doi: 10.56294/hl2022137
ORIGINAL
A Comprehensive Assessment of Improper Medical Waste Disposal and Its Effects on Environmental Health
Evaluación exhaustiva de la eliminación inadecuada de residuos médicos y sus efectos en la salud ambiental
Dillip Kumar Dash1 ![]() , Mohammad Asif2
, Mohammad Asif2 ![]() , Pooja Varma3
, Pooja Varma3 ![]() , Shankar Lal Soni4
, Shankar Lal Soni4 ![]()
1IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Paediatrics. Bhubaneswar, India.
2Noida International University, School of Liberal Arts. Greater Noida, India.
3JAIN (Deemed-to-be University), Department of Psychology. Bangalore, India.
4Arya College of Pharmacy. Jaipur, India.
Cite as: Dash DK, Asif M, Varma P, Lal Soni S. A Comprehensive Assessment of Improper Medical Waste Disposal and Its Effects on Environmental Health. Health Leadership and Quality of Life. 2022; 1:137. https://doi.org/10.56294/hl2022137
Submitted: 14-08-2022 Revised: 01-11-2022 Accepted: 16-12-2022 Published: 17-12-2022
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Improper medical waste disposal poses significant environmental and health risks. Investigation on its impact, focusing on factors like healthcare facility type, worker training, and waste management infrastructure is crucial. To assess the relationship between improper waste disposal and environmental health outcomes is the main aim of this research. Surveys were conducted with 150 healthcare workers and 50 waste management personnel across local hospitals and clinics to gather data on disposal practices and health impacts. Data was analyzed using SPSS Version 28 to explore relationships between variables, including healthcare facility type, training level, infrastructure, regulatory enforcement, and waste segregation practices, impacting environmental health outcomes. Descriptive statistics and multiple regression analysis, highlighting key factors influencing improper disposal. Descriptive statistics were employed to summarize and present key characteristics of the dataset, such as frequencies, means, and standard deviations, offering an overview of the sample’s demographic details and waste disposal practices. Additionally, multiple regression analysis was conducted to explore the relationships between variables like environmental health outcomes (e.g., pollution levels). Multiple regression analysis showed strong correlations between waste segregation practices and environmental health outcomes (p < 0,05). Improper medical waste disposal poses significant environmental health risks, with insufficient training and infrastructure identified as major contributors. Policy changes and improved waste management practices are recommended.
Keywords: Medical Waste Disposal; Environmental Health; Descriptive Statistics; Multiple Regression Analysis.
RESUMEN
La eliminación inadecuada de residuos médicos plantea importantes riesgos para el medio ambiente y la salud. Es crucial investigar su impacto centrándose en factores como el tipo de centro sanitario, la formación de los trabajadores y la infraestructura de gestión de residuos. Evaluar la relación entre la eliminación inadecuada de residuos y los resultados para la salud ambiental es el principal objetivo de esta investigación.
Se realizaron encuestas a 150 trabajadores sanitarios y 50 empleados de gestión de residuos de hospitales y clínicas locales para recabar datos sobre las prácticas de eliminación de residuos y su impacto en la salud. Los datos se analizaron con el programa SPSS versión 28 para explorar las relaciones entre variables como el tipo de centro sanitario, el nivel de formación, la infraestructura, la aplicación de la normativa y las prácticas de segregación de residuos, que influyen en los resultados de salud ambiental.
Las estadísticas descriptivas y el análisis de regresión múltiple pusieron de relieve los factores clave que influyen en la eliminación inadecuada.
Se emplearon estadísticas descriptivas para resumir y presentar características clave del conjunto de datos, como frecuencias, medias y desviaciones estándar, ofreciendo una visión general de los detalles demográficos de la muestra y de las prácticas de eliminación de residuos. Además, se realizó un análisis de regresión múltiple para explorar las relaciones entre variables como los resultados de salud ambiental (por ejemplo, los niveles de contaminación). El análisis de regresión múltiple mostró fuertes correlaciones entre las prácticas de segregación de residuos y los resultados de salud ambiental (p < 0,05). La eliminación inadecuada de residuos médicos plantea importantes riesgos para la salud ambiental, y la formación y las infraestructuras insuficientes son los principales factores que contribuyen a ello. Se recomienda modificar las políticas y mejorar las prácticas de gestión de residuos.
