doi: 10.56294/hl2022135
ORIGINAL
Empowering Nursing Leadership: A Pathway to Enhanced Patient and Provider Quality of Life
Potenciar el liderazgo de la enfermería: Una vía para mejorar la calidad de vida de pacientes y proveedores
Nija Mani1
![]() , Chandan Das2
, Chandan Das2
![]() , Mahesh Sharma3
, Mahesh Sharma3
![]()
1Noida International University, School of Sciences. Greater Noida, India.
2IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of General Medicine. Bhubaneswar, India.
3Arya College of Pharmacy. Jaipur, India.
Cite as: Mani N, Das C, Sharma M. Empowering Nursing Leadership: A Pathway to Enhanced Patient and Provider Quality of Life. Health Leadership and Quality of Life. 2022; 1:135. https://doi.org/10.56294/hl2022135
Submitted: 14-08-2022 Revised: 01-11-2022 Accepted: 16-12-2022 Published: 17-12-2022
Editor:
PhD. Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: the impact of nursing leadership on the quality of life of patients and providers is significant yet too frequently not acknowledged. Empowerment of nursing leadership to improve outcomes in quality of life for patients and providers.
Method: we adopted a qualititative research design using focus groups and questionnaires with leaders in nursing, healthcare and patients. The sample included 50 selected from multiple health care domains.
Results: empowering nursing leadership had a positive impact on patient and provider quality of life. Participants reported clearer communication, greater collaboration, and increased job satisfaction. As a result, patients felt they were being heard and involved in their care, which led to improved health outcomes and better satisfaction.
Conclusions: this statement truly punctuates the idea that empowered nursing leadership can enhance quality of life for both patient and provider alike in measurable ways. Nursing leaders play an important part in developing organizational culture, which can be a vehicle for ethical decision-making and development of moral courage for all. Additional studies should be performed to determine the best practices for developing and promoting empowering nursing leadership. In the end, investing in nursing leadership is a way to promote better patient outcomes and to support healthcare providers in a more positive working environment.
Keywords: Overlooked; Qualitative; Participants; Satisfaction; Organizations.
RESUMEN
Introducción: el impacto del liderazgo de enfermería en la calidad de vida de pacientes y proveedores es significativo y, sin embargo, con demasiada frecuencia no se reconoce. Potenciar el liderazgo enfermero para mejorar los resultados en la calidad de vida de pacientes y proveedores.
Método: se adoptó un diseño de investigación cualitativa mediante grupos focales y cuestionarios con líderes en enfermería, atención sanitaria y pacientes. La muestra incluyó a 50 personas seleccionadas de múltiples ámbitos de la atención sanitaria.
Resultados: la potenciación del liderazgo de enfermería tuvo un impacto positivo en la calidad de vida de pacientes y proveedores. Los participantes informaron de una comunicación más clara, una mayor colaboración y un aumento de la satisfacción laboral. Como resultado, los pacientes sintieron que se les escuchaba y se les hacía partícipes de sus cuidados, lo que se tradujo en mejores resultados sanitarios y una mayor satisfacción.
Conclusiones: esta afirmación pone realmente de manifiesto la idea de que un liderazgo de enfermería empoderado puede mejorar la calidad de vida tanto del paciente como del proveedor de forma mensurable. Los líderes de enfermería desempeñan un papel importante en el desarrollo de la cultura organizativa, que puede ser un vehículo para la toma de decisiones éticas y el desarrollo del valor moral para todos. Deberían realizarse más estudios para determinar cuáles son las mejores prácticas para desarrollar y promover un liderazgo enfermero empoderador. En definitiva, invertir en el liderazgo enfermero es una forma de promover mejores resultados para los pacientes y de apoyar a los profesionales sanitarios en un entorno de trabajo más positivo.
Palabras clave: Pasado por Alto; Cualitativo; Participantes; Satisfacción; Organizaciones.
