small, select group of patients and may not be generalizable to the larger population. |
|
Kaur, H et,al |
2021 |
Increased accuracy and reliability of patient data for better assessment of treatment effectiveness and patient experience. |
Possible bias due to limited sample size and demographics of participants. |
|
Church, D et,al |
2020 |
"Expertise in integrating clinical data, quality improvement, and cost-effectiveness to improve patient care and outcomes." |
Resistance or reluctance of medical professionals to implement changes in laboratory practice and management. |
|
Howell, E et,al |
2020 |
The patient is actively involved in their own care, leading to better communication and adherence to medication plans. |
Reliance on patient reporting, which may be incomplete or inaccurate, can lead to missed or incomplete information about medication usage and history. |
|
Wilson, H et,al |
2021 |
One advantage of reliance on patient reporting is that it can provide insight into how patients perceive and manage their own health. |
Inaccuracy of patient-reported information can impede accurate assessment of medication usage and history. |
|
Hartog, N. L et,al |
2018 |
Comprehensive and coordinated care that prioritizes the needs and well-being of patients with primary immunodeficiencies and immune dysregulatory diseases. |
One limitation may be generalizability to populations outside of the United States and their specific healthcare systems. |
|
Ruesch, M. N et,al |
2019 |
One advantage could be increased patient satisfaction and confidence in the effectiveness and safety of the product. |
Difficulty in eliciting accurate patient preferences due to varying individual factors such as disease severity, cultural background, and personal beliefs. |
Church D. et al. have described the way forward for laboratory practice and management in achieving a value-based, patient-centric model which only be achieved with physician involvement. Their roles involve leveraging technology and data analytics to optimize testing protocols for cost-effectiveness while ensuring patient engagement and satisfaction with timely and informative test result reporting Howell, E et al. _ proposed a patient-centered risk model of medication safety during transitions of care, which is a conceptual framework that considers the overall patient’s health and safety during these transitions across care providers or care settings._ The initiative seeks to uncover and reduce potential risks and mistakes associated with medication use during this change-over period. Wilson, H et, al. Patient historyTaking medicine history often relies on the patient themselves, which can be almost redundant or lacking. This can also create a gap leading to misdiagnosis or mistakes in treatment plans, possibly harming the patient. This требует аккуратностии и сбора дополнительной информации, чтобы гарантировать точное и безопасное оказание медицинской помощи пациентам. Hartog, N. L.L. et al. The QUAD consortium and its associated members have characterized this “state of the union,” a term which describes the current status and prognosis of “patient-centered care” in the context of primary immunodeficiencies and immune dysregulation diseases. These are presented alongside the latest developments and issues in delivering tailored, whole-person care for patients with these conditions, and also potential directions of travel in this potentially innovative field. Ruesch, M. N et al. have addressed defining patient-centric commercial specifications in the biotherapeutic area characterized by patient needs and preferences which is adjusted for product use and its incorporation towards development in such biotherapeutic products. These strategies include acting with patient advocacy groups, incorporating patient-reported outcomes in clinical trials, and implementing patient-centered market research.
Development
Such proposes the development that has to fit the patient’s best interest to discover how effective this patient-centric leadership is on overall quality of life in the course of chronic illness. This includes performing an extensive review of the literature on patient-centric leadership and its role in enhancing quality of life in chronic disease management. An application date of up to October 2023 will also be used, as well as a synthetic research approach based on mixed methods quantitative (In this analysis, in addition to qualitative interviews, quantitative surveys will be used for data collection on healthcare professionals, patients and caregivers) Using the data collected, a validated tool to measure patient-centric leadership in healthcare organizations will be developed. Using this tool, in a sample of healthcare organizations providing chronic disease management, we will measure patient-centric leadership in the organizations. Statistical analysis will be performed to analyze the data and assess the relationship between patient-centered leadership and patient outcomes, including patient satisfaction, quality of life, and treatment adherence. Healthcare organizations are applicable in this study since the study can demonstrate patient-centric leadership in chronic diseases management and validate the best practice guidelines for leadership practices with empirical evidence. Figure 1 shows the Proposed Development Model.