Palabras clave: Eliminación de Residuos Médicos; Salud Ambiental; Estadística Descriptiva; Análisis de Regresión Múltiple.
INTRODUCTION
Medical waste plays an important role in the spread and exacerbation of diseases. This issue is particularly prevalent in developing countries. Healthcare waste poses significant hazards, including increased risks of disease and injury. Various sector’s involvement in recycling medical waste further exacerbates disease transmission risks, mainly for waste collectors, scavengers, and recycling workers.(1) Medical waste disposal is the process of securely handling and getting disposed of trash produced in healthcare facilities, including clinics, hospitals, labs, and other medical establishments. Medical waste includes items like used syringes, gloves, surgical instruments, bandages, medications, and any other materials polluted with bodily fluids or infectious agents.(2) The presence of medical waste can really destroy the environment, public health, and spread infectious diseases if it is not disposed properly. The improper disposal of medical waste, like throwing it into ordinary trash or unsanitary incineration, causes severe health hazards. Among these are harmful exposures to hazardous materials, infections, and pollution from air, water, and soil.(3) Proper medical waste disposal would require strict stipulations and protocols for treating, sorting, and disposing of waste safely. The process usually requires segregation of wastes, sorting into different categories by risk level, and then treating using autoclaving, incineration, or chemical disinfection.(4) Secure storage, transportation, and documentation ensure that there is no risk of cross-contamination. The relevance of medical waste disposal goes beyond healthcare facilities. It affects surrounding communities and the ecosystems in which the healthcare facilities operate.(5) Medical waste is growing, particularly during medical emergency, and needs strong systems for sustainable and responsible management of such waste for individual health and the environment.(6)
Hazardous substances, such as infectious materials, heavy metals, and toxic chemicals, can leach into the environment if not properly treated or discarded, as expressed in figure 1.(7) In addition, contaminated medical waste in water bodies may pose very significant risks to public health, disrupt ecosystems, and affect communities dependent on safe water sources.(8) This could facilitate the transmission of infections, harm to wildlife, and long-term contamination of natural resources. Inadequate disposal methods, like burning or dumping waste improperly, can produce harmful pollutants into the atmosphere, affecting air quality.(9) Improper medical waste disposal can significantly influence environmental health by contaminating air, water and soil.(10) Therefore, the current research to investigate the improper medical waste disposal poses significant environmental and health risks, leading to pollution and contamination of natural resources. Effective waste management practices, including proper segregation and infrastructure improvements, are crucial to mitigating these risks and safeguarding public health.

Figure 1. Healthcare waste generative places
Research Objective
The improper medical waste disposal and its effects on environmental health were investigated. The focus is on assessing how these factors influence environmental health outcomes, such as pollution levels and public health risks. By surveying healthcare workers and waste management personnel, the research will explore the relationships between these variables and identify the primary challenges in waste disposal practices. The findings will provide insights into the role of training, infrastructure, and regulatory compliance in waste management. Based on these insights, recommendations will be made to improve waste management systems, with the goal of minimizing environmental and health hazards associated with improper medical waste disposal.
Key Contributions
· To examine the impact of healthcare facility type, worker training, and waste management infrastructure on improper medical waste disposal practices through surveys conducted with 150 healthcare workers and 50 waste management personnel.
· To assess the relationship between waste segregation practices and environmental health outcomes by analyzing survey data using descriptive statistics and multiple regression analysis.
· To explore the influence of regulatory enforcement on medical waste disposal effectiveness, using survey responses to evaluate compliance and practices.
· To identify the primary challenges in waste disposal by analyzing demographic details and waste disposal practices across different healthcare settings.
Research Organization
Section 2 reviews related works, including various methods that have been applied to examine the impact of poor medical waste disposal. Section 3 describes data collection, research design, and methods. Section 4 outlines the findings from the statistical analysis, while Section 5 provides a summary of the discussion based on these results. Lastly, the findings, limitations, and future research in Section 6.
