doi: 10.56294/hl2022124
ORIGINAL
Exploring the Impact of Patient Quality of Life on Family Caregiver Burden in Palliative Care
Explorando el Impacto de la Calidad de Vida del Paciente en la Carga del Cuidador Familiar en Cuidados Paliativos
Mahesh Sharma1 ![]() , Pallavi Prakash Chandra2
, Pallavi Prakash Chandra2 ![]() , Debasmita Rath3
, Debasmita Rath3 ![]()
1Arya College of Pharmacy, Jaipur, India.
2Noida International University, School of Allied Health Sciences. Greater Noida, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Paediatrics. Bhubaneswar, India.
Cite as: Sharma M, Chandra PP, Rath D. Exploring the Impact of Patient Quality of Life on Family Caregiver Burden in Palliative Care. Health Leadership and Quality of Life. 2022; 1:124. https://doi.org/10.56294/hl2022124
Submitted: 10-08-2022 Revised: 28-10-2022 Accepted: 14-12-2022 Published: 15-12-2022
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Palliative Care (PA) significantly focuses on family caregivers, and it’s critical to comprehend the interdependencies among patients, family caregivers, and service providers. Since there aren’t many long-term studies that look at how patient Quality of Life (QoL) in PC affects family Caregiver Burden (CB), this research aims to investigate the connection between family CB and patient QoL in PC settings. PC is intended to help patients with severe diseases, but it frequently puts a heavy financial, emotional, and physical burden on family caregivers. 200 data (100 patients, 100 caregivers) were gathered from caregivers of patients receiving PC in a variety of hospital settings using established measures for assessing CB and QoL. The obtained data will be statistically analyzed to determine the association between patient QoL and CB utilizing multiple regression (MR) analysis and Spearman’s rank correlation (SRC). The results show that the caregiver’s perceived burden is greatly increased by low patient QoL, especially when it comes to physical and emotional health. The findings underscore the need for interventions that take into account the psychological and physical burden on caregivers in addition to the needs of patients. Research improves the knowledge of family caregiver interactions in PC and offers solutions to reduce caregiver stress, including resources to improve patient QoL, psychological support, and respite care.
Keywords: Patient QoL (QoL); psychological Support; Caregiver Burden; Palliative Care.
RESUMEN
Los cuidados paliativos (CP) se centran significativamente en los cuidadores familiares, y es fundamental comprender las interdependencias entre pacientes, cuidadores familiares y proveedores de servicios. Dado que no hay muchos estudios a largo plazo que analicen cómo la calidad de vida (CdV) del paciente en CP afecta a la carga del cuidador familiar (CCF), esta investigación pretende investigar la conexión entre la CCF familiar y la CdV del paciente en entornos de CP. La CP está pensada para ayudar a pacientes con enfermedades graves, pero con frecuencia supone una pesada carga económica, emocional y física para los cuidadores familiares. Se recopilaron 200 datos (100 pacientes, 100 cuidadores) de cuidadores de pacientes que reciben CP en diversos entornos hospitalarios utilizando medidas establecidas para evaluar la CB y la CdV. Los datos obtenidos se analizarán estadísticamente para determinar la asociación entre la CdV del paciente y el CB utilizando análisis de regresión múltiple (RM) y correlación de rangos de Spearman (CRS). Los resultados muestran que la carga percibida por el cuidador aumenta en gran medida por la baja calidad de vida del paciente, especialmente en lo que respecta a la salud física y emocional. Los resultados subrayan la necesidad de intervenciones que tengan en cuenta la carga psicológica y física de los cuidadores, además de las necesidades de los pacientes. La investigación mejora el conocimiento de las interacciones de los cuidadores familiares en la CP y ofrece soluciones para reducir el estrés de los cuidadores, incluyendo recursos para mejorar la CdV del paciente, apoyo psicológico y cuidados de respiro.
Palabras clave: QoL del Paciente (QoL); Apoyo Psicológico; Carga Del Cuidador; Palliativecare.
