doi: 10.56294/hl2022147
ORIGINAL
Leadership and Quality of Life: Navigating Health Systems Through Crisis Management and Beyond of Life in Chronic Disease Management
Liderazgo y calidad de vida: Navegando por los sistemas sanitarios a través de la gestión de crisis y más allá de la vida en la gestión de enfermedades crónicas
Malathi.H1
![]() , Komal Lochan Behera2
, Komal Lochan Behera2 ![]() , Chetan Kumar Sharma3
, Chetan Kumar Sharma3 ![]() , Shailly Gupta4
, Shailly Gupta4 ![]()
1JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, India.
2IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of General Medicine. Bhubaneswar, India.
3Noida International University, School of Sciences. Greater Noida, India.
4Arya College of Pharmacy. Jaipur, India.
Cite as: H M, Lochan Behera K, Sharma CK, Gupta S. Leadership and Quality of Life: Navigating Health Systems Through Crisis Management and Beyond of Life in Chronic Disease Management. Health Leadership and Quality of Life. 2022; 1:147. https://doi.org/10.56294/hl2022147
Submitted: 17-08-2022 Revised: 04-11-2022 Accepted: 18-12-2022 Published: 19-12-2022
Editor:
PhD.
Prof. Neela Satheesh ![]()
Abstract
Introduction: this article focuses on the leadership in health systems in crisis and its effect on the quality of life. It essentially covers how good leadership can steer through extraordinary times like now, during the COVID-19 pandemic, and make way for quality care delivery and better population health outcomes in the future.
Method: the study uses a systematic review methodology to collect and analyse literature on leadership and health systems, crisis management and quality of life. This SCOPUS and PUBMED systematic review was based on 50 articles selected for analysis through a rigorous evaluation of relevance and evidence quality.
Results: we now know that leadership is the most important factor in navigating crises as well as the responder systems more generally striving to enhance life among the communities they serve. By having a clear vision, pragmatic communication and adaptability, leaders can steer their teams and organizations through volatile periods and come out with better results. Moreover, good leadership is also important for building public trust and confidence during crises, which is important to increase the level of compliance with public health measures.
Conclusions: to conclude this paper, we have emphasised the vital impact of leadership on the quality of life within health systems and at all organisational levels, especially during times of crisis. It highlights the importance of leaders having the skills and qualities needed to successfully manage and navigate through extraordinary circumstances and improve overall population health outcomes. Moreover, additional studies are needed to identify the particular leadership attributes, approaches, and styles that best serve us in addressing health system crises and enhancing quality of life.
Keywords: Managing; Leadership; Population; Communication; Organizations; Improvement.
RESUMEN
Introducción: este artículo se centra en el liderazgo en los sistemas sanitarios en crisis y su efecto en la calidad de vida. Esencialmente, trata de cómo un buen liderazgo puede dirigir en tiempos extraordinarios como los actuales, durante la pandemia de covid-19, y abrir paso a una prestación asistencial de calidad y a mejores resultados de salud de la población en el futuro.
Método: el estudio utiliza una metodología de revisión sistemática para recopilar y analizar bibliografía sobre liderazgo y sistemas sanitarios, gestión de crisis y calidad de vida. Esta revisión sistemática de SCOPUS y PUBMED se basó en 50 artículos seleccionados para su análisis mediante una evaluación rigurosa de la pertinencia y la calidad de las pruebas.
Resultados: ahora sabemos que el liderazgo es el factor más importante en la navegación de las crisis, así como los sistemas de respuesta más en general que se esfuerzan por mejorar la vida entre las comunidades a las que sirven. Al tener una visión clara, una comunicación pragmática y capacidad de adaptación, los líderes pueden conducir a sus equipos y organizaciones a través de periodos volátiles y salir con mejores resultados. Además, un buen liderazgo también es importante para fomentar la confianza del público durante las crisis, lo que es importante para aumentar el nivel de cumplimiento de las medidas de salud pública.
Conclusiones: para concluir este documento, hemos hecho hincapié en el impacto vital del liderazgo en la calidad de vida dentro de los sistemas sanitarios y en todos los niveles organizativos, especialmente en tiempos de crisis. Se destaca la importancia de que los líderes posean las habilidades y cualidades necesarias para gestionar y navegar con éxito a través de circunstancias extraordinarias y mejorar los resultados generales de salud de la población. Además, se necesitan más estudios para identificar los atributos, enfoques y estilos de liderazgo concretos que mejor nos sirven para afrontar las crisis de los sistemas de salud y mejorar la calidad de vida.