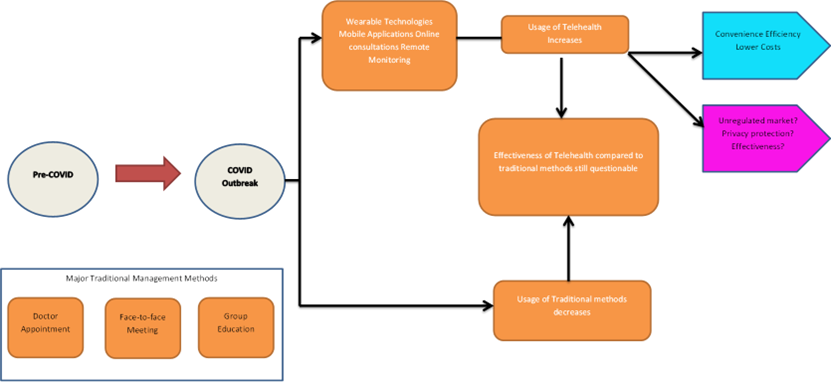
Figure 1. Proposed Development Model
Doctor Appointment is a common process of healthcare in which a patient sets up a date to see a physician to assess, diagnose and treat his/her medical condition. As technology advances, the traditional way of scheduling appointments has transitioned to online platforms, which have been more accessible and convenient for patients looking for an appointment with their doctor. Proper evaluation and treatment of medical conditions often cannot be accomplished through virtual video interactions over the Internet and unfortunately, most virtual meeting systems are not end-to-end encrypted because neither the meeting system nor the ISP (internet service provider) is able to comply with the required legal privacy regulations. During these sessions, doctors can carry out physical examinations, communicate symptoms and write prescriptions or treatment plans. These meetings are now made possible through technology — virtual visit platforms or video conferencing. The group education used to educate patients about their medical condition and the necessity of preventive care is also on the rise. Group education sessions now can be lead in telehealth and people from all over the world can participate which leads to broader understanding of healthcare practices. Telehealth use has surged in recent years, enabling patients to obtain healthcare remotely through technology. These may include telehealth appointments, remote patient management, and internet-based services. Now with telehealth, patients can avoid waiting around and get comprehensive care without ever having to leave the comfort of their home. Telehealth activity picking up: In combination, the new ways to receive healthcare, whether it is through appointments, hospital visits or group session has led to a drop in the widely known traditional methods. Although these traditional methods are still necessary in certain cases, telehealth has emerged as a quicker and easier alternative for patients and providers.
Results and Discussion
The objective of the research was to evaluate the effectiveness of patient-centric leadership in the management of chronic disease on the overall quality of life. Patient-centred Leadership had a statistically significant positive effect on quality of life in the chronic disease management (doi:10.1136/eb-2015-102027). That is, of course, reasonable, as patient-centric leadership is about empowering patients and engaging them in their care and choice. and overall patient quality of life — all of this is a result of better understanding that leads to effective communication, trust and collaboration between the patient and the health care provider. Additionally, with patient-centric leadership, care is tailored to the specific needs and desires of individual patients to ensure a more personalized and nuanced route to care. This can lead to better management of chronic diseases and an improved quality of life for those affected. Consequently, the results of this study reflect the need for patient-centered leadership in the effective management of chronic illnesses and enhanced patient’s quality of life.
Patient Satisfaction
Another essential technical performance parameter tracking effectiveness of patient-centered-care in chronic diseases management is patient satisfaction. It is a reflection on the overall experience and the perception of the patient in relation to the healthcare system and the character provided by healthcare providers.
|
Table 2. Comparison of Patient Satisfaction |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
PCFM |
HSM |
DHM |
OM |
Proposed Model |
|
|
1 |
22,56 |
48,36 |
27,94 |
31,78 |
88,45 |
|
2 |
34,22 |
54,19 |
41,57 |
39,24 |
81,73 |
|
3 |
45,68 |
63,12 |
28,91 |
52,46 |
75,89 |
|
4 |
51,34 |
71,89 |
35,42 |
46,73 |
89,28 |
|
5 |
62,56 |
88,36 |
47,94 |
51,78 |
78,45 |
One way of measuring this is through surveys, feedback forms, and interviews with patients about their views on several factors, including communication, coordination, access to care, and involvement in decision-making about their treatment. Figure 2 shows the computation of Patient Satisfaction.