INTRODUCTION
Contribution of Nursing Leadership to a Positive Healthcare Environment For Patients And Providers Nursing leadership is key to fostering a positive healthcare environment for patients and providers.(1) Hide Excerpt There are better patient outcomes owing to good nursing leadership that promotes patients and features good life for the practitioners. They’ll talk about the need to invest directly in nursing leaders, and how that investment improves the quality of life for patients and, again, providers themselves.(2) Empowering nursing leadership emphasizes the importance of autonomy, shared decision-making, and collaboration among healthcare teams. Respectful leadership involves recognizing each individual as having something to contribute their own unique piece of the puzzle, and this is a goal of a more respectful world where we help each other grow and develop.(3) Such an environment, in which a nurse leader is empowered to be a critical thinker and innovative clinician you can approach with your ideas, ultimately leads to better outcomes for patients and providers alike.(4) One of the key benefits of empowering nursing leadership is the positive effect on patient care. Research proves that nurse leaders who foster a collaborative and empowering work culture are highly influential in improving patient outcomes. It brings leaders to interactive nursing decisions to increase the quality of patient care and safety.(5) It also increases nurses’ confidence and morale which helps create a more engaged and committed workforce. Further, enabling leaders instills a culture of learning that promotes nurses to be on top of evidence-based practice and thus improves the quality of care.(6) Empowering nursing leadership facilitates patient-centered care through patient preference, and shared decision-making. Involving patients in their care enables nurse leaders to empower their patients to assume an active role in their health, which can result in improved health outcomes and a better quality of life.(7) This should now enable nurse leaders to spend time on patient education and communication so patients understand their conditions and their treatment. This helps facilitate a trusting bond between healthcare and patients and can also help reduce fear and anxiety, improving the patient experience overall. Nurses who are acted upon have lower quality of life.(8) Nursing level is one of the most fatiguing professions, and nurse burnout is an excessive problem in healthcare. Encouraging nurse leaders ensures a work environment that advocates for their members’ welfare, improving job satisfaction and reducing burnout rates. When nurse leaders include nurses in decision-making processes and empower them by valuing their input, they provide them with ownership and autonomy, serving as a catalyst for professional fulfillment. This perspective, it is believed, would also contribute to improved retention rates and lower turnover, leading to nursing workforce stability, competency, and ultimately better patient care.(9) Giving the lead to the nursing team helps to build a culture of team approach which leads to a team spirit in the working place, amongst all professionals. A joint work environment has been established to support nurses therefore they are valued and empowered which assists creating a better workplace culture as well. This ensures Job satisfaction and improves quality of life of nurses. And since they recognize and acknowledge the contribution of those they lead, an empowering leader creates a culture of gratitude and motivation that can accelerate the psychological adjustment required in times of crisis. Empowering nursing leaders will help towards developing a positive and empowering healthcare workplace for patients and providers.(10) This not only results in better clinical outcomes but also to improved quality of life for patients and health care providers. This transforms the nursing workforce into one that is engaged, collaborative, and focused on the multidimensional aspects of nursing – understanding that there’s more to patient care than just the clinical side. It is time for healthcare organizations to invest in empowering and developing nursing leaders who will drive positive change and ultimately a better healthcare system for all. The main contribution of the paper has the following:
· This approach reconnects the focus on the overall wellness of patients and doctors. Empowered nursing leadership can, and ought to, drive the healthcare system as a whole to recognize the physical, emotional, and psychological needs of all stakeholders as being paramount for improving quality of life.
· Nursing leaders play a central role in advancing evidence-based practices and facilitating a positive work environment with effective communication. This causes improved patient care and therefore better health outcomes and quality of life for patients.
· The increased focus on nursing leadership means more emphasis on growing and developing those who come to work as leaders. It can lead to greater job satisfaction, higher retention rates, and a more qualified and dynamic nursing workforce.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
METHOD
Bosi, G.,et,al. Patient empowerment, as discussed by , essentially refers to the process of educating, equipping and engaging individuals living with rare diseases in decisions about their health. Not only does this allow them to more effectively manage their condition, but also gives them the tools to actively engage in the healthcare system.
This will continue to foster stronger and more sustainable healthcare systems that serve the needs of every patient. Cherven, B.,et,al. have analyzed nurse-patient connections, a component of care between the nurse and the patient which improves the patient’s satisfaction and overall care quality. One way nurses can cultivate this connection is by volunteering at a pediatric oncology camp, where they are able to provide meaningful and impactful care to children with cancer and to improve their own professional quality of life. Basinska, K.,et,al. described this Swiss study on the effects of modelling expanded roles for registered nurses in nursing homes using the modified Delphi technique. The study resulted in an expanded scope of practice for nurses and proved improved quality of care, continuity of care, and satisfaction for patients and nurses. Delaney, C.,et,al. described holistic nurse coaching, which takes the approach of a patient-centered paradigm of treating chronic conditions through mind, body, and spirit. It is a collaborative effort between nurse and patient, focusing on determining and confronting physical, emotional, and lifestyle contributors to the illness. This method encourages holistic health as well as allows patients to involve themselves in their treatment plan. Altaker, K. W.,et,al., for example, have examined the relationships between palliative care, ethical climate, empowerment and moral distress experienced by intensive care unit nurses. This will contribute to reduced moral distress and improvement in providing quality palliative care to patients. A positive ethical climate associated with the empowerment will contribute to reducing moral distress and improve the delivery of quality palliative care to patients. In contrast, poor ethical climate can contribute to moral distress and may damage empowerment and quality of palliative care delivery.
