doi: 10.56294/hl2022131
ORIGINAL
Evaluation of Peer Training Programs for Health Volunteers to Enhance Chronic Disease Management
Evaluación de programas de formación entre iguales para voluntarios sanitarios con el fin de mejorar la gestión de las enfermedades crónicas
Dheeraj
Ghanshyamdas Agrawal1, Syed Fahar Ali2
![]() , Pooja Varma3
, Pooja Varma3 ![]() , Rachita Sarangi4
, Rachita Sarangi4
![]()
1Dr. D.Y.Patil Institute of Technology, Department of Electronics & Telecommunication. Pimpri, India.
2Noida International University, School of journalism and Mass Communication (SJMC). Greater Noida, India.
3JAIN (Deemed-to-be University), Department of Psychology. Bangalore, India.
4IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Paediatrics. Bhubaneswar, India.
Cite as: Agrawal DG, Fahar Ali S, Varma P, Sarangi R. Evaluation of Peer Training Programs for Health Volunteers to Enhance Chronic Disease Management. Health Leadership and Quality of Life. 2022; 1:131. https://doi.org/10.56294/hl2022131
Submitted: 14-08-2022 Revised: 22-10-2022 Accepted: 21-12-2022 Published: 22-12-2022
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Chronic diseases, including hypertension, diabetes, and cardiovascular conditions, were major health concerns among older adults in rural areas. Health Outreach Volunteers (HOVs) were vital in addressing these challenges by providing basic healthcare services. The intention of this research is to develop to and evaluate the effectiveness of a peer-training program in enhancing HOV’s knowledge, self-confidence, and performance in chronic disease management. The training program consisted of an eight-session program, delivered over 4 weeks. A total of 67 health workers participated in twice-weekly sessions, focusing on chronic disease management, health behaviors, and communication strategies. Data were gathered through pre- and post-intervention assessments using the Health Knowledge and Wellness Assessment (HKWA), the Chronic Disease Management Survey (CDMS), and self-efficacy scales. Continued training initiatives should be prioritized to further strengthen the capacity of HOVs in rural well-being settings. Significant improvements were determined in HOVs, HKWA (p=0,001), CDMS (p=0,001), and self-confidence scores (p=0,01). Participants also described an increase in their ability to deliver healthcare services, enhance patient education, and foster superior interaction with healthcare proficient. The peer-led training program proved effective in improving the skills, knowledge, and assurance of HOVs in the supervision of chronic diseases. Continued training invention should be prioritized to further maintain the potential of HOVs in rural health surroundings.
Keywords: Peer Training Programs; Health Volunteers; Chronic Disease; Health Outreach Volunteers (HOVs).
RESUMEN
Las enfermedades crónicas, entre ellas la hipertensión, la diabetes y las afecciones cardiovasculares, eran los principales problemas de salud entre los adultos mayores de las zonas rurales. Los Voluntarios de Promoción de la Salud (VPS) eran vitales para hacer frente a estos problemas mediante la prestación de servicios básicos de atención sanitaria. El objetivo de esta investigación es desarrollar y evaluar la eficacia de un programa de formación entre iguales para mejorar los conocimientos, la autoconfianza y el rendimiento de los HOV en la gestión de enfermedades crónicas. El programa de formación consistió en un programa de ocho sesiones, impartidas a lo largo de 4 semanas. Un total de 67 trabajadores sanitarios participaron en sesiones dos veces por semana, centradas en la gestión de enfermedades crónicas, conductas de salud y estrategias de comunicación. Los datos se recopilaron mediante evaluaciones previas y posteriores a la intervención en las que se utilizaron la Evaluación de Conocimientos de Salud y Bienestar (HKWA, por sus siglas en inglés), la Encuesta de Gestión de Enfermedades Crónicas (CDMS, por sus siglas en inglés) y escalas de autoeficacia. Se debe dar prioridad a las iniciativas de formación continuada para fortalecer aún más la capacidad de los HOV en entornos rurales de bienestar. Se determinaron mejoras significativas en las puntuaciones de los HOV, HKWA (p=0,001), CDMS (p=0,001) y autoconfianza (p=0,01). Los participantes también describieron un aumento de su capacidad para prestar servicios sanitarios, mejorar la educación de los pacientes y fomentar una interacción superior con los profesionales sanitarios. El programa de formación dirigido por compañeros demostró ser eficaz para mejorar las habilidades, los conocimientos y la seguridad de los HOV en la supervisión de enfermedades crónicas. Debe darse prioridad a la formación continuada para mantener el potencial de los HOV en los entornos sanitarios rurales.