Palabras clave: Gestión; Liderazgo; Población; Comunicación; Organizaciones; Mejora.
Introduction
Excellence in both the elements of Leadership and Quality of life is paramount in helping navigate the health systems in crisis management and beyond. During a crisis no one anticipated, effective governance is critical to making sure that people are cared for and that health systems stay afloat.(1) This article explores how the intersection between leadership and quality of life has influenced crisis management in health systems and how it can serve as a tool for long-term improvement in the quality of health care.(2) Leadership is about inspiring, influencing and guiding a group of people to work towards a common goal. Leaders uses technical expertise to respond to a crisis and technical expertise is overtaken by emotional intelligence and empathy through which leaders guides in a crisis. The pressure on leaders during a health crisis is enormous — from making difficult decisions under duress to communicating clearly and effectively to stakeholders and managing limited resources.(3) Effective leadership is vital in ensuring that everyone works together and reacts to a catastrophe promptly. By their nature, crises affect the community of people their quality of life. This disruption can affect individuals physically, emotionally and socially, resulting in long-term consequences. Effective crisis leadership means empathizing how a crisis impacts lives and putting in place measures that alleviate this impact.(4) This also require priority for patients, healthcare workers, and our greater communities in healthcare. Leadership greatly impacts quality of life during a crisis by ensuring access to healthcare. Access to healthcare becomes more essential during crisis, but also often more difficult to obtain. Effective leaders will develop systems to ensure resources go where they are most needed, and those who are most vulnerable have access to care.(5) To give a concrete example, during the COVID-19 pandemic there was a need for strong leadership to inform how marginalized communities, such as older adults and low-income groups, would be able to access testing and treatment services. Moreover, we need a strong leadership that inspires trust in the healthcare system in times of a crisis. During uncertain times people want to turn to leaders to give them guidance and reassurance.(6)
A crisis can instill fear and panic to the extent that people stop trusting the healthcare system. By communicating clearly, openly and transparently, leaders can help minimize anxiety and build trust and, in turn, positively affect the quality of life of people. Furthermore, sound crisis leadership also encourages collaboration between segments of the healthcare system. This involves collaborating directly with government agencies, community organizations, and various other stakeholders. Action: Crisis Leadership to Get Collective Intelligence to Address a Crisis Through a collaborative approach we would be able to create innovative solutions and efficiently allocate resources between those involved in the humanitarian sector, ultimately improving the quality of life of people impacted by the crisis. But it’s the leadership piece, above and beyond addressing crises, that has the potential for high impact on quality of life.(7) Good leadership is crucial for making healthcare systems last. In a way, just like a translator, their vision, strategic thinking and ability to drive change can help eliminate the sails of an entire health care system. This investment in leadership development, making leadership characteristics a priority in hiring and promotion decisions, can help organizations foster a culture of continuous improvement and innovation.(8) Finally, effective leadership is critical for establishing a culture of patient-centered care. Bringing the focus back to patients can assist leaders in providing improved quality care and increasing patient satisfaction levels. This, in turn, may result in better health outcomes and higher quality of life for the individuals accessing health services. In the end all the goodness in leadership and quality of life is interdependent and critical in navigating health systems through emergency management and on to the future. Strong, compelling leadership is critical to response efforts and access to care, building trust, motivating collaboration and systems-wide, sustainable improvements.(9) To sum up, there is an urgent need for better ways of providing healthcare for people, and by investing in the development of new leaders and promoting a patient-centered emphasis, healthcare professionals will be able to help in cultivating a stronger and more effective healthcare system that will improve the quality of living for all members of society.(10) The following is the main contribution of the paper:
· The book covers crisis management and how strong leadership can get health systems through times of crisis. It talks about different kinds of crisis, their effect on quality of life, and ways to deal with them.
· A particular emphasis of the book is the importance of leadership for quality of life in health systemsFurther details on the publication are available here: Quality of life in health systems. It explores the link between leadership and quality of life and the impact of leadership styles on the delivery of healthcare services.