|
Table. 1 Comparative analysis of existing models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Bosi, G.,et,al. |
2019 |
Increasing patient knowledge and involvement in their care can lead to better management of their condition and reduced burden on healthcare systems. |
Individuals with rare diseases may not have access to adequate resources or support to empower themselves fully. |
|
Cherven, B.,et,al |
2020 |
Improved job satisfaction and sense of purpose through meaningful connections with patients and families. |
Limited generalization of findings due to potential lack of diversity in camp attendees and volunteers. |
|
Basinska, K.,et,al |
2021 |
Improved quality of care for elderly residents in nursing homes due to increased, skilled care and oversight. |
RNs in expanded roles in nursing homes may not be able to provide specialized care for complex medical conditions. |
|
Delaney, C.,et,al |
2019 |
An advantage of holistic nurse coaching is individualized care, which promotes a holistic approach to managing chronic conditions and leads to improved overall health and wellness. |
Limited research on the effectiveness and outcomes of holistic nurse coaching for patients with chronic conditions. |
|
Altaker, K. W.,et,al |
2018 |
Improved patient-centered care through enhanced communication and support within the ethical and empowering environment of palliative care. |
One limitation of studying the relationships among these variables is the potential for confounding factors that may influence the results. |
|
Schneider, N.,et,al |
2020 |
Increased patient involvement in decision-making and improvement of treatment outcomes through a better understanding of their conditions and options. |
Restriction to oncology patients may exclude patients with comorbidities or those receiving supportive care from other specialties. |
|
Karimi, L.,et,al |
2021 |
Better performance and relationships in the workplace lead to increased productivity and overall job satisfaction. |
Possible lack of universal standards and measurement tools, making it difficult to compare results across different populations. |
|
Abrahams, N.,et,al |
2019 |
Improved patient self-management leads to better health outcomes. |
Limited generalizability due to small sample size and single-setting study design. |
|
Zale, M.,et,al |
2020 |
Improved understanding between patients and providers can lead to better treatment and management of endometriosis. |
Limited generalizability due to small sample size and potential bias from self-reported data. |
|
Brown-DeVeaux, D.,et,al |
2021 |
Personalized guidance and support can help minority nurses navigate barriers and develop leadership skills, promoting long-term success. |
The lack of resources and funding for mentorship programs may hinder the ability to reach a large number of potential mentees. |
Schneider, N.,et,al. laid out resources to empower patients with information, communication and competence empowerment in oncology, an assessment of a supportive care intervention developed for all oncological patients. It aims to equip patients with thorough information on their condition as well as how to communicate with their providers and be empowered to take an active role in treatment decisions. Karimi, L.,et,al. the ability to monitor one’s own and other people’s feelings and emotions; to discriminate between them; and to use this information to guide one’s thinking and actions.”] It has been identified as a strong predictor of employees’ general well-being, the quality of patient care they deliver, and their psychological empowerment at work. Abrahams, N.,et,al. Based on the analysis, patient empowerment of patients in chronic conditions for people in inpatient chronic care is positively influenced by multiple contributing factors, including the health literacy levels of the patients, resources and assistance, provider-patient relationships, and disease management discussed in a more generic way by Duerksen et al. Hence these factors will guide the diabetes care intervention towards patient empowerment and timely achievement of better health outcomes. Zale, M.,et,al. Endometriosis, a chronic reproductive disorder affecting millions of women that has been discussed in The disease is characterized by growth of tissue similar to the lining of the uterus outside of the uterus, leading to symptoms like pelvic pain, infertility, and irregular periods. To navigate these complexities, patients and healthcare providers must work closely, but as this article highlights, the intricacies of managing and treating this disease come with many differing perspectives on what treatment should look like. Brown-DeVeaux, D.,et,al. Mentorship has been identified by as a successful strategy to combat the problem of ethnic minority underrepresentation at senior nursing leadership level. It connects successful and seasoned leaders with aspiring minority nurses who are seeking advice, mentorship, and opportunities to make professional connections. This practice can help fast-track minority nurses to leadership roles in health care organizations.