Related works
A multi-criteria model to evaluate infectious waste management in a large healthcare unit was developed.(11) The methods involved applying pair wise comparison matrices to assess scale factors, indicators, criteria, and sub-criteria. The results showed strong environmental management but highlighted the need for improved staff awareness and sustainable procurement. Limitations included limited staff engagement and green supplier diversity, suggesting opportunities for further improvement. Medical waste management based on world health organization (WHO) guidelines was applied to private and public hospitals were investigated.(12) Multi-criteria decision making (MCDM) techniques were used to structure the evaluation criteria, with data collected from questionnaires, checklists, and interviews conducted with healthcare personnel. Results showed proper waste segregation but reliance on unsafe disposal methods and inadequate treatment facilities. Restrictions included weak technical guidelines, poor enforcement, and insufficient monitoring, emphasizing the need for regulations, technologies, expertise, and funding.
COVID-19 hospital and biomedical waste management were analyzed with a focus on disinfection technologies and strategies.(13) The method involved examining global initiatives and the utilization of several disinfection methods to reduce health and environmental risks. From the results, improper disposal of COVID-waste, especially personal protective equipment, posed significant public health and environmental hazards. Waste management practices were constrained by the reliance on secondary data, which may not have accurately reflected real-time scenarios. The COVID-19 pandemic's heightened waste disposal issues and need to investigate reaction strategies that were discussed.(14) It also sought to propose effective responses to mitigate risks associated with improper waste handling. The methods involved reviewing the surge in medical and infectious waste, particularly from healthcare facilities and homes, and evaluating existing waste management practices. The findings revealed that improper waste management increased virus transmission risks. A limitation of the research was the reliance on existing guidelines, which may not have fully addressed the unique challenges posed by the pandemic.
The widely used plastics on a daily basis and their potential risks to the atmosphere as well as individual health that were examined.(15) The approach utilized existing works that gave information regarding the toxicity of plastics. The results showed that the plastic polyvinyl chloride has high toxicity. Insignificant drawbacks to this research was a lack of further detailed descriptions concerning the additive combined effects with varied plastic types. The administration of healthcare wastes (HCWs) between health workers and associated factors in primary healthcare facilities was investigated.(16) A cross-sectional health facility survey was conducted, where health workers were interviewed about their knowledge, attitudes, and practices regarding HCW management. The results showed that most health workers had high knowledge of HCW management and practiced appropriate safety measures when handling HCWs. The survey was limited by self-reported data, which may have introduced response bias.
The investigation explored healthcare waste management practices to gather data that can guide policy decisions.(17) A cross-sectional approach was used, and quantitative data were gathered from respondents working in major healthcare facilities. From the results, improved training and provision of personal protective equipment (PPE) to healthcare professionals to enhance the waste management practices. Major healthcare facilities were prioritized, which may have overlooked waste management practices in smaller or rural settings. Medical waste disposal technologies were evaluated by comparing energy recovery, environmental impact, and economic cost.(18) Life cycle assessment (LCA) as well as Energy recovery analysis (ERA) techniques were employed. The results revealed that steam and microwave sterilization combined with burning had the enhanced energy recovery efficiency, while plasma melting had the lowest. The evaluation was constrained by the exclusion of emerging medical waste disposal technologies that could offer alternative solutions.
Research Gaps
Although increasing awareness of improper medical waste disposal risks exists, the research in this area remains woefully inadequate. Specifically, there is little investigation of the complex relationship between specific healthcare facility types, training programs, and infrastructure quality as the individual relate to managing waste. Indeed, despite findings that identify inadequately trained workers and insufficient infrastructure, little research investigates how these elements differ across healthcare settings or how enforcement of regulatory efforts affect outcomes. Moreover, the role of emerging technologies in waste management has not been sufficiently evaluated, and hence potential solutions have remained unexplored. More studies need to be done to determine whether policies and technological advancements can indeed reduce the medical waste-related environmental and health hazards. Thus, the present research seeks to bridge these gaps by assessing the impacts of waste management practices and providing practical recommendations for improvement.
METHOD
Statistical techniques were employed to examine the impact of improper medical waste disposal on environmental health outcomes, focusing on variables, such as healthcare facility type, worker training, and waste management infrastructure. The proposed relationships and factors influencing improper disposal are presented in figure 2.