Palabras clave: Programas de Formación entre Pares; Voluntarios de Salud; Enfermedades Crónicas; Voluntarios de Promoción de la Salud (HOVs).
INTRODUCTION
A chronic condition is a preventive approach in treating chronic medical conditions like diabetes, hypertension, CVD, and pneumonia. It encompasses patient education, regular monitoring, drug adherence, and planned treatment regimes.(1) Proper supervision requires cooperation between the healthcare professionals, patients, and caregivers to deal with the emotional, physical, and social issues. High tech equipment including telemedicine and digital health software, are brought in to create patient experiences and reduce healthcare system stress.(2) Health volunteers increase the quality of life (QoL) for people with chronic medical conditions by eliminating the physician-patient boundary during treatment. They recommend learning, emotional maintenance, and management adherence, emphasizing early intervention, modification to behavior, and periodic evaluations.(3) This concern not only reduces the strain on the medical manufacturing, but also develops societal support by encouraging individuals to obtain a proactive advance in maintaining their health. The advancements merges with public health targets to enhance accessibility, affordability, and stability of care for individuals with chronic diseases.(4)
Health volunteers encourage valuable consumption of food, exercise, and stress management in the workplace, with the intention of improving overall health and wellness.(5) It entails working with patients to discriminate and encourage long-term behavioral changes that improve productivity, diminish absences, and lower the risk of accidents or sickness. Health coaching supports individuals with chronic or severe health environments to address their illnesses and avoid the rotation of chronic illness and extreme anxiety.(6) It has the prospect to enhance health outcomes, principally for people suffering from CVD and other co-morbid conditions. The efficiency of HOVs in managing chronic diseases can be considerably improved through proper training and capacity-building initiatives. One promising approach is peer-led training programs,(7) which allow individuals with similar cultural and social contexts to become leaders in health education and chronic disease management, especially in resource-limited settings. HOVs are instrumental in bridging the healthcare gap between rural and urban areas,(8) providing essential services like health screenings, medication adherence support, symptom monitoring, and health education. The objective of the research is to estimate the efficiency of a peer-training program in enhancing HOV knowledge, self-confidence, and performance in managing chronic diseases. It aims to assess improvements in key areas such as disease management, health behaviors, and communication strategies.
The organization of the research is listed as follows: Section 2 determines the related work and Section 3 examines the materials and method of the research. Section 4 illustrates the results and discussion of the research. Section 5 describes the conclusion of the research.
Related work
The idea of self-management in healthcare was widely(9) utilized but lacks consensus. It defined qualities in eight phases, which include person-oriented, person-environment-oriented, and summary characteristics. Person-oriented characteristics include active engagement, accountability for difficulties, beneficial psychological techniques, and an openness to social support. Person-environment-oriented characteristics include being knowledgeable about conditions, disease, treatment, and self-management, communicating needs, values, and goals, and cultivating open partnerships with healthcare professionals. Self-management was a lifetime effort that requires personal abilities and encompasses medical, role, and emotional management. Transparency on self-administration can improve understanding and make it easier to undertake chronic illness self-management methods. Health systems have aggressively utilized telecommunication for COVID-19 care and chronic illness management, as determined in the research. However, without assuring equality,(10) inequities in healthcare availability can be compounded for populations at risk such as rural inhabitants, racial/ethnic minorities, older adults, low-income people, and those with insufficient medical comprehension or understanding of English. To avoid exacerbating health disparities, clinicians and health system leaders should investigate possible inequalities in remote healthcare accessibility, devise substances to mitigate technological obstacles, eliminate health system-created constraints to video appearances, and promote laws and facilities that promote equitable telemedicine accessibility.
The COVID-19 epidemic was the largest worldwide problem since World War II, and improving public understanding, attitudes, and practice was critical to managing it. Research(11) was conducted among 404 chronic disease patients at Addis Zemen Hospital in Northwest Ethiopia to analyze their understanding, perspective, and behavior about COVID-19. The findings revealed a substantial amount of inadequate expertise and behavior, at 33,9 % and 47,3 %. Age, educational status, rural domicile, and yearly revenue were all related with low awareness. Poor knowledge, practice, and economic levels were all associated with poor COVID-19 practice, necessitating the use of local language booklets and comprehensive details from health professionals.