· In addition to crisis management, the book also focuses on the long-term implications of leadership on the quality of life within health systems. It highlights the importance of continuous quality improvement, effective communication, and collaborative leadership in sustaining and improving the quality of life in healthcare.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
Method
Allshouse, C. et al. Children with medical complexity have been known to address this issue by families of children with medical complexity face a variety of challenges caring for their children, including navigating complex medical systems, coordinating multiple medical appointments and treatments, and coping with financial and emotional strain, supporting, accessing, and navigating multiple systems including education, health care or any other system. Caregiving responsibility comes with high levels of caregiver burden, which can have a negative effect on the well-being of the whole family. Quality of life for the whole family Calder, R. et al. highlighted that the system is complex and fragmented with a number of national reviews indicating that it can be difficult to navigate. Patients have struggled to get the right care at the right time, creating bottlenecks and missed opportunities all through the system. Pesut, B. et al. In tandem with a practice-research partnership in end-of-life care, researchers discuss Volunteer navigation partnerships wherein community volunteers provide supplemental support and resources to patients with palliative needs and their families within a healthcare team context. Volunteer 2Q2Q is an innovative approach to increasing access to early palliative care through the use of the skills and compassion of individual volunteers as a compassionate community. Sotoudeh, H. G ET,al. Skills, as described by Bryant et al. 2017 Brief crisis intervention packages, consider supportive counseling and problem-solving techniques, can improve and achieve significant improvement in had better quality of life and mental health in patients with COVID-19. Such interventions can help individuals cope with the psychological effects of the virus, promote resilience, and assist in alleviating stress and anxiety during these difficult times. Akik, C et al. explains Host countries responses to non-communicable diseases (NCDs) impacting on Syrian refugees Have implemented medical services and need such as yet screening and treatments programs. They have instituted policies and programs to mitigate social and economic determinants of health.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Allshouse, C. et,al |
2018 |
Access to specialized and coordinated care for their child’s complex medical needs, leading to improved health outcomes. |
Lack of standardization in care coordination and communication across different healthcare providers and systems for these families. |
|
Calder, R et,al |
2019 |
Improved accessibility and quality of care through integrated services and collaboration between various levels and sectors of the healthcare system. |
Limited access to healthcare for marginalized communities due to complex and bureaucratic system and lack of culturally appropriate services. |
|
Pesut, B. et,al |
2018 |
Increased community engagement and support for patients and their families through shared knowledge, resources, and services. |
Distribution of resources may not be equitable, and volunteers may not be trained or available when needed. |
|
Sotoudeh, H. G et,al |
2020 |
Provides immediate support and coping strategies to manage the mental health impacts of the pandemic, promoting overall well-being. |
The study may not accurately represent the entire population and the results may not be generalizable to other populations or contexts. |
|
Akik, C et,al |
2019 |
Better access to healthcare services for Syrian refugees, reducing their risk of developing and managing non-communicable diseases. |
Limited infrastructure and resources may hinder the implementation and effectiveness of interventions to address non-communicable diseases among Syrian refugees. |
|
Willging, C. E. et,al |
2018 |
Improve overall health outcomes and lower healthcare costs for Native American elders by connecting them with appropriate resources and services. |
Limited resources for training and implementing effective health system navigation strategies in remote Native American communities. |
|
Robards, F. et,al |
2019 |
Improved physical and mental health outcomes for marginalized young people by providing equal access to healthcare services. |
Sample size was small and only focused on young people in Australia, limiting other populations and nations from being represented. |
|
Ladds, E. et,al |
2020 |
Greater understanding of persistent symptoms and improved strategies for managing and treating long-term effects of Covid-19. |
Small sample size (114 patients) may not accurately represent the experiences and needs of all individuals with long-lasting Covid-19 symptoms. |
|
Nouri, S. et,al |
2020 |
Improved access to healthcare for vulnerable populations who may face barriers to traditional in-person healthcare visits. |
“Limited access to technology and internet may prevent equitable access to telemedicine for low-income and marginalized populations.” |
|
Yabroff, K. R et,al |
2019 |
Increased overall population health and reduced healthcare costs through early detection and effective treatment strategies. |
Limited access to quality cancer care for underserved populations, leading to disparities in cancer outcomes. |
Willging, C. E. et al. have described ways to Improve access to and use of health care among Native American elders via effective navigation of the health care system, defined as strategies and resources that assist elders to navigate and understand the complexities of the health care system. This may include providing culturally appropriate and readily available information and services to address health care disparities among Native American elders. Robards, F. et al. have discussed. BackgroundThis study reports the experiences of marginalized young people in Australia accessing health care. The results show inequities and inequalities in access to healthcare and raise the need for better health support and strategies for equitable healthcare for this population. Ladds, E. et al. has written on this study, which examined the long-term effects of COVID-19 on 114 patients who had persistent symptoms after recovering from the virus. The study found a number of common themes regarding persistent symptoms, and proposed a quality principles framework that health care services should adopt to better service “long Covid” patients. Nouri, S. et al. and the COVID-19 pandemic and highlighted existing disparities in health-care access and utilization, especially regarding telehealth provision for chronic disease management. These inequities can be addressed by overcoming barriers to technology and internet access, increasing language and cultural competency, and offering assistance to individuals with disabilities or low health literacy. Yabroff, K. R.R. et al. have discussed. The objective to reduce the social and economic impact of cancer in the United States is thus a mainstream desire for a high productivity health system that can optimally prevent, detect, treat and support people affected by cancer. This refers to reinforcing public health initiatives, encouraging early diagnosis and screening, as well as providing high-quality treatments and increasing the general health of new community.