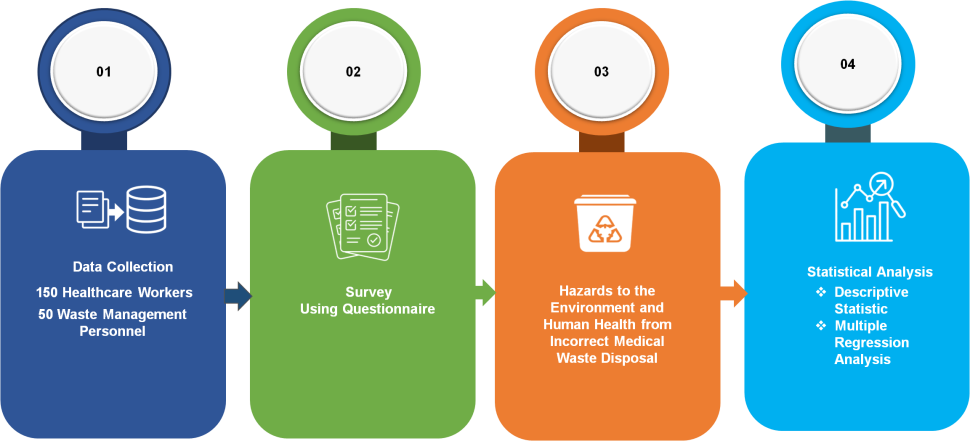
Figure 2. Overall Proposed Flow Diagram
Data Collection
Data were collected using questionnaires from 150 health care workers and 50 waste management personnel in local hospitals and clinics. Questions covered practices in disposal, training levels, infrastructure, and the health implications of the improper disposal of medical waste. The participants were selected according to their various roles: the role being played either in regard to waste management or healthcare provision. Various demographic information, including age and gender, years of experience, and particular roles in healthcare and waste management, were also taken. The survey assisted in getting insights into the current practices in waste disposal and their implications for environmental health. Table 1 summarizes demographic details of participants.
|
Table 1. Details of the Participants |
|
|
Demographic details |
N=200 |
|
Age |
|
|
18-26 yrs |
70 |
|
26- 38yrs |
90 |
|
39-47yrs |
30 |
|
48 and above |
10 |
|
Gender |
|
|
Male |
120 |
|
Female |
80 |
|
Role |
|
|
Healthcare Worker |
150 |
|
Waste Management Personnel |
50 |
|
Years of Experience |
|
|
0-5 yrs |
80 |
|
6-10 yrs |
60 |
|
More than 11 yrs |
60 |
|
Healthcare Facility Type |
|
|
Hospital |
120 |
|
Clinic |
80 |
Survey Questionnaires
Interviews were conducted with healthcare professionals and waste handlers for the analysis of their activities and attitudes toward the disposal of medical waste. The questionnaire included the following: training programs, techniques of segregation, quality of infrastructure, regulatory compliance, and environmental health impact through improper disposal. The respondents replied to various dimensions of managing waste disposal on likert scale (Completely Disagree to Completely Agree). In the questionnaire, environmental health risks posed by improper disposal were also perceived, adherence to regulatory guidelines and the prevalence of problems of waste segregation issues were also taken into account. The results serve as practical recommendations for improving medical facility waste management practices. A 5-point Likert scale used to rate the answers is presented in table 2.
|
Table 2. Survey Questionnaires for Participants |
|
|
S.NO |
Questions |
|
1 |
How often do you receive training on proper medical waste disposal? |
|
2 |
Do you feel adequately equipped to manage medical waste at your facility? |
|
3 |
How would you rate the waste management infrastructure at your facility? |
|
4 |
Is waste segregation practices followed consistently at your facility? |
|
5 |
To what extent do you believe improper medical waste disposal contributes to environmental health risks? |
|
6 |
How frequently do you encounter issues with waste segregation or disposal at your facility? |
|
7 |
Are regulatory guidelines for waste disposal strictly enforced at your facility? |
|
8 |
In your opinion, what improvements are needed in waste disposal practices to minimize environmental health risks? |
Hazards to the environment and human health from incorrect medical waste disposal
The hazardous dispersal of medical wastes into the environment poses a high threat to the healthcare staff and the large community. Crucial factors that have led the situation to worsen include lack of resources, lack of legislative powers, and poor knowledge among waste operatives. Most of the healthcare institutions do not have an environmental management plan, and very few employees and senior officials are conversant with WHO guidelines on proper disposal practices. Hazardous substances like pharmaceutical waste and heavy metals are frequently released into sewer systems or dumped close to agricultural land, causing pollution, ecosystem disruption, and even the potential contamination of water sources.