According to(12), aging, urbanization, changes in lifestyle, and unequal access to healthcare were all contributing reasons to the global increase in long-term non-communicable diseases (NCDs). Lower-middle-income countries (LMICs) were disproportionately affected, considering 85,90 % of impulsive deaths among people aged 30-69 years. NCDs were associated with substantial levels of illness and death, as well as significant treatment costs. Primary health care (PHC) services were critical for avoiding and managing NCDs, particularly in low- and middle-income countries that have inadequate medical facilities and hospitalization. A comprehensive PHC service approach can be effective in both high- and low-resource environments. The method enabled patients and assists healthcare practitioners in improving patient health at a lesser cost. An investigation(13) involving 54 health-care personnel discovered that a health coaching program aimed at employees with at least one cardiovascular disease risk factor was helpful to encourage healthy lifestyles. 74 % of the participants followed the program, which consisted of six sessions over a 12-week period. The patients had significant rates of obesity, hypertension, diabetes, prediabetes, hyperlipidemia, chronic pain/rehabilitation requirements, depressive disorders, and other multiple conditions. Following the coaching, participants lost substantial weight, improved their exercise, reduced anxiety, and rested better. The research concluded that health instruction for healthcare personnel with obesity and CVD risk factors was a potential way to improving health and well-being.
To analyze the Diamond diabetes monitoring device’s usefulness, credibility, and reliability for maternal patients with diabetes mellitus in Australia, was examined in the research. The gadget(14) was adapted from a design science research standpoint, and an 8-week nonblinded crossovers clinical trial was done across two periods. The findings revealed that ten patients preferred standard care plus the technological solution above conventional therapy in isolation. All physicians believed that the technological solution helped them provide higher-value treatment for patients and was beneficial to analytically observe glucose levels and any change or trends. The investigation indicated that an entire strategy was required to provide value-driven, personalized care in chronic disease management. Chronic diseases assassinate about 12 million people each year in low- and middle-income countries (LMICs), with the total number anticipated to climb if not treated. The investigation(15) emphasized the value of society pharmacists in managing chronic illnesses and the necessity for policymakers to relocate for that capacity. Society pharmacies provided affordable healthcare, although they often cannot be officially recognized as primary care practitioners. As a result, policy changes should encourage individuals to utilize the clinical talents strategically as part of the primary healthcare team in low- and middle-income countries. The purpose of the research(16) was to investigate the probability and suitability of a movable health-based approach that combined traditional community health volunteer programs with electronic devices in rural Nepal. 17 female health professionals effectively monitored the blood pressures of 1113 rural Nepalis, recognized 169 hypertension patients, and gathered health-related data. 70 % of these patients possessed a mobile phone, and 92 % wanted to receive health-related information on it. 84 % favored voice calls, with 7 % and 1 % preferring texts and devices, correspondingly. The findings indicate that a digital healthiness involvement combining characteristic phones and female group of people health volunteers could be a viable and practical strategy to conduct a verification-based curriculum to lower high blood pressure in rural Nepal. According to a meta-analysis of 30 trials, consistent care techniques can minimize hospitalizations in 12,9 % of patients and 21,9 % in the experimental group(17) during an interval of one to three months. Interventions that addressed all continuity dimensions increased the advantages. However, three months later, the effect was uncertain. The investigation demonstrated that longevity of healthcare therapy can minimize temporary hospitalizations in older adults with chronic conditions, but provides insufficient evidence of avoiding permanent recurrence difficulties.
METHOD
This research evaluated the knowledge, skills, and adoption barriers of HOVs after receiving eight sessions of peer training for four weeks. The trainings included chronic disease management, health practices, and communication tactics. The impact of the peer-training program was gauged by using statistical analysis that compared the pre- and post-intervention consequences and measured significant improvements in knowledge, self-efficacy, and performance indicators.