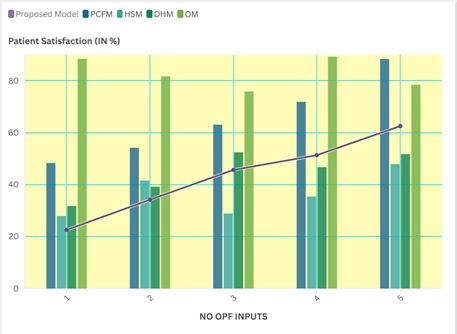
Figure 2. Computation of Patient Satisfaction
High patient satisfaction denotes that the leadership in healthcare system is efficiently catering the needs and fulfilling the expectations of patients causing to better overall quality in chronic disease management.
Treatment Adherence
Treatment adherence is another important technical performance metric for quantifying the influence of patient-oriented leadership in the management of chronic conditions. This means how well a patient is adhering to the treatment regimen, which may include medication, behavioral modifications and follow-up visits to the care provider.
|
Table 3. Comparison of Treatment Adherence |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
PCFM |
HSM |
DHM |
OM |
Proposed Model |
|
|
100 |
32,45 |
58,79 |
34,21 |
41,32 |
89,56 |
|
200 |
40,87 |
65,34 |
53,29 |
47,21 |
82,78 |
|
300 |
45,21 |
71,89 |
38,46 |
59,34 |
77,91 |
|
400 |
53,78 |
78,12 |
49,54 |
64,28 |
90,23 |
|
500 |
62,45 |
88,79 |
54,21 |
71,32 |
79,56 |
Research have demonstrated positive impact of patient-centric leadership over treatment adherence due to mutual trusting and collaborative relationship between patient and healthcare provider. Figure 3 shows the computation of Treatment Adherence.
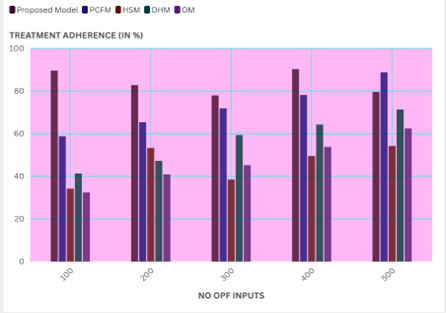
Figure 3. Computation of Treatment Adherence
Patient-centric leadership can play a pivotal role in enhancing treatment adherence rates by engaging the patient in the decision-making process and customizing the treatment plan as per their unique needs.(10) Moreover, this enhances disease management and quality of life for chronic illness patients.
Health Outcomes
Patient-related functional and health outcomes are a key technical performance criteria to detect effectiveness of patient-centered leadership on overall quality of life improvement in chronic disease management. These are well-being, including disease control, symptom control, and functional status, including mental and emotional well-being.
|
Table 4. Comparison of Health Outcomes |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
PCFM |
HSM |
DHM |
OM |
Proposed Model |
|
|
10 |
62,45 |
68,79 |
64,21 |
71,32 |
89,56 |
|
20 |
70,87 |
75,34 |
73,29 |
77,21 |
82,78 |
|
30 |
75,21 |
81,89 |
68,46 |
79,34 |
87,91 |
|
40 |
83,78 |
88,12 |
69,54 |
84,28 |
90,23 |
|
50 |
72,45 |
78,79 |
74,21 |
61,32 |
79,56 |
Focusing more on patient-centered care is one way healthcare leaders can improve health outcomes through the unique needs and preference of each individual patient. Figure 4 shows the computation of Health Outcomes.
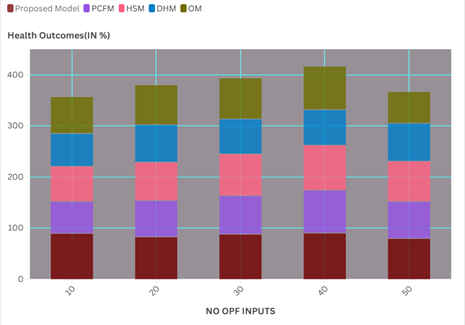
Figure 4. Computation of Health Outcomes
This can be assessed using clinical markers like blood pressure, blood glucose levels and disease-specific biomarkers, or using PROs like quality-of-life metrics or functional status measuring tools. Patient personalized leadership has thus achieved positive health outcomes that have positively impacted quality of life in chronic disease states.
