doi: 10.56294/hl2022114
ORIGINAL
Assessing the Impact of Telemedicine on Healthcare Management and Delivery in Rural Areas
Evaluación del impacto de la telemedicina en la gestión y prestación de asistencia sanitaria en zonas rurales
Lulup
Kumar Sahoo1 ![]() ,
Fazil Hasan2
,
Fazil Hasan2 ![]() ,
RenukaJyothi S3
,
RenukaJyothi S3 ![]()
1Siksha ‘O’ Anusandhan (Deemed to be University), Department of Neurology, IMS and SUM Hospital. Bhubaneswar, India.
2Noida International University, Department of Agriculture. Greater Noida, India.
3JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, India.
Cite as: Sahoo LK, Hasan F, RenukaJyothi S. Assessing the Impact of Telemedicine on Healthcare Management and Delivery in Rural Areas. Health Leadership and Quality of Life. 2022; 1:114. https://doi.org/10.56294/hl2022114
Submitted: 09-08-2022 Revised: 29-10-2022 Accepted: 19-12-2022 Published: 20-12-2022
Editor:
PhD. Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: telemedicine is increasingly used to provide health care in rural areas. It also highlights on telemedicine being the solution for the management and delivery of healthcare in such regions.
Methods: this is a literature review for obtaining data pertaining to the use of telemedicine in managing and delivering healthcare in rural locations. To gain first-hand perspectives, the researchers interviewed healthcare professionals and telemedicine providers as well.
Results: this study demonstrates the impact of telemedicine in providing greater access to health service in rural areas, especially in remote and underserved areas. It has also overall improved the healthcare management by DHHS in terms of communication and coordination between healthcare providers leading to a reduction in costs and increase in efficiency.
Conclusions: to conclude, this study shows that telemedicine has a major and a positive influence on healthcare management and delivery in area. It can help solve the dissonance of disadvantaged people not being able to get proper healthcare services and potentially bettering the overall healthcare system. Yet, expansion is dependent upon resources and training surrounding this adaptation system.
Keywords: Technology; Communication; Healthcare Professionals; Healthcare Management.
RESUMEN
Introducción: la telemedicina se utiliza cada vez más para prestar asistencia sanitaria en zonas rurales. También se hace hincapié en que la telemedicina es la solución para la gestión y prestación de asistencia sanitaria en dichas regiones.
Método: se trata de una revisión bibliográfica para obtener datos sobre el uso de la telemedicina en la gestión y prestación de asistencia sanitaria en zonas rurales. Para obtener perspectivas de primera mano, los investigadores entrevistaron también a profesionales sanitarios y proveedores de telemedicina.
Resultados: este estudio demuestra el impacto de la telemedicina a la hora de proporcionar un mayor acceso a los servicios sanitarios en las zonas rurales, especialmente en las remotas y desatendidas. También ha mejorado globalmente la gestión de la asistencia sanitaria por parte del DHHS en términos de comunicación y coordinación entre los proveedores de asistencia sanitaria, lo que se ha traducido en una reducción de los costes y un aumento de la eficiencia.
Conclusiones: para concluir, este estudio demuestra que la telemedicina tiene una influencia importante y positiva en la gestión y prestación de asistencia sanitaria en la zona. Puede ayudar a resolver la disonancia que supone que las personas desfavorecidas no puedan recibir servicios sanitarios adecuados y mejorarpotencialmente el sistema sanitario en general. Sin embargo, su expansión depende de los recursos y la formación que rodeen a este sistema de adaptación.
Palabras clave: Tecnología; Comunicación; Profesionales Sanitarios; Gestión Sanitaria.