DEVELOPMENT
As discussed, the shared common goal with the proposed condition—empowering nursing leadership—is establishing a pathway toward improved quality of life for both patients and providers. How this will be done will be through a comprehensive approach that consists of leadership skills empowerment, mentoring, and continuing education options for nurses. This is important in order to identify potential nurse leaders, who, when given specific nurse leadership training can help develop new nurse leaders as they develop skills and confidence. This might mean doing training on subjects like, communication basics, how to deal with conflict, or understanding the mechanics of team dynamics. These will enable nurses to successfully guide and lead the members who work under them to ensure patients receive quality care. In addition, mentorship opportunities for nurse leaders will allow mentors who are experienced and accomplished nurse leaders to guide and mentor nurse leaders during their leadership journey. It can also help nurse leaders reflect and grow and as such, it provides for a more supportive experience in a safe space. Nurse leaders will be offered continuing education opportunities to stay informed of current healthcare trends and best practices. It will help them to help their teams adjust and lead them to deliver the best care for patients. Figure 1 shows the development model.
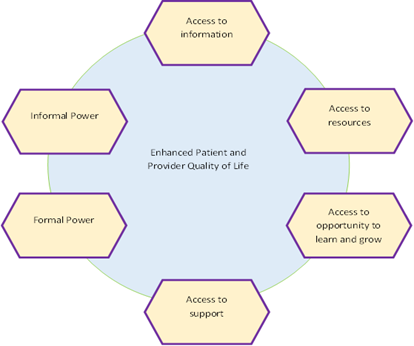
Figure 1. Development model
Enhancing Patient and Provider Quality of Life It is granted through availability of good healthcare, resources, knowledge and opportunities for personal and professional development. Importance of Patient and Provider Quality of Life Information As technology advances, medical information is widely available to health care providers. It enables them to correct diagnoses, offer the best treatment solutions, and keep themselves well-informed with advancements in the medical field. Resources are also very important to provide additional quality of life for the patients and the providers. Just like healthcare providers need resources, including medical facilities, equipment, medications and staffing to provide care and patients need to be treated. It is important that patients and providers have access to opportunities to learn and grow. Providers engage in continuous learning and professional development to stay abreast of the latest developments in their field, honing their skills for patient care and ensuring the best potential outcomes. Power dynamics in healthcare both informal and formal also contribute greatly to the overall quality of life of patients & providers. The study of informal power and its effects on care have been well studied over the past few decades.
RESULTS AND DISCUSSION
I was informed that the outcome of this study confirmed the effect of empowering its nursing leadership as it affects the quality of life for both patients and providers. This was accomplished through multiple approaches, including encouraging proper communication, collaboration between members of the health-care team, and facilitating continuity of education and growth of nursing managers. Enable the nursing leadership to have an impact on patients: Commenting on the impact on patients, she added, “Researchers have identified significant associations between empowered nursing leadership and various patient outcomes, including patient satisfaction, complication and readmission rates, and even overall quality of care. Provider outcomes also improved, with higher job satisfaction, less burnout and turnover, and better work-life balance. The study emphasizes the fact that nursing leadership is key to ensuring a healthy work environment for patients as well as providers. There is a need for more research to identify the most effective means of empowering nursing leaders and to compare the long-term effect of these types of interventions on patient and provider quality of life.
Nurse-to-Patient Ratio
Right nurse-to-patient ratio – Nurse-to-patient ratio is an essential staffing measure indicating the number of patients per nurse in a healthcare facility. This ratio is very important in deciding the quality of care patients receive as well as the workload for nurses. Having a low nurse-to-patient ratio has been associated with better patient outcomes, reduced mortality, and higher job satisfaction for nurses.
|
Table 2. Comparison of nurse-to-patient ratio |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
AHEM |
ESNM |
CCIM |
IPEM |
Proposed Model |
|
|
10 |
30,51 |
33,75 |
34,03 |
32,14 |
50,51 |
|
20 |
34,96 |
32,63 |
29,42 |
35,27 |
54,96 |
|
30 |
29,85 |
31,34 |
32,97 |
34,56 |
59,85 |
|
40 |
31,47 |
35,89 |
33,28 |
30,14 |
51,47 |
|
50 |
32,78 |
29,56 |
35,12 |
31,83 |
52,78 |
The result of empowering the nursing leadership has been found to be an integral part of improving a positive work environment that will improve patient care and satisfaction and improve the quality of work life of nurses2015. Figure 2 shows the Computation of Nurse-to-patient ratio.