INTRODUCTION
Palliative care (PC) plays a vital role in improving the Quality of Life (QoL) for individuals living with life-limiting medical conditions.(1) The Cancer Treatment Humanity extends traditional medical practices by delivering emotional assistance and implementing alternative ways to care for people facing illness and requires partnership from closest caregivers to provide complete wellbeing solutions.(2) Support services from beginning to end of the illness experience become essential due to the fundamental role played by family caregivers in this model. Fortunately, such caregivers encounter significant challenges as overcome mental and physical barriers while delivering care.(3) The burden of caregiving can jeopardize their own well-being on both sides, complicating their caregiving tasks. The direct link between the stress experienced by caregivers and the quality of care they can provide highlights the importance of supporting these individuals.(4) The extensive physical and emotional demands weaken caregivers’ capacity to handle sophisticated care responsibilities, which results in burnout. Patients and their caregivers need QoL assessments to fully understand how their health status affects both comfort levels and caregiver burdens.(5) Healthcare professionals can utilize these assessments to recognize early caregiver burden so they can provide effective interventions, which reduce stress while enhancing patient and caregiver results.(6) The essential relationship between patient quality of life and caregiver load currently receives minimal attention from healthcare leaders. To solve this, it is critical to incorporate caregiver issues into medical training.(7) Educating healthcare personnel on caregiver stress, psychological strain, and the importance of offering assistance can help improve caring practices.(8) The physical and mental protection of caregivers requires reliable access to proper training and resources and significant occupational health practices. By expanding palliative care services to include full support for caregivers from the family, healthcare institutions might encourage a more humane and successful strategy for end-of-life care.(9) Emphasizing environmental health, mental well-being, and providing robust healthcare management support will lead to improved caregiving experiences, better patient outcomes, and a healthier, more sustainable caregiving environment. The objective of the research is to examine the connection between family CB and patient QoL in PC settings, emphasizing the need for interventions addressing caregiver stress and patient QoL.
The structure of the research
Part 2 presented the related work, the research methodology is developed in Part 3, the performance evaluations are displayed in Part 4 and the conclusion is illustrated in Part 5.
Related work
Research examined the association among caregivers’ stress and QoL in patients receiving PC, highlighting a negative association between the CB and the overall QoL as assessed by the World Health Organization.(10) The findings suggest the importance of regularly evaluating the specific needs of caregivers. Another research examining QoL and CB among family caregivers of cancer patients undergoing treatment revealed that 70,22 % of caregivers reported mild to moderate burden, while 21,38 % endured severe to extreme anxiety. Research showed no significant variation in burden ratings or QoL among male and female adults, and no substantial difference in QoL scores, comparing the two groups.(11) The findings underscore the enormous challenges that caregivers endure in cancer care. The research investigated risk factors associated with caring for advanced cancer patients, assessed actions, and proposed a CARES structure for PC.(12) Results show significant improvements in depression enhancement, but the QoL and care outcomes were mixed. More trials were required to validate, determine and test real-world actions. The purpose of the research was to determine the variables that affect primary caretakers’ enjoyment of life while their patients have progressing, life-threatening illnesses.(13) The QoL of caregivers was impacted by social, psycho-emotional, monetary, and physical variables, according to the results. Guardians’ QoL was enhanced by communication, optimism, illness knowledge, and family engagement. The investigation discovered that the caregivers of seriously ill people with cancer have higher objective, CB, QOL, and sad feelings more prevalent in the greatest two stages.(14) Research employed multidimensional linear modeling with hierarchies to determine the connection between five different types of subjective unpleasantness and function deterioration. The data reveal that persons’ five unique symptom-functional states were substantially and variously related to their providers’ caring burden and QoL over the past six months. It was discovered that cancer patients with family caregivers had low levels of resiliency, which has been linked to greater caregiver burden and lower QoL.(15) Resilience reduced caregiver stress while improving QoL, emphasizing resilience’s both immediate and secondary impact on happiness in life. An investigation discovered that family caregivers of advanced cancer patients feel significant discomfort and depressed symptoms, highlighting the need for psychological support.(16) Female gender, spouse/partner status, tiredness, and poor PC results all raised the chance of moderate to severe anxiety and depression symptoms. Research examined the connections with Spiritual Well-Being (SWB), burden as a caregiver, and QoL among cancer patients’ family caregivers.(17) The findings show that more SWB caregivers experienced better quality of life and less stress, indicating that healthcare providers should pay more attention to spiritual resources for family cancer care during the cancer experience.(18) Research in Sweden discovered that 32 % of relatives of oesophageal cancer survivors reported high or moderate CB, with younger caregivers becoming more likely to experience it. This burden was connected to higher depression, anxiety, and signs of post-traumatic stress disorder and diminished health-related QoL.