Data collection
The purpose of the peer-training program was to increase knowledge, self-efficacy, and competencies of HOVs in supervising chronic diseases as well as improve healthcare service provision. The study collected data regarding health workers, n=67, who underwent eight peer trainings within a period of time greater than four weeks. Trainings focused on chronic disease care, health behaviour, and communication strategies. Interviews, questionnaires, and observation were used during pre- and post-intervention stages to assess knowledge, skills, and deployment issues. Table 1 and Figure 1 present an extensive suggestion of the participant gender, age, education, and specialized background, highlighting the group’s diverse structure.
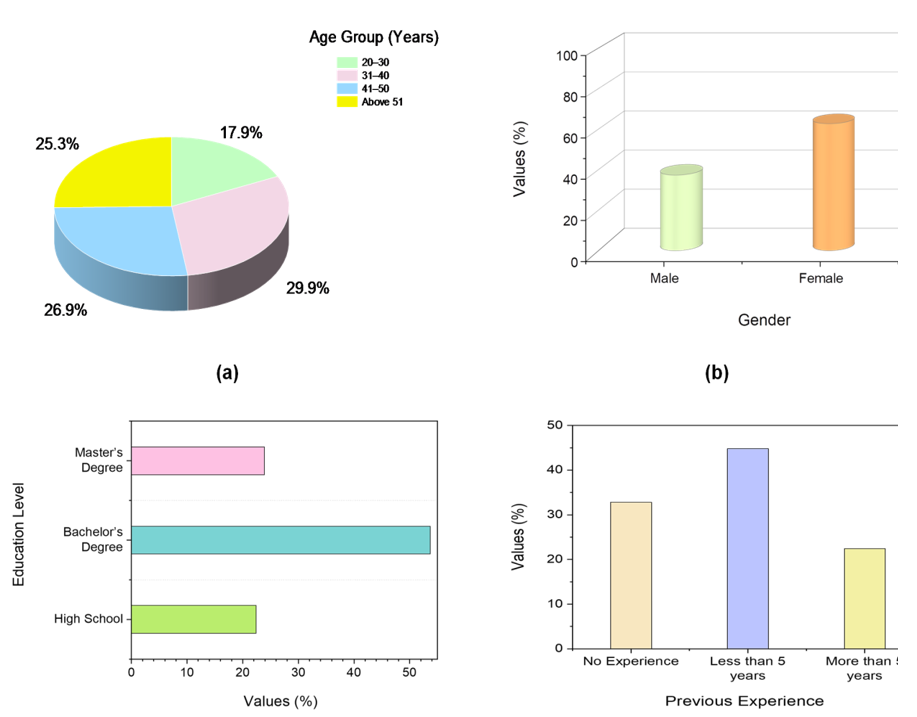
Figure 1. Graphical representations of the demographic variables
|
Table 1. Characteristics of Demographic variables (n=67) |
|||
|
Variable |
Category |
No. |
% |
|
Gender |
Male |
25 |
37,3 |
|
|
Female |
42 |
62,7 |
|
Age Group (Years) |
20–30 |
12 |
17,9 |
|
|
31–40 |
20 |
29,9 |
|
|
41–50 |
18 |
26,9 |
|
|
Above 51 |
17 |
25,3 |
|
Education Level |
High School |
15 |
22,4 |
|
|
Bachelor’s Degree |
36 |
53,7 |
|
|
Master’s Degree |
16 |
23,9 |
|
Previous Experience |
No Experience |
22 |
32,8 |
|
|
Less than 5 years |
30 |
44,8 |
|
|
More than 5 years |
15 |
22,4 |
The following table highlights the demographic characteristics of participants in the peer training program. The majority of the participants (42, 62,7 %) were female, with 25 males (37,3 %). About age, the majority of participants (20, 29,9 %) were between the ages of 31 and 40, followed by those aged 41 to 50 (18, 26,9 %), 51 and up (17, 25,3 %), and 20 to 30 (12, 17,9 %). In terms of education, more than half of the participants (36, 53,7 %) had a Bachelor’s degree, 16 (23,9 %) had a Master’s degree, and 15 (22,4 %) graduated from high school. In terms of past experience in health-related professions, 30 individuals (44,8 %) had fewer than 5 years of experience, 22 (32,8 %) had no prior experience, and 15 (22,4 %) had more than 5 years.