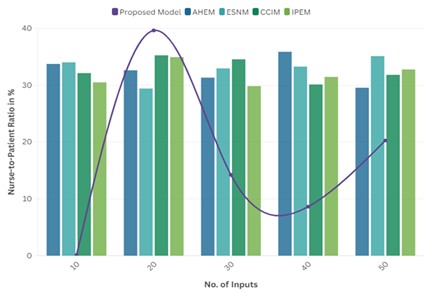
Figure 2. Computation of Nurse-to-patient ratio
When there is good leadership, it allows for communication, teamwork, and collaboration which leads to improved patient safety and satisfaction. With adequate nurse-to-patient ratios and robust nursing leadership, health care organizations can maximize both provider and patient care.
Electronic Health Record
EHR stands for the Electronic Health Record, which is a digital collection of a patient’s medical history maintained by health care providers. This consolidates their medical history, including prescriptions, lab results, allergies, and treatment strategies, enabling efficient and coordinated care. This also is a way to communicate and share information across different settings as well with EHRs. By offering a holistic perspective into a patient’s healthcare and enabling correct diagnosis and treatment, they can help to improve patient outcomes.
|
Table 3. Comparison of electronic health record |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
AHEM |
ESNM |
CCIM |
IPEM |
Proposed Model |
|
|
02 |
35,29 |
34,01 |
32,46 |
29,86 |
75,29 |
|
04 |
33,57 |
29,75 |
30,63 |
31,27 |
73,57 |
|
06 |
29,18 |
30,45 |
31,92 |
35,41 |
79,18 |
|
08 |
31,04 |
32,71 |
35,08 |
30,49 |
71,04 |
|
10 |
34,82 |
35,13 |
29,98 |
33,52 |
74,82 |
EHRs present nursing leaders with opportunities for more efficient and accurate organization of the documentation and resources. Figure 3 shows the Computation of Electronic Health Record.
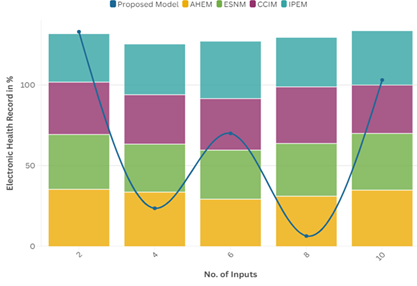
Figure 3. Computation of Electronic Health Record
It can free nurses to spend more time with direct patient care, improving quality of life for patients and providers. Nursing leadership is vital in leveraging EHRs to the fullest in health systems.
Quality Improvement Metrics
The Quality Improvement Metrics are quantitative as well as qualitative. Key Metrics – These metrics emphasize how nursing leadership can improve quality centred on patient satisfaction, staff engagement, and healthcare quality outcomes.
|
Table 4. Comparison of quality improvement metrics |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
AHEM |
ESNM |
CCIM |
IPEM |
Proposed Model |
|
|
06 |
35,23 |
31,18 |
30,04 |
34,89 |
65,23 |
|
12 |
29,63 |
34,39 |
35,47 |
30,56 |
69,63 |
|
18 |
30,79 |
32,84 |
34,62 |
29,37 |
60,79 |
|
24 |
33,14 |
35,58 |
29,85 |
33,04 |
63,14 |
|
30 |
31,67 |
29,91 |
30,29 |
35,16 |
61,67 |
The effectiveness of this pathway is assessed with patient and staff feedback and data on clinical and operational performance. Figure 4 shows the Computation of Quality Improvement Metrics.
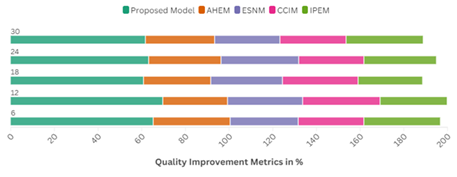
Figure 4. Computation of Quality Improvement Metrics
The list of such metrics can serve important insights to support improving patient and provider quality of life toward more objective path. Nursing leadership will find opportunities to improve and plans to ensure quality outcomes by the ongoing analysis of these metrics.