METHOD
Patients were included based on specific criteria: the research included patients who received PC treatment specifically for advanced cancer when the expected life expectancy was less than six months. They should have no other conditions associated with a shorter life time expectation and must be receiving outpatient care. Both patients and family caregivers needed to be adults (at least 18 years old) with sufficient proficiency in the local language to comprehend the provided data and complete the required questionnaires. All participants needed to provide consent by both understanding the procedure and signing documents before joining. This included patients, caregivers, and healthcare providers. A systematic participant selection process was implemented, ensuring adherence to specific criteria to gather meaningful insights into the impact of patient QoL on caregiver burden while upholding ethical research standards.
Data Collection
The healthcare providers involved with this research engaged qualified patients and family caregivers before requesting their consent to join the research. The data collection span lasted during a determined time frame. A total of 200 data (100 patients, 100 caregivers) were gathered from caregivers of patients receiving PC in a variety of hospital settings, using established measures for assessing CB and QoL. Participating patients received questionnaires every month following their inclusion to complete the EORTC QLQ-C30 and CB measure. Data was collected over a six-month follow-up period, ensuring confidentiality through pseudonymized identification numbers for patients and caregivers, which also facilitated accurate data matching. Access to personal information was restricted for clinical staff, and all responses remained anonymous to healthcare providers, prioritizing privacy and safeguarding participant identity. Table 1 presents the demographic information about patients and caregivers to demonstrate fundamental variables, like aging, gender, marital status, work status, health status, smoking behavior, and physical exercise levels. Such variables simultaneously affect patient QoL together with CB within PC environments. The research results will clarify how different demographic data points affect caregiver stress and mental state as well as adaptive ability through identified interventions beneficial for patients and their caretakers.
|
Table 1. Demographic values for the patient and caregivers |
|||
|
Variable |
Data (N=200) |
Patients (N=100) |
Caregivers (N=100) |
|
Age (Mean ± SD) |
55,6 ± 10,2 |
58,1 ± 9,8 |
53,1 ± 10,5 |
|
Gender |
|||
|
Male (%) |
120 (60 %) |
45 (45 %) |
75 (75 %) |
|
Female (%) |
80 (40 %) |
55 (55 %) |
25 (25 %) |
|
Marital Status |
|||
|
Married (%) |
140 (70 %) |
85 (85 %) |
55 (55 %) |
|
Single (%) |
40 (20 %) |
10 (10 %) |
30 (30 %) |
|
Divorced/Widowed (%) |
20 (10 %) |
5 (5 %) |
15 (15 %) |
|
Employment Status |
|||
|
Employed (%) |
90 (45 %) |
60 (60 %) |
30 (30 %) |
|
Unemployed (%) |
110 (55 %) |
40 (40 %) |
70 (70 %) |
|
Health Condition |
|||
|
Chronic Illness (%) |
130 (65 %) |
90 (90 %) |
40 (40 %) |
|
No Chronic Illness (%) |
70 (35 %) |
10 (10 %) |
60 (60 %) |
|
Smoking Status |
|||
|
Current Smoker (%) |
50 (25 %) |
30 (30 %) |
20 (20 %) |
|
Former Smoker (%) |
30 (15 %) |
15 (15 %) |
15 (15 %) |
|
Non-Smoker (%) |
120 (60 %) |
55 (55 %) |
65 (65 %) |
|
Physical Activity |
|||
|
Active (%) |
100 (50 %) |
40 (40 %) |
60 (60 %) |
|
Inactive (%) |
100 (50 %) |
60 (60 %) |
40 (40 %) |
Statistical Analysis
The IBM SPSS version 27 focuses on examining the association among patient QoL and CB in PC. The research uses three methods including Spearman’s rank correlation (SRC) and multiple regression (MR), Chi-square (x2) tests, and regression analysis for complete understanding. The strength and direction of correlations between continuous variables like physical health anxiety and depression with CB are observed through the SRC method. The impact of multiple factors on caregiver stress becomes measurable using MR analysis when considering both patient mental health and resilience levels. The (x2) test reveals associations between categorical variables that include factors like smoking status, physical activity levels and CB measurements. Results are presented with statistical significance (p-values), regression coefficients, and confidence intervals (95 %) to ensure robust conclusions. A combination of research methods delivers an extensive understanding of how patient health patterns affect caregiving burdens so clinicians can create specific PC interventions.