INTRODUCTION
It is especially important for rural populations who have historically had more difficulty than any other cohort in gaining access to leading care delivery systems.(1) This essay investigates the effect of telemedicine on healthcare administration and delivery in rural areas, highlighting its benefits, challenges, and future outlook. Advantages of Telemedicine In Rural Areas – One of the advantages of telemedicine in rural areas is enhanced access to healthcare services. It mainly affected the areas where the healthcare facilities and healthcare professionals are scarce.(2) Telemedicine allows patients in remote areas to consult with physicians to receive diagnoses and treatment for minor ailments without the need for travel and at a lower cost, bridging the gaps caused by distance and lack of healthcare staff. Having easier access to healthcare services can result in positive health outcomes such as patients getting timely treatment for their acute and chronic conditions.(3)
Telemedicine is a technology and telecommunication-enabled care delivery service. It enables a hopeful change in the health care device by resolving problems associated with geographical limitations, profession supply and call increase. Telemedicine has the ability to reduce healthcare costs in rural communities, in fact.(4) Patients save in terms of money and time travelling (which can be lengthy and expensive) to attend these services. That can also reduce the need for infrastructure — and staffing — all of which can be costly in remote areas. According to a study performed by the American Telemedicine Association, the U.S. healthcare system could save more than $6 billion every year in travel, hospital readmissions, and redundant ER visits using telemedicine services.(5) The influences of telemedicine in rural-oriented healthcare management are also positive. Healthcare providers can remotely access patient information and collaborate with other providers, enhancing care coordination, which reduces medical mistakes. It allows for better use of resources, with healthcare workers able to attend to and treat far more patients from afar.(6)
Filling gaps in doctors and nurses in rural areas. Telemedicine in Rural Areas: challenges Learn more about the challenges posed by telemedicine in rural areas While telemedicine vs in rural areas has potential, we also face challenges.(7) One of the main challenges over there is any access to technology. Telemedicine services rest upon a stable internet connection. In addition, many rural people may not have the necessary technology, such as a smartphone or desktop computers, to attend telemedicine visits. This gap may pose a barrier to access telemedicine services in these communities. Acceptability of new technologies and Resistance to Change is another challenge. Patients as well as healthcare providers in rural areas may be reluctant to adopt telemedicine as per their routine healthcare delivery practice.(8) That might be because of concerns about the quality of care or privacy and security, or simply the lack of in-person interaction with healthcare providers.(9) This will likely require education and training programs that can facilitate the development of trust and familiarity with telemedicine for patients and healthcare professionals alike in these communities.(10)
The main contribution of the paper has the following
• Telemedicine has played a pivotal role in making healthcare services accessible to the population residing in remote areas. Patients no longer need to seek medical treatment at clinics far away and, as such, can be a pain point for remote locations with limited transport capabilities. As a result, medical specialists are more readily available, chronic conditions are better managed, and overall health outcomes are improving in rural communities.
• Additionally, telemedicine has contributed to the cost savings of the healthcare facilities in rural areas. By telemedicine patients can consult with online medical personnel through the internet or video telephone call that saving the traveling and reduces the cost. This is particularly helpful for people who do not have the financial means to travel for medical treatment and who cannot afford to pay medical costs.
• Rural regions are also benefitting from telemedicine for management and delivery of healthcare. This improves communication among patients and healthcare professionals, streamlining medical records and data and facilitating better coordination among a variety of health care providers. As a result, healthcare services are delivered more efficiently and effectively, which ultimately leads to improved health outcomes for individuals in rural communities.
Chen, J., Amaize, A., et al. Among others, have debated the assessment for telehealth adoption and barriers among hospitals in urban and rural settings. This will include an analysis of how telehealth technology is used to provide healthcare services and the challenges hospitals face with implementing and using this technology. This is important as telehealth services can be utilized in both rural and urban environments to create more accessible and effective healthcare capabilities. Harkey, L. C., et al. The authors have analyzed this systematic review that examined the existing data on patient satisfaction with telehealth services in rural areas. In general, these findings suggest strong patient satisfaction with telehealth due to greater accommodation to care accessibility, convenience, and cost savings. However, several limitations like technical issues and absence of physical involvement were highlighted. Kiberu, V. M., et,al. Assessment of health provider readiness for telemedicine services in Uganda was also explored by, which involves the evaluation of preparedness of health