Evaluation segregation system
Improper medical waste disposal practices were prevalent across healthcare establishments (HCEs), as observed in table 3, which presents the composition of the generated waste. Many establishments collected waste without segregation, placing it in general municipal bins, where it was subsequently handled by local authorities.
|
Table 3. Medical Waste Distribution in Surveyed Healthcare Facilities |
|
|
Category of Waste |
Approximate Waste Generated (kg/day) |
|
Harmless General Waste |
28,200 |
|
Hazardous Pathological Waste |
1,500 |
|
Hazardous Infectious Waste |
850 |
|
Pharmaceutical Waste |
700 |
|
Hazardous Chemical Waste |
900 |
|
Toxic Waste |
800 |
Additionally, medical waste, including blood-stained materials and anatomical body parts, was disposed in domestic bins, drains, and sewerage systems. Table 4 illustrates that the majority of HCEs employed partial or no segregation of waste, further compounding environmental and health risks.
|
Table 4. Disposal Practices in Surveyed Healthcare Establishments (HCEs) |
|||
|
Healthcare Facility Type |
Proper Disposal |
Partial Disposal |
No Disposal |
|
Local Hospital |
2 |
3 |
1 |
|
Clinic |
5 |
6 |
21 |
|
Diagnostic Center |
6 |
8 |
44 |
Statistical Variables
Improper medical waste disposal poses significant environmental and health risks, requiring an in-depth analysis of contributing factors. The variables involved in this research are as follows.
· Healthcare Facility Type: Categorizes healthcare establishments based on their nature (e.g., hospital, clinic), to explore how facility type impacts waste disposal practices and environmental outcomes.
· Worker Training Level: Measures the extent of training healthcare and waste management personnel receives, assessing how training influences proper waste disposal and health risks.
· Waste Segregation Practices: Examines whether medical waste is effectively segregated into appropriate categories, influencing the efficiency and safety of disposal methods.
· Infrastructure Quality: Evaluates the adequacy and functionality of waste management infrastructure in healthcare facilities, determining its role in supporting proper disposal practices.
· Pollution Levels: Quantifies the degree of environmental pollution (e.g., air, water) associated with improper waste disposal, linking waste management practices to health outcomes.
Statistical Analysis
Relationships between improper medical waste disposal and environmental health outcomes were analyzed by using statistical methods with the statistical Package for the Social Sciences (SPSS) Version 28. Descriptive statistics summarized key characteristics of the data, and multiple regression analysis examined the impact of variables.
Descriptive statistics
Summarizing as well as organizing information through measures, this helps to highlight its key features, including variability and central tendency. This approach captures the essential characteristics of the dataset, such as participants' demographic details and waste disposal practices, providing the necessary context for further analysis of factors influencing environmental health outcomes.
Multiple regression analysis
The association among improper medical waste disposal and healthcare facility type, worker training, waste management infrastructure, regulatory enforcement, and waste segregation practices was examined by using a regression model. This analysis identifies the impact and significance of these factors on environmental health outcomes.
![]()
X2 is a training Level, X1 represents a facility type, environmental health outcomes are denoted by Y from improper medical waste disposal and waste segregation is evaluated by X5. The model identifies key contributors to waste disposal issues, with ∈ representing the error term.
RESULTS
The statistical findings exposed in this section offer an examination of connections between environmental health effects and healthcare waste disposal strategies.
Descriptive Statistics
This type of statistics is used to analyze key variables like healthcare facility type, worker training, waste segregation, infrastructure quality, and pollution levels, revealing patterns and variability in the data that are established in table 5. Figure 3 shows the outcomes of variables and their mean values.