RESULTS
The analysis examines the connection between CB and QoL within PC settings. Data from 200 participants, comprising 100 patients and 100 caregivers, were assessed using validated instruments. SRC, MR analysis, and the (x2) test were employed to inspect the effects of physical, psychological, and emotional wellness upon stress among caregivers. The research shows how patient health status affects CB burden and helps direct programs for caregiver support efforts.
EORTC QLQ-C30 Scores to Analyze Patient QoL Trends and Insights
Table 2 presents scores from the EORTC QLQ-C30 dimensions across three-time points (t1, t2, and t3), analyzing patient-reported outcomes on QoL. Variables such as overall QoL, physical functioning, emotional functioning, fatigue, and symptoms like pain, insomnia, and appetite loss are evaluated using median values and interquartile ranges. P-values indicate the statistical significance of changes over time, with notable trends (e.g., decreased physical functioning, p < .01). This table aligns with the research by quantifying patient health dynamics, providing critical insights into how changes in QoL and symptom burden impact caregiver stress, resilience, and perceived burden. The figure consists of three scatterplots comparing different health dimensions (e.g., QoL, fatigue, pain) across three-time points: t1 (Time 1, blue), t2 (Time 2, green), and t3 (Time 3, red). Each plot highlights variations in these dimensions over time, suggesting trends in patient-reported outcomes.
|
Table 2. EORTC QLQ-C30 scores across dimensions and time points |
|||||
|
EORTC QLQ-C30 Dimension |
Number |
t1 |
t2 |
t3 |
p* |
|
Overall QoL |
56 |
40,0 (20,0-70,0) |
35,0 (15,0-65,0) |
55,0 (20,0-75,0) |
,06 |
|
Physical functioning |
53 |
40,0 (10,0-80,0) |
30,0 (5,0-60,0) |
25,0 (0,0-80,0) |
<,01 |
|
Emotional functioning |
56 |
60,0 (45,0-75,0) |
55,0 (30,0-70,0) |
45,0 (15,0-65,0) |
,35 |
|
Dyspnoea |
54 |
25,0 (0,0-60,0) |
30,0 (0,0-70,0) |
35,0 (0,0-80,0) |
,42 |
|
Pain |
57 |
70,0 (25,0-85,0) |
60,0 (20,0-80,0) |
65,0 (30,0-90,0) |
,18 |
|
Insomnia |
57 |
40,0 (10,0-70,0) |
35,0 (0,0-65,0) |
45,0 (10,0-70,0) |
,29 |
|
Fatigue |
56 |
75,0 (50,0-95,0) |
70,0 (45,0-90,0) |
80,0 (50,0-100,0) |
,12 |
|
Appetite loss |
57 |
45,0 (20,0-75,0) |
40,0 (10,0-70,0) |
50,0 (10,0-85,0) |
,08 |
|
Nausea/vomiting |
53 |
20,0 (10,0-60,0) |
25,0 (0,0-60,0) |
30,0 (0,0-70,0) |
,47 |
|
Constipation |
52 |
40,0 (10,0-55,0) |
35,0 (0,0-60,0) |
45,0 (0,0-70,0) |
,21 |
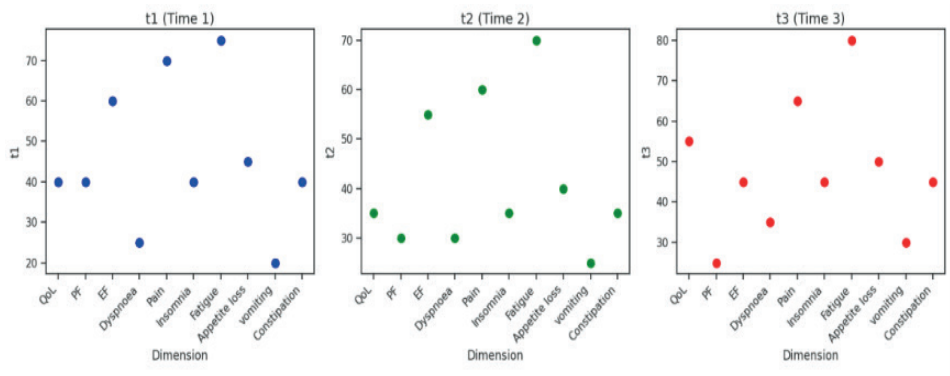
Figure 1. Changes in health dimensions across three-time points
The heatmap visualizes figure 2 and presents an SRC matrix, showing the strength and direction of relationships between variables like anxiety, depression, fatigue, physical QoL, mental health, resilience, Post-Traumatic Growth (PTG), and CB. In the context of the research, it illustrates how patient QoL (physical and mental health) correlates with CB, highlighting significant links such as high CB with fatigue and poor patient QoL. This supports the research’s findings on caregiver stress and the need for targeted interventions.