provider, capability and resources of health provider to implement telemedicine. This involves evaluating their technological framework, training and proficiency with telemedicine, and organizational encouragement for this model. It also identifies any potential challenges and barriers to successful implementation. Gillespie, S. M., et,al. have addressed standards applicable to telemedicine in evaluating and treating deterioration in nursing home residents. These standards are based on state regulations and facility policies. As a rule, they demand adequate staff training, informed consent from both the resident and their family, and adherence to privacy and security protocols regarding telehealth services. Muzammil, S et al. have been talking about Telehealth (also known as telemedicine), the use of communication technology to provide medical services remotely. Though it started out as a tool to give healthcare access to rural people, it’s now used to give care to every person seeking care -- and especially valuable during a crisis like the current COVID-19 pandemic.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Chen, J., Amaize, A., & Barath, D |
2021 |
Improved understanding of disparities and strategies needed to address them, leading to equitable access to healthcare for all. |
Lack of generalizability due to the small sample size and potential regional variations in telehealth adoption and barriers. |
|
Harkey, L. C., Jung, S. M., Newton, E. R., & Patterson, A |
2020 |
Improved access to healthcare for rural patients who may not have easy access to traditional in-person appointments. |
Limited access to reliable internet connection and technology in rural areas can skew results and exclude specific populations. |
|
Kiberu, V. M., Scott, R. E., & Mars, M. |
2019 |
Increased efficiency and accessibility of healthcare services for patients in remote or underserved areas. |
Lack of access to reliable technology and infrastructure in certain regions may affect the accuracy of provider readiness assessments. |
|
Gillespie, S. M., |
2019 |
Improved efficiency and timeliness in monitoring and addressing changes in resident health status. |
Possible limitation: Lack of infrastructure and technical support in the nursing home for effective implementation of telemedicine. |
|
Muzammil, S. |
2020 |
One advantage of Telehealth is its ability to provide access to medical care in remote or underserved areas. |
One limitation of Tele-Health is its current focus on providing access to healthcare in rural areas, neglecting its potential for widespread use in other areas. |
|
Mars, M. |
2019 |
Increasing accessibility and availability of healthcare services to underserved populations in remote areas. |
One limitation is that it may not accurately capture the true extent of the providers’ readiness or willingness to adopt telemedicine services. |
|
Chu, C., Cram, P., |
2021 |
Improved access to healthcare in rural areas, especially during a pandemic. |
The study does not account for differences in access to technology and internet connectivity in rural areas. |
|
Mullen-Fortino, M., |
2019 |
Saving time and expense associated with traveling to a physical location for assessment. |
Limited accuracy and reliability of diagnostic tests and assessments due to lack of physical interaction with the patient. |
|
Niznik, J. D., |
2018 |
Improved access to medication management and education for patients in remote or underserved areas. |
Possible lack of patient-provider face-to-face interaction may impede the establishment of a strong therapeutic alliance and may hinder medication adherence. |
|
Ruiz de Adana, M. S., |
2020 |
Objective and unbiased comparison of outcomes between telemedicine and standard care groups. |
Potential lack of generalizability to other regions/populations with different health care systems or access to telemedicine services. |
Mars, M et al. Assessing the readiness of health providers for telemedicine services in Uganda. These are their technological infrastructure, knowledge and skills, attitude and willingness to adopt telemedicine, and regulatory framework. This may assist in identifying the barriers and challenges that must be addressed in order to implement telemedicine services in UgandaChu, C., et al. The study looks at the prevalence of telemedicine in rural areas, before and during the COVID-19 pandemic. This uses a repeated cross-sectional design, examining data from numerous time points to assess changes in the use of telemedicine. The purpose of the study is to examine the effect of the pandemic on health care access in rural communities. Mullen-Fortino, M., et al. that enables telemedicine technology between virtual consultation and remote monitoring of the presurgical assessment by health care providers. This minimizes the need for physical visits, allowing for improved efficiency and effectiveness. Patients receive care with added comfort and convenience: They stay in their own home. Niznik, J. D., et,al. have discussed. In conclusion, the systematic review supports that clinical pharmacist services via telemedicine in the outpatient or ambulatory care setting positively affect patient outcomes, medication adherence, and overall healthcare costs. These services also increase access to specialized pharmaceutical care and help to alleviate the shortage of pharmacists in rural or underserved areas. Ruiz de Adana, M. S., et,al. To our knowledge, the only other study conducted to evaluate the effects of telemedicine care in patients with type 1 diabetes with suboptimal glycemic control is the PLATEDIAN study in Spain, an ongoing research project in Andalusia, Spain. Results from this multifaceted, randomized study will further elucidate if telemedicine interventions can yield improved outcomes for these patients.