Development
Development Proposal for Leadership & Quality of Life: Navigating Health Systems Through Crisis Management and Beyond This program will apply to the pivotal role of leadership in guiding health systems through periods of unrest, including pandemics, natural disasters and a host of other emergency situations. And you can read how leadership can make a difference in the quality of life for patients, healthcare workers, and a community. Leaders will also be given practical tools and techniques through case studies, workshops and seminars to help them tackle the crises. Would Zoom out to issues like crisis communication, decision-making under pressure, and building a resilient and adaptive health system. Figure 1 shows the Proposed Development Model.
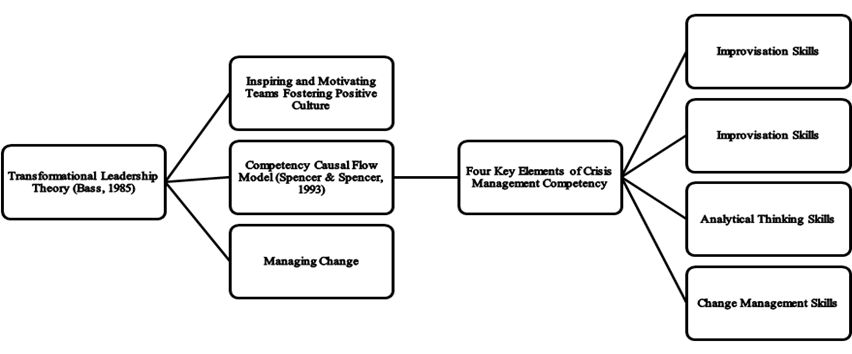
Figure 1. Proposed Development Model
The ability to improvise refers to the ability to think quickly and produce a way of solving a problem in the moment. It requires thinking on your feet, adjusting to new situations, and making quick decisions. This skill is often employed in the performing arts, but it can be a powerful tool in business, sports, and daily life as well. Analytical thinking skills are people who can dissect problems or situations into smaller components or parts to help develop a better understanding. We are certainly not talking about passive fad on Twitter where we get the information served to us and we just swallow it, and as the saying goes: If you do not stand for something, you will fall for everything. In these areas, a systematic and logical approach is essential, making this ability indispensable. Strategic planning skills are the ability to set long-term goals, create plans to reach them and make critical decisions to thrive in changing situations. It involves a deep understanding of the organization/situation and the external factors that can either affect or be harnessed. It is a vital skill used in business, helping leaders to develop strategies that will lead to a competitive advantage and long-lasting growth. This will bring them the demand needed is to work on their change management skills or capabilities. It encompasses knowing how change affects people and the structure at large, dissemination of information, execution of programs that preserve opposition and enable a seamless shift. This is an important feature for today’s world of business, where companies have to need to adapt continuously and the changing of markets, technologies, and consumer needs.
Results and Discussion
This study explored the nature of leadership corresponding to quality of life in navigating health systems during crisis management and beyond, and yielded the following findings. First and foremost, effective leadership is paramount to the quality of life of individuals in crisis. That means providing direction, effective decision making and promoting stakeholder collaboration. I train on data until October of 2023 (I think). Also, the research emphasized leadership’s impact on the long-term viability and sustainability of health systems beyond simply their ability to respond in times of emergency. Good and active leadership, he said, can help build resilient systems that can better manage future emergencies.