Training Sessions
The Health Outreach Volunteers (HOVs) participated in a four-week peer training program included eight sessions. The training program was intended to advance their comprehension and skills in chronic disease management, such as hypertension, diabetes, and CVD. It covered chronic conditions, promoted healthy behavior, and communicated effectively with patients. Practical essentials were also included, allocate participants to examine patient education strategy, evaluate health risks, and create tailored care plans. Participants who accomplished the training indicated superior abilities to manage chronic conditions, correspond with patients, and collaborate with healthcare expert.
Assessment
The research determined the efficacy of the peer training program by assessing three evaluation scales: the Health Knowledge and Wellness Evaluation (HKWA), the Chronic Disease Management Survey (CDMS), and self-efficacy scores.
HKWA
• The HKWA is apparatus used to assess individuals’ knowledge of critical health issues such as disease avoidance, management, and wellness activities.
• The HKWA is composed of multiple-choice questions that test acquaintance of health habits and well-being approaches. Each question is distributed a score based on whether the health performance is suitable. The total score can reveal an individual’s degree of health sensitivity, with higher values indicative of higher consideration.
CDMS
• The CDMS evaluates participants’ ability to manage chronic disorders like diabetes, hypertension, and CVD.
• The CDMS involves questions about symptom association, medication adherence, medical visits, lifestyle change, and perceived challenges to manipulating the disease, and respondents are graded depending on adhering to recommended procedures.
Self-efficacy scores
• Self-efficacy scales were utilized to evaluate participants’ confidence in their abilities to provide proficient healthcare services, enhance patient learning, and foster qualified relations.
• The self-efficacy established employs questions with Likert scales to evaluate things based on an individual’s response, with higher scores representing superior self-efficacy. For example, a 4 out of 5 on health condition assurance recommends superior self-efficacy.
These scores provided a complete assessment of the training program’s effect on participants’ understanding, abilities, and trust in chronic disease management.
Statistical Analysis
For this statistical analysis, SPSS software has been used for the conduct of statistical tests. The operational statistical test used were Independent T-test, Interquartile Range (IQR), and Friedman Test. Independent T-test was used to analyze the participants’ scores on their health knowledge pre-and post-training, HKWA, and determine whether significant modification existed following the peer-training program. IQR were set up to measure the variability in CDMS scores, establishing data allocation and alteration reliability before and after training. The Friedman Test is used to compare self-efficacy values before and after the sessions of training, determining whether there was significant change in participants’ self-confidence in chronic disease management.
RESULTS
Health Knowledge and Wellness Assessment (HKWA)
HKWA utilizes an Independent T-test to evaluate pre and post-intervention values to measure the participants’ initial value understanding as well as the enhancement made as the outcome of the program. The independent t-test consequences in table 2 show considerable improvement in a variety of health knowledge and awareness ratings post an intervention. Each variable assessment indicates a range of aspects of health knowledge, and the findings indicate that participants’ scores increased statistically, significant between pre and post-intervention.
|
Table 2. Results for HKWA Scores |
|||||
|
Variable |
Pre-Intervention Mean (SD) |
Post-Intervention Mean (SD) |
t-value |
p-value |
Effect Size (Cohen’s d) |
|
Nutrition Knowledge Score |
6,8 (1,2) |
8,5 (1,0) |
7,32 |
0,001 |
1,58 |
|
Physical Activity Knowledge |
7,0 (1,3) |
8,8 (0,9) |
8,45 |
0,001 |
1,75 |
|
Disease Prevention Awareness |
6,5 (1,1) |
8,2 (0,8) |
8,12 |
0,001 |
1,70 |
|
Stress Management Techniques Awareness |
6,9 (1,4) |
8,7 (0,9) |
7,95 |
0,001 |
1,63 |
|
Health Literacy Level |
7,2 (1,5) |
8,9 (1,1) |
7,80 |
0,001 |
1,56 |
Nutrition Knowledge Score
The pre-intervention mean score was 6,8 (SD = 1,2), which increased to 8,5 (SD = 1,0) post-intervention. The t-value of 7,32 and a p-value of 0,001 indicate a highly significant difference, with an effect size of 1,58, suggesting a large effect of the intervention on nutrition knowledge. Physical Activity Knowledge: Participants had a pre-intervention mean score of 7,0 (SD = 1,3), which rise to 8,8 (SD = 0,9) after the intervention. The t-value of 8,45 and p-value of 0,001 also reflect a significant improvement, with a large effect size of 1,75. Disease Prevention Awareness, indicates the mean value of 6,5 (SD = 1,1) pre-intervention to 8,2 (SD = 0,8) post-intervention. The t-value of 8,12 and p-value of 0,001 indicate a considerable change, with an effect size of 1,70, suggesting a strong impact of the intervention on disease prevention responsiveness. Stress Management Techniques Awareness: The pre-intervention mean 6,9 (SD = 1,4), which improved to 8,7 (SD = 0,9) post-intervention. The t-value of 7,95 and p-value of 0,001 show a significant difference, with a production size of 1,63, indicating a considerable effect of the intervention on stress management awareness. The overall health literacy level mean score increased from 7,2 (SD = 1,5) to 8,9 (SD = 1,1) post-intervention. The t-value of 7,80 and p-value of 0,001 substantiate a significant development, with an effect size of 1,56, indicating a large effect of the intervention on health literacy. The involvement considerably enlarged participants’ health knowledge and conception across an assortment of illness-related areas, as shown by considerable advantages and high impact sizes in the independent t-test findings.