|
Table 5. Outcome Values for Variables |
|||||||
|
Variable |
SD |
Max |
Median |
Kurtosis |
Mean |
Min |
Skewness |
|
Healthcare Facility Type |
1,10 |
5 |
3 |
-1,30 |
2,65 |
1 |
0,45 |
|
Worker Training Level |
0,85 |
5 |
3 |
-0,97 |
3,21 |
1 |
-0,02 |
|
Waste Segregation Practices |
1,05 |
5 |
3 |
-1,03 |
2,94 |
1 |
0,15 |
|
Infrastructure Quality |
1,12 |
5 |
3 |
-0,97 |
2,58 |
1 |
0,36 |
|
Pollution Levels |
0,95 |
5 |
3 |
-1,30 |
3,10 |
1 |
0,12 |
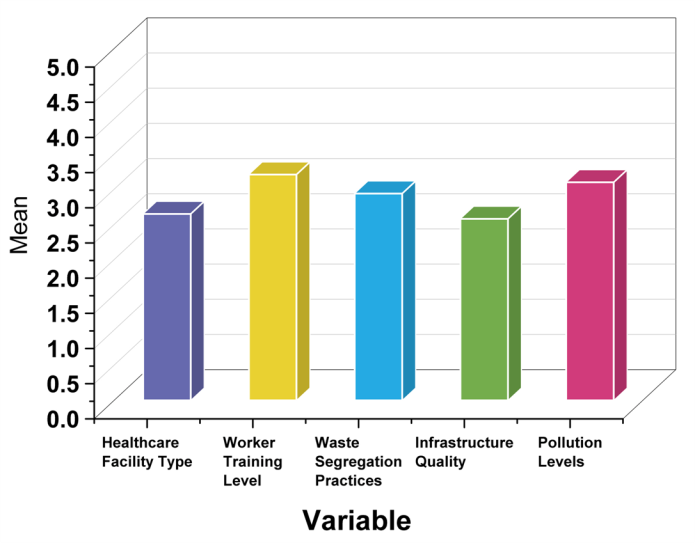
Figure 3. Comparison between Variables and Mean
The mean of 2,65 for healthcare facility type indicates a mix of facilities, mostly medium-sized, with a slight skew towards smaller ones (0,45). Worker training level (mean = 3,21) suggests generally well-trained staff, with minimal skew (-0,02). Waste segregation practices (mean = 2,94) are slightly below average, with a slight positive skew (0,15). Infrastructure quality (mean = 2,58) is below average, and pollution levels (mean = 3,10) show moderate concerns, with a small skew towards higher pollution. This also provides that improper medical waste disposal is significantly linked with insufficient training and infrastructure, as the variability in these factors directly impacts the effectiveness of waste segregation practices, ultimately influencing pollution levels.
Multiple Regression Analysis
Unstandardized coefficients (B) represent the size of the impact that each factor has on the outcome, expressed in their original units, while standardized coefficients (β) show the relative importance of variables on a standardized scale. Standard error measures variability, t-value tests significance, and p-value determines if the relationship is statistically significant. Table 6 shows the relationships between variables using regression analysis. Figure 4 shows the outcomes of variables and their SE values.
|
Table 6. Results for Regression Analysis |
||||||
|
Variable |
Unstandardized coefficients (B) |
Standardized coefficients (β) |
SE |
t-value |
p-value |
Significance Level |
|
Healthcare Facility Type |
0,045 |
0,120 |
0,030 |
1,500 |
0,011 |
Significant |
|
Worker Training Level |
-0,210 |
-0,320 |
0,052 |
-4,038 |
0,001 |
Significant |
|
Waste Segregation Practices |
0,480 |
0,510 |
0,056 |
8,571 |
0,001 |
Significant |
|
Infrastructure Quality |
-0,265 |
-0,370 |
0,048 |
-5,521 |
0,000 |
Highly Significant |
|
Pollution Levels |
0,315 |
0,290 |
0,060 |
5,250 |
0,001 |
Significant |
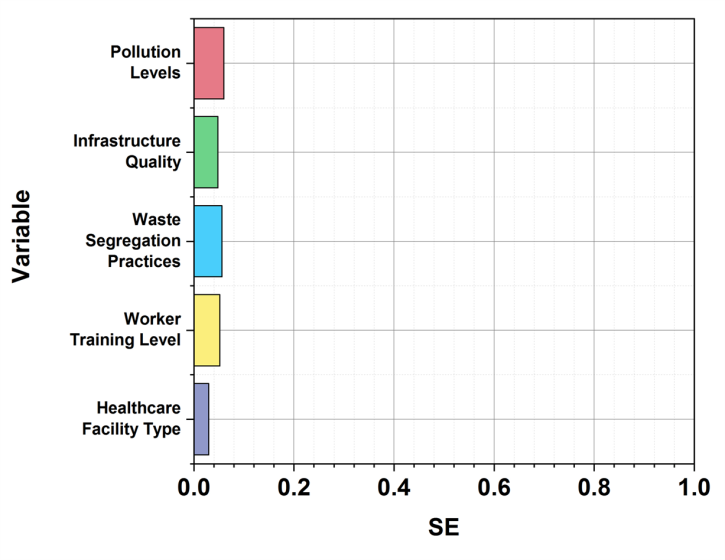
Figure 4. Results for Multiple Regression Analysis
The results demonstrated strong correlations between waste segregation practices and improved environmental health outcomes (B = 0,480). Insufficient worker training (B = -0,210) with poor infrastructure quality (B = -0,265) significantly contributed to improper medical waste disposal. Worker training level and pollution levels showed significant effects, along with waste segregation practices and infrastructure quality. These negative correlations highlight the urgent need for enhanced training programs and infrastructure upgrades. Healthcare facility type showed no significant impact (B = 0,045, p > 0,05). Effective policy reforms are necessary to address these key risk factors.