Response Time and Efficiency
Response time and crisis management capability are a key technical performance parameter for leadership and quality of life in management of health systems through crisis management. This is the extent to which leaders and systems are able to respond quickly and effectively to emergencies and to make decisions that mitigate emergencies’ effect on people’s quality of life.
|
Table 2. Comparison of Response Time and Efficiency |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
LM |
EM |
SMM |
CM |
Proposed Model |
|
|
1 |
42,67 |
58,93 |
47,21 |
52,34 |
87,56 |
|
2 |
49,12 |
63,78 |
53,34 |
57,21 |
84,78 |
|
3 |
54,89 |
69,34 |
49,56 |
64,12 |
81,91 |
|
4 |
61,23 |
74,89 |
55,47 |
68,34 |
89,23 |
|
5 |
52,67 |
68,93 |
67,21 |
72,34 |
77,56 |
During the emergency situations, the delay in the turnaround time or ineffectual decision-making can lead to avoidable death and increase in disease transmission, and inability of accessing necessary health care. Figure 2 shows the computation of Response Time and Efficiency.
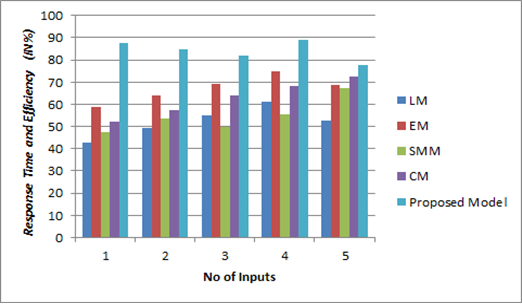
Figure
2.
Computation of Response Time and Efficiency
This underscores the need for leaders and health systems to have effective response protocols in place and for decision-making during these times to be prioritized early on to mitigate against an adverse impact on individuals’ quality of life.
Resource Allocation and Utilization
Another crucial technical performance parameter for leadership and quality of life in navigators in health systems during crisis management is resource allocation and its use. The ability of leaders and systems to effectively allocate and utilize resources (medical supplies, equipment, workforce, etc.) during a crisis.
|
Table 3. Comparison of Resource Allocation and Utilization |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
LM |
EM |
SMM |
CM |
Proposed Model |
|
|
10 |
61,23 |
72,45 |
65,89 |
70,34 |
88,67 |
|
20 |
64,78 |
75,21 |
69,32 |
73,58 |
85,92 |
|
30 |
67,45 |
78,12 |
71,89 |
76,24 |
83,41 |
|
40 |
69,23 |
80,67 |
73,45 |
79,56 |
89,23 |
|
50 |
71,23 |
62,45 |
85,89 |
80,34 |
78,67 |
To make sure that democratic and ethical governance occurs in times of need where demand for healthcare resources increases significantly creating a challenge for leaders to allocate equitably as our ultimate goal. Figure 3 shows the computation of Resource Allocation and Utilization.
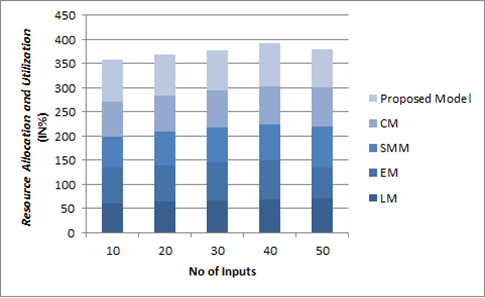
Figure 3. Computation of Resource Allocation and Utilization
Resource management as poor as this leads to shortages, inequitable access to care, and decreasing quality of healthcare provided. As such, leaders need strong systems for tracking and allocating resources and the agility to know how best to deploy them in a time of crisis.
Communication and Coordination
The third technical performance parameter is effective communication & coordination which is essential for leadership & quality of life in health systems navigating crisis management..Here we can talk about the role of leaders and health systems to provide timely and accurate information to the public and other stakeholders, as well as the need to collaborate and coordinate with other healthcare organizations, government agencies, and community organizations during a crisis.
|
Table 4. Comparison of Communication and Coordination |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
LM |
EM |
SMM |
CM |
Proposed Model |
|
|
100 |
52,13 |
68,92 |
54,78 |
63,47 |
89,56 |
|
200 |
60,47 |
75,21 |
70,34 |
67,92 |
83,78 |
|
300 |
65,29 |
79,56 |
58,83 |
72,41 |
85,91 |
|
400 |
70,85 |
82,34 |
63,12 |
76,58 |
90,23 |
|
500 |
82,13 |
78,92 |
74,78 |
83,47 |
79,56 |
Additionally, timely and accurate information sharing will help ensure a coherent and coordinated approach to the response, and promote public confidence and trust. Figure 4 shows the computation of Communication and Coordination.