Chronic Disease Management Survey (CDMS)
CDMS is an apparatus intended to evaluate various aspect of chronic disease management among HOVs. It integrates factor like management observance, patient monitoring, and the operation of evidence-based actions, and data is estimated in the Inter quartile Range (IQR) to represent a variety of values. It evaluate critical apparatus that contribute to effective management of chronic conditions such as hypertension, diabetes, and CVD. The estimation focus on five key areas: Medication Adherence, Symptom Monitoring, Appointment Attendance, Dietary Compliance, and Physical Activity Engagement. Table 3 shows the CDMS component outcomes.
|
Table 3. Numerical Findings of CDMS Component |
|||
|
CDMS Component |
Pre-Training Mean Score |
Post-Training Mean Score |
P value |
|
Medication Adherence |
65 % |
85 % |
< 0,001 |
|
Symptom Monitoring |
55 % |
80 % |
< 0,001 |
|
Appointment Attendance |
70 % |
90 % |
< 0,001 |
|
Dietary Compliance |
60 % |
82 % |
< 0,001 |
|
Physical Activity Engagement |
50 % |
75 % |
< 0,001 |
In the consideration of the peer-training program, the findings from the CDMS emphasized considerable improvement in each of these areas following the training intervention. The mean score for Medication Adherence inflated from 65 % pre-training to 85 % post-training, indicating an extensive development in the participant capability to allow prescribed medication schedule. Similarly, Symptom Monitoring depicts an increase from 55 % to 80 %, reflecting superior reliability in tracking chronic disease symptoms. Appointment Attendance also superior considerably, increasing from 70 % to 90 %, which suggests that HOVs became more attentive in attending scheduled medical visits. Dietary Compliance and Physical Activity Engagement showed gains as well, with achieve growing from 60 % to 82 % and from 50 % to 75 %, respectively. All improvements were statistically considerable, with P-values is less than 0,001, underscoring the efficiency of the training program in enhancing the skills and confidence of HOVs in association with chronic diseases. These results highlight the significance of continued training initiative to further support the capacity of HOVs in rural health setting.
Friedman Test
The Friedman Test was used to investigate variations in optimism ratings across various aspects of the training program. To compare the improvement in scores of the participants before and after sessions of training utilizing the Friedman Test for Self-efficacy Scales. The test estimates whether there are significant distinction in the attainment of the five subscales of self-efficacy, Table 4 represents the confidence in disease management, goal setting ability, problem-solving skills, resilience to setbacks, and social support utilization.