DISCUSSION
An investigation was conducted to determine the effects of improper medical waste disposal on environmental health. The factors under investigation included the type of healthcare facility, worker training, and the quality of waste management infrastructure. The dataset was gathered through questionnaires targeting 150 health care workers and 50 waste management personnel in various local hospitals and clinics, focusing on the waste disposal practices, trainings offered to the workers, and the quality of infrastructure. Data were gathered from 150 health care workers and 50 waste management personnel, targeting their waste disposal practices and environmental health outcomes. Descriptive statistics and multiple regression analysis on SPSS Version 28 showed significant correlations in disposal practices with environmental outcomes. Inadequate training on the workers' part and inadequate infrastructure have been highlighted as major reasons for improper disposal, and an increased interest in training programs and improved infrastructure is expected. The need for certain policy reforms and enhance improved waste management practices appears to be necessary.
CONCLUSIONS
The influence of improper medical waste disposal on environmental health was accessed in this research. The data were composed of 150 healthcare workers and 50 waste management personnel spread across the local hospitals and clinics. The descriptive statistics revealed improper medical waste disposal is significantly linked with insufficient training and infrastructure, as the variability in these factors directly impacts the effectiveness of waste segregation practices, ultimately influencing pollution levels. Significant correlations were established in multiple regression analysis, where practices in waste segregation correlated positively with environmental health improvements. However, inadequate worker training and infrastructural deficiencies emerged as major factors contributing to inappropriate waste disposal. The type of healthcare facility showed no significant correlation with the outcome; instead, the findings highlight the importance of improved training and infrastructure upgrades. Two significant drawbacks are the specific focus and self-reported information. Expanding the sample size and covering broader regions could enhance the generalizability of future research.
BIBLIOGRAPHIC REFERENCES
1. Zand AD, Heir AV. Emanating challenges in urban and healthcare waste management in Isfahan, Iran after the outbreak of COVID-19. Environmental Technology. 2021 Jan 15; 42(2):329-36. https://doi.org/10.1080/09593330.2020.1866082
2. Joseph B, James J, Kalarikkal N, Thomas S. Recycling of medical plastics. Advanced Industrial and Engineering Polymer Research. 2021 Jul 1;4(3):199-208. https://doi.org/10.1016/j.aiepr.2021.06.003
3. Xiong X, Liu X, Iris KM, Wang L, Zhou J, Sun X, Rinklebe J, Shaheen SM, Ok YS, Lin Z, Tsang DC. Potentially toxic elements in solid waste streams: Fate and management approaches. Environmental pollution. 2019 Oct 1;253:680-707. https://doi.org/10.1016/j.envpol.2019.07.012
4. Iyer M, Tiwari S, Renu K, Pasha MY, Pandit S, Singh B, Raj N, Krothapalli S, Kwak HJ, Balasubramanian V, Jang SB. Environmental survival of SARS-CoV-2–a solid waste perspective. Environmental Research. 2021 Jun 1;197:111015. https://doi.org/10.1016/j.envres.2021.111015
5. Aryampa S, Maheshwari B, Sabiiti EN, Zamorano M. A framework for assessing the ecological sustainability of waste disposal sites (EcoSWaD). Waste Management. 2021 May 1;126:11-20. https://doi.org/10.1016/j.wasman.2021.02.044