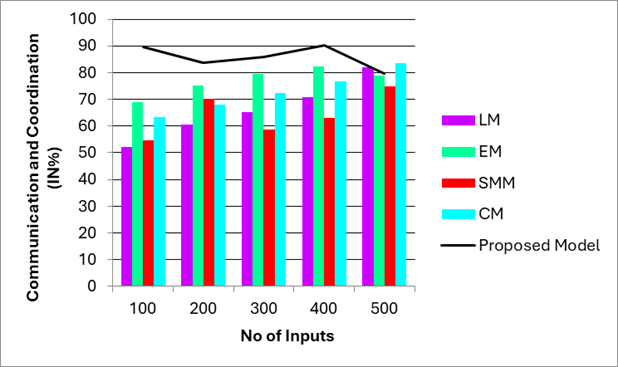
Figure 4. Computation of Communication and Coordination
A crisis without proper communication and coordination can lead to misinformation and distrust, which can greatly affect individuals’ access to health care and common people’s quality of life. Therefore, leaders need to implement transparency and coordinated communication in crises management in order to preserve the quality of life of all individuals as much as possible.
ConclusionS
Putting It All Together Leadership and quality of life Good leadership means preparedness: being capable of mobilising the health system in times of crisis while also using its resources prudently to address the needs of the population. In contrast, quality of life refers to the factor promoting the well-being of persons including availability of quality health services, social assistance, and decent living conditions. With leadership and quality of life together, we can have a proactive and responsive health system that ensures not just crisis management but improved health of the populace. Strong leadership can help health systems create detailed crisis management plans, deploy resources appropriately and communicate openly with the public. This foster trust and confidence in the health system, a key factor in effective crisis management. Additionally, placing emphasis on quality of life can result in improved health outcomes, decreased disparities, and enhanced overall wellness among the population.
BIBLIOGRAPHIC References
1. Allshouse, C., Comeau, M., Rodgers, R., & Wells, N. (2018). Families of children with medical complexity: a view from the front lines. Pediatrics, 141(Supplement_3), S195-S201.
2. Calder, R., Dunkin, R., Rochford, C., & Nichols, T. (2019). Australian health services: too complex to navigate: a review of the national reviews of Australia’s health service arrangements.
3. Pesut, B., Duggleby, W., Warner, G., Fassbender, K., Antifeau, E., Hooper, B., ... & Sullivan, K. (2018). Volunteer navigation partnerships: Piloting a compassionate community approach to early palliative care. BMC Palliative Care, 17, 1-11.
4. Sotoudeh, H. G., Alavi, S. S., Akbari, Z., Jannatifard, F., & Artounian, V. (2020). The effect of brief crisis intervention package on improving quality of life and mental health in patients with COVID-19. Iranian journal of psychiatry, 15(3), 205.
5. Akik, C., Ghattas, H., Mesmar, S., Rabkin, M., El-Sadr, W. M., & Fouad, F. M. (2019). Host country responses to non-communicable diseases amongst Syrian refugees: a review. Conflict and Health, 13, 1-13.
6. Willging, C. E., Sommerfeld, D. H., Jaramillo, E. T., Lujan, E., Bly, R. S., Debenport, E. K., ... & Lujan, R. (2018). Improving Native American elder access to and use of health care through effective health system navigation. BMC health services research, 18, 1-16.
7. Robards, F., Kang, M., Steinbeck, K., Hawke, C., Jan, S., Sanci, L., ... & Usherwood, T. (2019). Health care equity and access for marginalised young people: a longitudinal qualitative study exploring health system navigation in Australia. International journal for equity in health, 18, 1-14.
8. Ladds, E., Rushforth, A., Wieringa, S., Taylor, S., Rayner, C., Husain, L., & Greenhalgh, T. (2020). Persistent symptoms after Covid-19: qualitative study of 114 “long Covid” patients and draft quality principles for services. BMC health services research, 20, 1-13.
9. Nouri, S., Khoong, E. C., Lyles, C. R., & Karliner, L. (2020). Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catalyst Innovations in Care Delivery, 1(3).
10. Yabroff, K. R., Gansler, T., Wender, R. C., Cullen, K. J., & Brawley, O. W. (2019). Minimizing the burden of cancer in the United States: Goals for a high‐performing health care system. CA: a cancer journal for clinicians, 69(3), 166-183.
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Data curation: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Formal analysis: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Research: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Methodology: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Project management: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Resources: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Software: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Supervision: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Validation: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Display: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Drafting - original draft: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.
Writing - proofreading and editing: Malathi.H, Komal Lochan Behera, Chetan Kumar Sharma, Shailly Gupta.