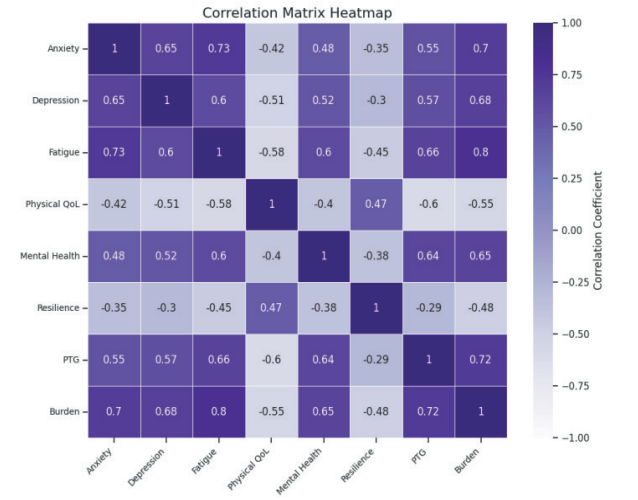
Figure 2. SRC between patient QoL and CB
Table 3 provides the findings of various statistical analyses that examine this connection between various psychological and health-related variables (e.g., anxiety, depression, fatigue, physical and mental health, resilience, post-traumatic growth (PTG), burden, social support, and sleep quality) and the outcomes in the research. The regression coefficients (β) show the strength and direction of these relationships, and Standard Error (SE) while the standardized coefficients indicate the relative importance of each variable. The p-values highlight statistically significant variables (p < 0,05), which are critical for understanding how these factors contribute to QoL and CB, providing insights for potential interventions in PC settings.
|
Table 3. MR analysis results for psychological and health variables |
|||||
|
Variable |
β |
SE |
Confidence Interval (95 %) |
Standardized Coefficient (β) |
p-value |
|
Anxiety |
0,32 |
0,05 |
[0,22, 0,42] |
0,45 |
<0,001 |
|
Depression |
0,21 |
0,04 |
[0,13, 0,29] |
0,30 |
<0,001 |
|
Fatigue |
-0,15 |
0,03 |
[-0,21, -0,09] |
-0,25 |
<0,001 |
|
Physical QoL |
0,18 |
0,06 |
[0,06, 0,30] |
0,22 |
0,003 |
|
Mental Health |
0,14 |
0,05 |
[0,04, 0,24] |
0,19 |
0,005 |
|
Resilience |
0,09 |
0,04 |
[0,01, 0,17] |
0,13 |
0,02 |
|
PTG |
0,23 |
0,05 |
[0,13, 0,33] |
0,31 |
<0,001 |
|
Burden |
0,10 |
0,04 |
[0,02, 0,18] |
0,14 |
0,01 |
|
Social Support |
0,12 |
0,05 |
[0,02, 0,22] |
0,16 |
0,02 |
|
Sleep Quality |
-0,08 |
0,03 |
[-0,14, -0,02] |
-0,12 |
0,008 |
Table 4 presents the outcomes of a (x2) test investigating the link among experienced and anticipated in occurrences across various health dimensions in the research sample. Each variable, such as overall QoL, physical functioning, and emotional effectiveness, is measured for potential differences. The (x2), degrees of freedom (df), and p-value indicate the statistical significance of these differences. About the research, this analysis helps to identify whether variations in health dimensions (e.g., QoL, fatigue) are significantly associated with participant characteristics, offering insights into the psychological and health factors influencing CB.