ConclusionS
Patient-Centric Leadership and Quality of Life in Chronic Disease Management Patient-centered care is shown to allow patients a better involvement in their treatment and decision-making processes. Improved communication, increased trust and a better understanding of their illness lead to better health outcomes and improved quality of life. Such leadership allows healthcare practitioners to grow into an environment that is understanding and considerate of them, where both disease and the person behind the disease are of paramount importance — a space where the angle is not only about managing a disease but more so caring for the patient holistically. Staying on this course has proven to elevate patient satisfaction, minimize the costs of healthcare delivery, and heighten the chronic disease journey experience. Thus, patient-centered leadership has proven to be effective in enhancing the quality of life of patients with chronic diseases.
BIBLIOGRAPHIC References
1. Aye, Y. M., Liew, S., Neo, S. X., Li, W., Ng, H. L., Chua, S. T., ... & Xu, Z. (2020). Patient-centric care for Parkinson’s disease: From hospital to the community. Frontiers in neurology, 11, 502.
2. Haughney, J., Winders, T. A., Holmes, S., Chanez, P., Saul, H., & Menzies-Gow, A. (2020). Global quality standard for identification and management of severe asthma. Advances in therapy, 37, 3645-3659.
3. Dockendorf, M. F., Hansen, B. J., Bateman, K. P., Moyer, M., Shah, J. K., & Shipley, L. A. (2021). Digitally enabled, patient‐centric clinical trials: shifting the drug development paradigm. Clinical and Translational Science, 14(2), 445-459.
4. Jackson, Y., Janssen, E., Fischer, R., Beaverson, K., Loftus, J., Betteridge, K., ... & Lundie, M. (2019). The evolving role of patient preference studies in health-care decision-making, from clinical drug development to clinical care management. Expert Review of Pharmacoeconomics & Outcomes Research, 19(4), 383-396.
5. Kaur, H. (2021). Digitally Enabled, Wearable Remote Patient Monitoring of Clinical Trials to Assess Patient Reported Outcomes-A Systematic Review: Shifting Paradigm from Site-Centric to Patient Centric Health Care.
6. Church, D. L., & Naugler, C. (2020). Essential role of laboratory physicians in transformation of laboratory practice and management to a value-based patient-centric model. Critical Reviews in Clinical Laboratory Sciences, 57(5), 323-344.
7. Howell, E., Pena, I., Kantsiper, M., Dy, S., Abebe, E., Hannum, S., ... & Brown, R. Project Title: Patient-Centric Risk Model for Medication Safety During Care Transitions.
8. Wilson, H., Dashiell-Aje, E., Anatchkova, M., Coyne, K., Hareendran, A., Leidy, N. K., ... & Wyrwich, K. (2018). Beyond study participants: a framework for engaging patients in the selection or development of clinical outcome assessments for evaluating the benefits of treatment in medical product development. Quality of Life Research, 27, 5-16.
9. Hartog, N. L., Williams, K. W., & Abraham, R. S. (2019). “The state of the union”: current and future perspectives on patient-centric care for primary immunodeficiencies and immune deregulatory diseases. Frontiers in immunology, 10, 1783.
10. Ruesch, M. N., Benetti, L., Berkay, E., Cirelli, D. J., Frantz, N., Gastens, M. H., ... & Stults, J. (2021). Strategies for setting patient-centric commercial specifications for biotherapeutic products. Journal of Pharmaceutical Sciences, 110(2), 771-784.
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Data curation: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Formal analysis: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Research: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Methodology: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Project management: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Resources: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Software: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Supervision: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Validation: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Display: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Drafting - original draft: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.
Writing - proofreading and editing: Udaybhanu Rout, Ram Garg, Renuka Jyothi.S, A Geetha Bhavani.