|
Table 4. Evaluation of Friedman findings for Self-Efficacy Scales |
||||
|
Self-Efficacy Scale |
Pre-Training Median |
Post-Training Median |
Z-Statistic |
P value |
|
Confidence in Disease Management |
3,00 |
4,00 |
-5,678 |
0,000 |
|
Goal Setting Ability |
3,50 |
4,50 |
-4,920 |
|
|
Problem-Solving Skills |
3,00 |
4,00 |
-5,432 |
|
|
Resilience to Setbacks |
3,50 |
4,50 |
-5,123 |
|
|
Social Support Utilization |
3,00 |
4,00 |
-5,234 |
|
The Friedman Test was conducted on the self-efficacy scales of health workers before and after the peer training program. The Confidence in Disease Management scale showed a significant increase in median scores from 3,00 (pre-training) to 4,00 (post-training), with a Z-statistic of -5,678 indicating a substantial improvement. Similarly, Goal Setting Ability improved from a median of 3,50 to 4,50 (Z = -4,920), and Problem-Solving Skills increased from 3,00 to 4,00 (Z = -5,432). Resilience to Setbacks also demonstrated significant improvement, with a median increase from 3,50 to 4,50 (Z = -5,123). Finally, Social Support Utilization showed a similar positive change, with the median rising from 3,00 to 4,00 (Z = -5,234). These results highlight the effectiveness of the training program in enhancing the self-efficacy of health workers across all measured dimensions. All improvement were statistically considerable, with P-values less than 0,000. The Friedman Test was applied to evaluate changes in self-efficacy subscales pre- and post-training. Significant improvements were found in all five scales with all P-values being less than 0,05 (P = 0,01). It signifies that the peer-training program efficiently enhanced participants’ assurance in management chronic illness, surroundings health-related goal, solve problems, active back from delay, and utilizing social support.
Discussion
The intention of the research appeared to determine the effectiveness of a peer-training program superior to the knowledge, self-confidence, and performance of HOVs in chronic illness management, specifically hypertension, and CVD. The pre- and post-interventions results clearly show that the training had a considerable influence on HOVs’ ability to efficiently supervise chronic diseases and progress their overall health literacy. The HKWA training program greatly enlarged participants’ determination of the issues, which are associated with health such as physical exercise, disease anticipation, and stress management. The curriculum greatly boosted health literacy among HOVs, providing them with critical knowledge to effectively educate and help clients in managing chronic conditions. The CDMS data revealed significant advances in key components of chronic illness supervision, such as medication adherence, symptom monitoring, appointment, provisions observance, and physical activity participation. The program enhanced its participants’ capability to control chronic diseases, emphasizing the necessity of ongoing education for HOVs in developing patient care and commitment in rural settings with limited healthcare access. The Friedman Test results, a peer-training program significantly increased the self-efficacy of health and social work volunteers in five subscales.
CONCLUSION
The research established that a peer-training program significantly improved the knowledge, self-efficacy, and assessment of HOVs in the care of chronic conditions including diabetes mellitus, hypertension, and CVD. Health literacy for chronic illness management skills as well as self-efficacy went up following training, as demonstrated by considerable increases on the HKWA, CDMS, and Self-Efficacy Scales. It ensured the effectiveness of peer-led training in providing the HOVs with the equipment that they need for the management of chronic diseases while educating patients for the effective service delivery. This study pointed to the importance of continued peer-training activities as essential elements in improving HOVs’ skills in the handling of chronic disease issues in the rural areas. Besides, it suggested the significance of professional development as well as longitudinal research for fine-tuning service provision.
Limitations and Future Scope
These research limitations include being set in a rural environment, possible bias within the self-efficacy measure, and future research should involve looking at retention of knowledge and health outcome for peer training programs, both of which utilize digital tools remotely.
REFERENCES
1. Mirsky JB, Horn DM. Chronic disease management in the COVID-19 era. Am J Manag Care. 2020 Aug 1;26(8):329-30.
2. Klimeš F, Voskrebenzev A, Gutberlet M, Kern AL, Behrendt L, Grimm R, Suhling H, Crisosto CG, Kaireit TF, Pöhler GH, Glandorf J. 3D phase‐resolved functional lung ventilation MR imaging in healthy volunteers and patients with chronic pulmonary disease. Magnetic Resonance in Medicine. 2021 Feb;85(2):912-25. https://doi.org/10.1002/mrm.28482
3. Ding H, Chen Y, Yu M, Zhong J, Hu R, Chen X, Wang C, Xie K, Eggleston K. The effects of chronic disease management in primary health care: Evidence from rural China. Journal of Health Economics. 2021 Dec 1;80:102539. https://doi.org/10.1016/j.jhealeco.2021.102539
4. Lazarus G, Findyartini A, Putera AM, Gamalliel N, Nugraha D, Adli I, Phowira J, Azzahra L, Ariffandi B, Widyahening IS. Willingness to volunteer and readiness to practice of undergraduate medical students during the COVID-19 pandemic: a cross-sectional survey in Indonesia. BMC Medical Education. 2021 Dec;21:1-2.