|
Table 4. (x2) Analysis of health dimensions across research variables |
|||||
|
Variable |
Observed (O) |
Expected (E) |
(χ²) |
df |
p-Value |
|
Overall QoL |
120 |
110 |
2,36 |
2 |
0,31 |
|
Physical Functioning |
130 |
120 |
3,33 |
2 |
0,19 |
|
Emotional Functioning |
115 |
105 |
3,81 |
2 |
0,15 |
|
Dyspnoea |
125 |
118 |
2,07 |
2 |
0,36 |
|
Pain |
140 |
130 |
4,13 |
2 |
0,13 |
|
Insomnia |
110 |
105 |
1,22 |
2 |
0,54 |
|
Fatigue |
135 |
125 |
4,20 |
2 |
0,12 |
|
Appetite Loss |
100 |
95 |
1,32 |
2 |
0,52 |
|
Nausea/Vomiting |
90 |
88 |
0,22 |
2 |
0,89 |
|
Constipation |
105 |
100 |
0,72 |
2 |
0,70 |
DISCUSSION
The relationship between health dimensions, including anxiety, depression, fatigue, physical and mental health, resilience, PTG, and CB among patients and caregivers in PC. According to statistical results based on MR and () testing, various health elements demonstrated considerable interconnections; depressive disorders have a significant impact on quality of life, as does caregiver stress. The research confirmed that improving patient resilience and post-traumatic growth levels creates better distress mitigation outcomes for both patients and their caregivers. Notably, fatigue, physical QoL, and mental health were important predictors of overall well-being, with caregivers reporting a noticeable burden. The data expose the need for specific intervention approaches to support caregivers physically and emotionally, which reduces their stress and enhances PC results.
CONCLUSION
The relationship between health dimensions, with anxiety, depression, fatigue, and QoL, in both patients and caregivers within PC settings. Important relations were found between psychological factors such as resilience and PTG and improved well-being for both groups. Main health outcomes exhibited by caregiver’s revealed fatigue and psychological well-being act as significant factors causing substantial health strain. Research findings emphasize that complete intervention of physical and emotional health needs strengthens both caregiver well-being and patient treatment results in PC. The use of data supplied by participants involves the possibility of bias, and a cross-sectional approach limits the capacity to make connections between variables. The resulting research groups do not accurately represent every individual within PC settings. Future research requires longitudinal design methods alongside enhanced sample sizes, combined with objective health metrics to reach wider adoption and confirm causal connections across diverse settings.
REFERENCES
1. Franchini L, Ercolani G, Ostan R, Raccichini M, Samolsky-Dekel A, Malerba MB, Melis A, Varani S, Pannuti R. Caregivers in home PC: gender, psychological aspects, and patient’s functional status as main predictors for their QoL. Supportive care in cancer. 2020 Jul;28(7):3227-35. https://doi.org/10.1007/s00520-019-05155-8
2. Wu LF, Lin C, Hung YC, Chang LF, Ho CL, Pan HH. Effectiveness of palliative care consultation service on caregiver burden over time between terminally ill cancer and non-cancer family caregivers. Supportive Care in Cancer. 2020 Dec;28:6045-55. https://doi.org/10.1017/S1478951521000213
3. Bužgová R, Kozáková R, Bar M. The effect of neuroPC on QoL and satisfaction with the quality of care in patients with progressive neurological disease and their family caregivers: interventional control research. BMC PC. 2020 Dec;19:1-0. https://doi.org/10.1186/s12904-020-00651-9
4. Vigna PM, de Castro I, Fumis RR. Spirituality alleviates the burden on family members caring for patients receiving PC exclusively. BMC PC. 2020 Dec;19:1-8. https://doi.org/10.1186/s12904-020-00585-2
5. Semere W, Althouse AD, Rosland AM, White D, Arnold R, Chu E, Smith TJ, Schenker Y. Poor patient health is associated with higher CB for older adults with advanced cancer. Journal of Geriatric Oncology. 2021 Jun 1;12(5):771-8. https://doi.org/10.1016/j.jgo.2021.01.002
6. Ahmad Zubaidi ZS, Ariffin F, Oun CT, Katiman D. CB among informal caregivers in the largest specialized PC unit in Malaysia: a cross-sectional research. BMC PC. 2020 Dec;19:1-5. https://doi.org/10.1186/s12904-020-00691-1