METHOD
It has become increasingly important to evaluate the influence of telemedicine on management and delivery of rural healthcare. For instance, telemedicine (the remote delivery of health services using telecommunications technology). Since at the same time it has the possibility to overcome the gap of health access between rural and urban. The first step in the development process would be to conduct a comprehensive assessment of the current state of healthcare management and delivery in rural areas, focusing on the challenges and limitations faced by healthcare providers and patients. It used to provide a baseline for comparison. Then do a survey or focus group discussions among rural healthcare providers and patients to get their perceptions of telemedicine and its potential role. And it could help identify fears or concerns they have about using technology for health care. The framework can then used to evaluate the effect of telemedicine on several domains including accessibility, quality of care, cost-effectiveness, and patient satisfaction, based on the data collected. The evaluation could be done through analysis of data from the implementation of telemedicine programs in selected rural communities. Interviews, surveys, and data analysis of patient outcomes and healthcare utilization rates before and after the implementation of telemedicine could be included in this. The evaluation’s results may eventually be utilized to make reform-related suggestions and approaches for incorporating telemedicine into rural healthcare structures, This would help health care providers in implementing telemedicine technology to better management and delivery of health care in rural areas. Single physician or nursing level cannot take care of all patients. Figure 1 shows the development model.
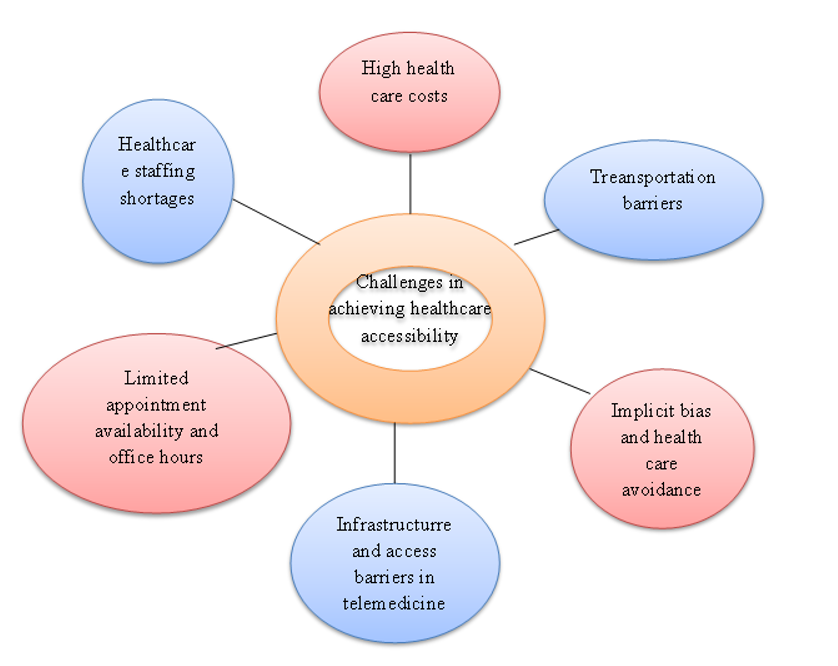
Figure 1. Development model
Healthcare staffing shortages are when there aren’t enough healthcare workers — like nurses, doctors and specialists — at a particular healthcare facility. They leave in droves due to high burnout, low wages and a lack of training opportunities, which is pretty similar across the board, blog after blog. This means it will be harder for these providers to have enough appointments and office hours to accommodate rising service demand. This leads to delayed care and possible poor outcomes for patients. Factors Social determinants of health in telemedicine Infrastructure and access barriers For some, and maybe even many, especially those dwelling within rural or remote regions, a stable internet connection may not be available. For example, implicit bias and healthcare avoidance can contribute to healthcare disparities in marginalized populations, wherein groups may be wary of seeking medical attention due to past negative experiences which made them feel it was not in their best interest to seek medical attention. Transportation barriers may also limit access to care for some individuals. For those who are less mobile (e.g. elderly or disabled), people with no access to public transportation, or are living in rural areas where healthcare is limited, this can be even more of a challenge. These hurdles could result in missed appointments, or delayed care, both of which affect overall health fate. High healthcare costs drive hundreds of thousands of people into medical bankruptcy, and millions lack access to necessary healthcare services.