6. Alharbi NS, Alhaji JH, Qattan MY. Toward sustainable environmental management of healthcare waste: a holistic perspective. Sustainability. 2021 May 9;13(9):5280. https://doi.org/10.3390/su13095280
7. Qian G, Duanmu C, Ali N, Khan A, Malik S, Yang Y, Bilal M. Hazardous wastes, adverse impacts, and management strategies: a way forward to environmental sustainability. Environment, Development and Sustainability. 2021:1-26. https://doi.org/10.1007/s10668-021-01867-2
8. Yusoff FM, Abdullah AF, Aris AZ, Umi WA. Impacts of COVID-19 on the aquatic environment and implications on aquatic food production. Sustainability. 2021 Oct 13;13(20):11281. https://doi.org/10.3390/su132011281
9. Okedere OB, Olalekan AP, Fakinle BS, Elehinafe FB, Odunlami OA, Sonibare JA. Urban air pollution from the open burning of municipal solid waste. Environmental Quality Management. 2019 Jun;28(4):67-74. https://doi.org/10.1002/tqem.21633
10. Behnam B, Oishi SN, Uddin SM, Rafa N, Nasiruddin SM, Mollah AM, Hongzhi M. Inadequacies in hospital waste and sewerage management in Chattogram, Bangladesh: exploring environmental and occupational health hazards. Sustainability. 2020 Oct 31;12(21):9077. https://doi.org/10.3390/su12219077
11. Zamparas M, Kapsalis VC, Kyriakopoulos GL, Aravossis KG, Kanteraki AE, Vantarakis A, Kalavrouziotis IK. Medical waste management and environmental assessment in the Rio University Hospital, Western Greece. Sustainable Chemistry and Pharmacy. 2019 Sep 1;13:100163. https://doi.org/10.1016/j.scp.2019.100163
12. Aung TS, Luan S, Xu Q. Application of multi-criteria-decision approach for the analysis of medical waste management systems in Myanmar. Journal of Cleaner Production. 2019 Jun 10;222:733-45. https://doi.org/10.1016/j.jclepro.2019.03.049
13. Ilyas S, Srivastava RR, Kim H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Science of the Total Environment. 2020 Dec 20;749:141652. https://doi.org/10.1016/j.scitotenv.2020.141652
14. Hantoko D, Li X, Pariatamby A, Yoshikawa K, Horttanainen M, Yan M. Challenges and practices on waste management and disposal during COVID-19 pandemic. Journal of environmental management. 2021 May 15;286:112140. https://doi.org/10.1016/j.jenvman.2021.112140
15. Rodrigues MO, Abrantes N, Gonçalves FJ, Nogueira H, Marques JC, Gonçalves AM. Impacts of plastic products used in daily life on the environment and human health: What is known?. Environmental toxicology and pharmacology. 2019 Nov 1;72:103239. https://doi.org/10.1016/j.etap.2019.103239
16. Wafula ST, Musiime J, Oporia F. Health care waste management among health workers and associated factors in primary health care facilities in Kampala City, Uganda: a cross-sectional study. BMC public health. 2019 Dec;19:1-0. https://doi.org/10.1186/s12889-019-6528-4
17. Odonkor ST, Mahami T. Healthcare waste management in Ghanaian hospitals: Associated public health and environmental challenges. Waste Management & Research. 2020 Aug;38(8):831-9. https://doi.org/10.1177/0734242X20914748
18. Zhao HL, Wang L, Liu F, Liu HQ, Zhang N, Zhu YW. Energy, environment and economy assessment of medical waste disposal technologies in China. Science of The Total Environment. 2021 Nov 20;796:148964. https://doi.org/10.1016/j.scitotenv.2021.148964
FINANCING
None.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Dillip Kumar Dash, Mohammad Asif, Pooja Varma, Shankar Lal Soni.
Data curation: Dillip Kumar Dash, Mohammad Asif, Pooja Varma, Shankar Lal Soni.
Formal analysis: Dillip Kumar Dash, Mohammad Asif, Pooja Varma, Shankar Lal Soni.
Drafting - original draft: Dillip Kumar Dash, Mohammad Asif, Pooja Varma, Shankar Lal Soni.
Writing - proofreading and editing: Dillip Kumar Dash, Mohammad Asif, Pooja Varma, Shankar Lal Soni.