7. Alsirafy SA, Nagy R, Hassan AD, Fawzy R, Abdelhafeez AA, Husein MO, Almashiakhi MA, Alabdullateef SH, Alghamdi SA, Elyamany AM. CB among family caregivers of incurable cancer patients in two eastern Mediterranean countries. BMC PC. 2021 Dec;20:1-8. https://doi.org/10.1007/s00520-019-04947-2
8. Kizza IB, Muliira JK. Determinants of QoL among family caregivers of adult cancer patients in a resource-limited setting. Supportive Care in Cancer. 2020 Mar;28:1295-304. https://doi.org/10.1007/s00520-019-04970-3
9. Duimering A, Turner J, Chu K, Huang F, Severin D, Ghosh S, Yee D, Wiebe E, Usmani N, Gabos Z, Patel S. Informal caregiver QoL in a palliative oncology population. Supportive Care in Cancer. 2020 Apr;28:1695-702. https://doi.org/10.1017/S1478951518001025
10. Tang Y. CB and bereavement among family caregivers who lost terminally ill cancer patients. Palliative & Supportive Care. 2019 Oct;17(5):515-22. https://doi.org/10.1080/15524256.2021.1888844
11. Cengiz Z, Turan M, Olmaz D, Erce Ç. Care burden and QoL in family caregivers of PC patients. Journal of Social Work in End-of-Life &PC. 2021 Jan 2;17(1):50-63. https://doi.org/10.4103/IJPC.IJPC_180_20
12. Mishra S, Gulia A, Satapathy S, Gogia A, Sharma A, Bhatnagar S. CB and QoL among family caregivers of cancer patients on chemotherapy: A prospective observational research. Indian Journal of PC. 2021 Jan;27(1):109. https://doi.org/10.1200/JCO.19.00018
13. Alam S, Hannon B, Zimmermann C. PC for family caregivers. Journal of Clinical Oncology. 2020 Mar 20;38(9):926-36. https://doi.org/10.1089/jpm.2021.0322
14. Norinder M, Årestedt K, Lind S, Axelsson L, Grande G, Ewing G, Holm M, Öhlén J, Benkel I, Alvarez A. Higher levels of unmet support needs in spouses are associated with poorer QoL–a descriptive cross-sectional research in the context of palliative home care. BMC PC. 2021 Dec;20:1-1.https://doi.org/10.1016/j.jpainsymman.2018.09.009
15. Wen FH, Chen JS, Chou WC, Chang WC, Shen WC, Hsieh CH, Tang ST. Family caregivers’ subjective caregiving burden, QoL, and depressive symptoms are associated with terminally ill cancer patients’ distinct patterns of conjoint symptom distress and functional impairment in their last six months of life. Journal of pain and symptom management. 2019 Jan 1;57(1):64-72. https://doi.org/10.1016/j.ejon.2020.101832
16. Oechsle K, Ullrich A, Marx G, Benze G, Heine J, Dickel LM, Zhang Y, Wowretzko F, Wendt KN, Nauck F, Bokemeyer C. Psychological burden in family caregivers of patients with advanced cancer at initiation of specialist inpatient PC. BMC PC. 2019 Dec;18:1-4. https://doi.org/10.1186/s12904-019-0469-7
17. Spatuzzi R, Giulietti MV, Ricciuti M, Merico F, Fabbietti P, Raucci L, Bilancia D, Cormio C, Vespa A. Exploring the associations between spiritual well-being, burden, and QoL in family caregivers of cancer patients. Palliative & Supportive Care. 2019 Jun;17(3):294-9.https://doi.org/10.1017/S1478951518000160
18. Pereira-Morales AJ, Valencia LE, Rojas L. Impact of the caregiver burden on the effectiveness of a home-based palliative care program: A mediation analysis. Palliative & supportive care. 2020 Jun;18(3):332-8. https://doi.org/10.1080/0284186X.2022.2119098
FINANCING
None.
CONFLICTS OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Data curation: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Formal analysis: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Research: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Methodology: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Resources: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Software: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Supervision: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Validation: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Visualization: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Original drafting and editing: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.
Writing - proofreading and editing: Mahesh Sharma, Pallavi Prakash Chandra, Debasmita Rath.