RESULTS AND DISCUSSION
A review demonstrated several positive outcomes for the existing healthcare system regarding the effectiveness of telemedicine in relation to healthcare management and delivery in rural areas. These advantages have included, among other things, access to healthcare services, quality of care, and patient and provider cost savings. In this study, one of the most experimental findings was the efficiency of telemedicine for delivering health services to rural areas that lack health due to the absence of health centers and lack of health staff. Specialized care and consultation by specialists in telemedicine system was not far off for patients. Furthermore, it ensured telemedicine, which improved the efficiency and quality of care by enabling healthcare providers to obtain patient data readily from remote locations, collaborate with other specialists in real time, among others. This allowed for faster, more accurate diagnosis and treatment, leading to better patient health outcomes. Telemedicine also eased economic pressure on patients and the providers. Patients were spared those travel and lodging expenses; health care providers eliminated costs for maintaining physical plant and personnel. In general, these findings serve as a support for the strong evidence of telemedicine to transform health in rural settings.
Increase in Access to Healthcare
Telemedicine is basically employment of some of technology and telecommunication to render and facilitate remote healthcare services. With the advancement of technology, telehealth has emerged as a means to enhance rural access to healthcare in a world growing ever more reliant on our digital devices. This report discusses the advantages and drawbacks of telemedicine in enhancing healthcare management and provision in remote regions. It considers how telemedicine can expand access to health care via virtual consultations, distance diagnosis and monitoring, and online medical education.
|
Table 2. Comparison of Increase in Access to Healthcare |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
TEM |
APM |
MIM |
IRM |
Proposed Model |
|
|
10 |
45,3 |
47,2 |
48,6 |
49,1 |
46,8 |
|
20 |
49,5 |
45,9 |
47,8 |
48,3 |
46,1 |
|
30 |
47,6 |
48,9 |
46,4 |
49,2 |
45,7 |
|
40 |
46,5 |
49,8 |
47,1 |