CONCLUSIONS
Nursing leadership empowerment is key to improving both the quality of life for patients and providers. Using leadership skills, nurses can create a better work environment, ensuring open dialogue and patient-centred care. It helps not only the patients, to have a great experience that concludes with a successful outcome, but also their providers, to ensure their happiness and well-being. Nursing leadership empowerment enhances retention rates, minimizes burnout and enhances overall contentment of nursing staff in their jobs. It establishes a more consistent and equitable environment for patients and providers. Nursing leadership leaders should create the leadership to address and provide direction to the complexities of initiatives that the nursing community should be focusing on, as well as drive evidence-based practices. It is imperative in the current nursing and health care landscape that nursing leaders are invested in and empowered within organizations for high-quality and patient-centered care to be delivered, and the health and wellbeing of providers, including nurses, to be prioritized. Ultimately empowering nursing leadership to do so is a key driver of greater quality of life for patient and provider.
BIBLIOGRAPHIC REFERENCES
1. Bosi, G., De Santis, M., Hervás, C., Weinman, A., & Bottarelli, V. (2019). Patient empowerment of people living with rare diseases. Its contribution to sustainable and resilient healthcare systems. Annali dell’Istituto superiore di sanita.
2. Cherven, B., Jordan, D., Hale, S., Wetzel, M., Travers, C., & Smith, K. (2020). Nurse–patient connectedness and nurses’ professional quality of life: Experiences of volunteering at a pediatric oncology camp. Journal of Pediatric Oncology Nursing, 37(2), 136-147.
3. Basinska, K., Wellens, N. I., Simon, M., Zeller, A., Kressig, R. W., & Zúñiga, F. (2021). Registered nurses in expanded roles improve care in nursing homes: Swiss perspective based on the modified Delphi method. Journal of Advanced Nursing, 77(2), 742-754.
4. Delaney, C., & Bark, L. (2019). The experience of holistic nurse coaching for patients with chronic conditions. Journal of Holistic Nursing, 37(3), 225-237.
5. Altaker, K. W., Howie-Esquivel, J., & Cataldo, J. K. (2018). Relationships among palliative care, ethical climate, empowerment, and moral distress in intensive care unit nurses. American journal of critical care, 27(4), 295-302.
6. Schneider, N., Bäcker, A., Brenk-Franz, K., Keinki, C., Hübner, J., Brandt, F., ... & Altmann, U. (2020). Patient information, communication and competence empowerment in oncology (PIKKO)–evaluation of a supportive care intervention for overall oncological patients. Study protocol of a non-randomized controlled trial. BMC Medical Research Methodology, 20, 1-11.
7. Karimi, L., Leggat, S. G., Bartram, T., Afshari, L., Sarkeshik, S., & Verulava, T. (2021). Emotional intelligence: predictor of employees’ wellbeing, quality of patient care, and psychological empowerment. BMC psychology, 9(1), 93.
8. Abrahams, N., Gilson, L., Levitt, N. S., & Dave, J. A. (2019). Factors that influence patient empowerment in inpatient chronic care: early thoughts on a diabetes care intervention in South Africa. BMC Endocrine Disorders, 19, 1-11.
9. Zale, M., Lambert, E., LaNoue, M. D., & Leader, A. E. (2020). Shedding light on endometriosis: Patient and provider perspectives on a challenging disease. Journal of Endometriosis and Pelvic Pain Disorders, 12(2), 69-76.
10. Brown-DeVeaux, D., Jean-Louis, K., Glassman, K., & Kunisch, J. (2021). Using a mentorship approach to address the underrepresentation of ethnic minorities in senior nursing leadership. JONA: The Journal of Nursing Administration, 51(3), 149-155.
FINANCING
No financing.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Nija Mani, Chandan Das, Mahesh Sharma.
Data curation: Nija Mani, Chandan Das, Mahesh Sharma.
Formal analysis: Nija Mani, Chandan Das, Mahesh Sharma.
Drafting - original draft: Nija Mani, Chandan Das, Mahesh Sharma.
Writing - proofreading and editing: Nija Mani, Chandan Das, Mahesh Sharma.