5. Pascucci D, Sassano M, Nurchis MC, Cicconi M, Acampora A, Park D, Morano C, Damiani G. Impact of interprofessional collaboration on chronic disease management: findings from a systematic review of clinical trial and meta-analysis. Health Policy. 2021 Feb 1;125(2):191-202. https://doi.org/10.1016/j.healthpol.2020.12.006
6. BohingamuMudiyanselage S, Stevens J, Watts JJ, Toscano J, Kotowicz MA, Steinfort CL, Bell J, Byrnes J, Bruce S, Carter S, Hunter C. Personalised telehealth intervention for chronic disease management: a pilot randomised controlled trial. Journal of telemedicine and telecare. 2019 Jul;25(6):343-52. https://doi.org/10.1177/1357633X18775850
7. Berihun G, Walle Z, Berhanu L, Teshome D. Acceptance of COVID-19 vaccine and determinant factors among patients with chronic disease visiting Dessie Comprehensive Specialized Hospital, Northeastern Ethiopia. Patient preference and adherence. 2021 Aug 17:1795-805.
8. Mazzucca S, Arredondo EM, Hoelscher DM, Haire-Joshu D, Tabak RG, Kumanyika SK, Brownson RC. Expanding implementation research to prevent chronic diseases in community settings. Annual review of public health. 2021 Apr 1;42(1):135-58.
9. Van de Velde D, De Zutter F, Satink T, Costa U, Janquart S, Senn D, De Vriendt P. Delineating the concept of self-management in chronic conditions: a concept analysis. BMJ open. 2019 Jul 1;9(7):e027775. https://doi.org/10.1136/bmjopen-2018-027775
10. Chen L, Baird A, Straub D. Fostering participant health knowledge and attitudes: an econometric study of a chronic disease-focused online health community. Journal of Management Information Systems. 2019 Jan 2;36(1):194-229. https://doi.org/10.1080/07421222.2018.1550547
11. Akalu Y, Ayelign B, Molla MD. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen Hospital, Northwest Ethiopia. Infection and drug resistance. 2020 Jun 24:1949-60. https://doi.org/10.2147/IDR.S258736
12. Haque M, Islam T, Rahman NA, McKimm J, Abdullah A, Dhingra S. Strengthening primary health-care services to help prevent and control long-term (chronic) non-communicable diseases in low-and middle-income countries. Risk management and healthcare policy. 2020 May 18:409-26. https://doi.org/10.2147/RMHP.S239074
13. Edman JS, Galantino ML, Hutchinson J, Greeson JM. Health coaching for healthcare employees with chronic disease: a pilot study. Work. 2019 Jan 1;63(1):49-56. https://doi.org/10.3233/WOR-192907
14. Wickramasinghe N, John B, George J, Vogel D. Achieving value-based care in chronic disease management: intervention study. JMIR diabetes. 2019 May 3;4(2):e10368. https://doi.org/10.2196/10368
15. Okoro RN, Nduaguba SO. Community pharmacists on the frontline in the chronic disease management: The need for primary healthcare policy reforms in low- and middle-income countries. Exploratory Research in Clinical and Social Pharmacy. 2021 Jun 1;2:100011. https://doi.org/10.1016/j.rcsop.2021.100011
16. Ni Z, Atluri N, Shaw RJ, Tan J, Khan K, Merk H, Ge Y, Shrestha S, Shrestha A, Vasudevan L, Karmacharya B. Evaluating the feasibility and acceptability of a Mobile health–based female community health volunteer program for hypertension control in rural Nepal: cross-sectional study. JMIR mHealth and uHealth. 2020 Mar 9;8(3):e15419. https://doi.org/10.2196/15419
17. Facchinetti G, D’Angelo D, Piredda M, Petitti T, Matarese M, Oliveti A, De Marinis MG. Continuity of care interventions for preventing hospital readmission of older people with chronic diseases: A meta-analysis. International journal of nursing studies. 2020 Jan 1;101:103396. http://dx.doi.org/10.1016/j.ijnurstu.2019.103396
FINANCING
None.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Data curation: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Formal analysis: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Research: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Methodology: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Project management: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Resources: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Software: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Supervision: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Validation: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Display: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Drafting - original draft: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.
Writing - proofreading and editing: Dheeraj Ghanshyamdas Agrawal, Syed Fahar Ali, Pooja Varma, Rachita Sarangi.