45,4 |
48,7 |
|
50 |
48,1 |
46,9 |
49,4 |
45,6 |
47,3 |
Telemedicine – The Pros and Cons includes the impact of telemedicine on healthcare outcomes, cost-effectiveness and patient satisfaction.
The report’s conclusions can help to improve both telemedicine utilization and the quality of care offered in limited-service facilities.
Cost Savings
As the years have passed, the healthcare industry has made significant advances to ensure that patients, especially those living in distant and remote villages, to gain access to quality treatment through technology, virtual communication tools e.g., telemedicine. In this essay, we will first present the technical aspects of telemedicine and how it changed rural healthcare management and delivery. Secure video conferencing, remote patient monitoring, and secure data storage systems are the main technical components of telemedicine. Telemedicine enables healthcare professionals to consult with patients, track their health, and securely store and share medical information remotely. Telemedicine is a game changer that can reshape the way healthcare is managed and delivered in rural parts of the world through significant cost savings in travel and in-person consultations.
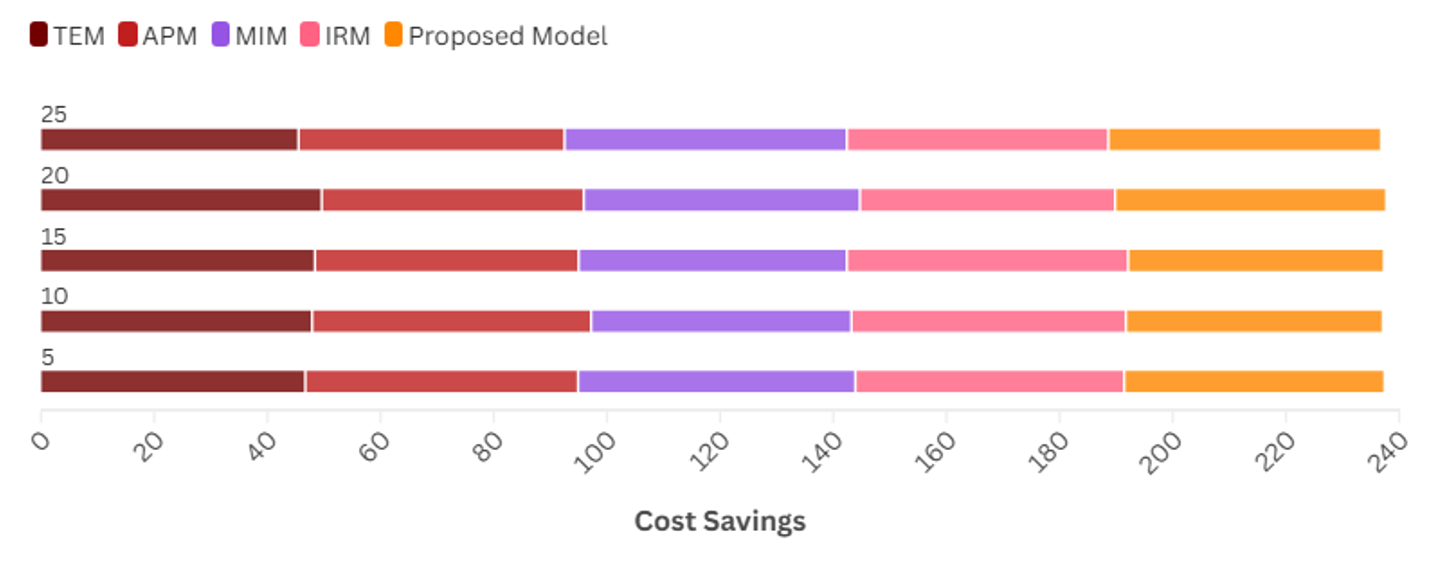
Figure 2. Cost Savings
|
Table 3. Comparison of Cost Savings |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
TEM |
APM |
MIM |
IRM |
Proposed Model |
|
|
5 |
46,7 |
48,2 |
49,0 |
47,5 |
45,8 |
|
10 |
47,9 |
49,3 |
46,0 |
48,5 |
45,2 |
|
15 |
48,4 |
46,6 |
47,4 |
49,7 |
45,0 |
|
20 |
49,6 |
46,3 |
48,8 |
45,1 |
47,7 |
|
25 |
45,5 |
47,0 |
49,9 |
46,2 |
48,0 |
This can create massive cost efficiencies for patients and healthcare providers alike. Moreover, telehealth provides better access to healthcare for rural areas, enhances patient outcome, and helps in better utilization of healthcare resources.
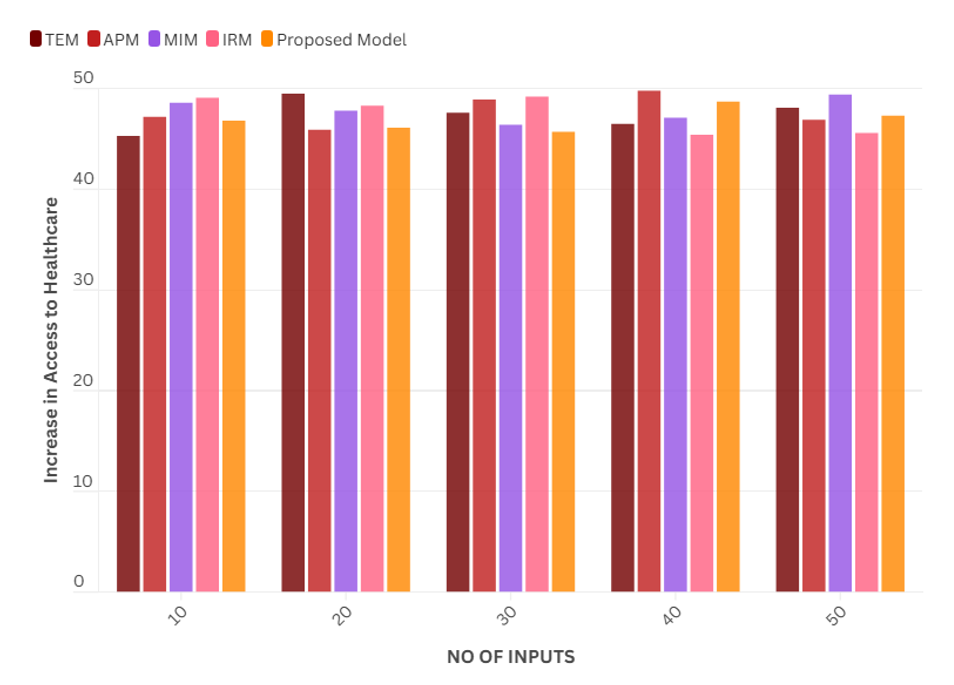
Figure 2. Access to healthcare
To summarize, telemedicine serves as a potential remedy for healthcare services within a rural approach. Through its technical components and cost-saving practices, QUAN has the advantage of being a feasible and effective strategy that can be used to provide quality healthcare services to underserved populations (universities: universities).
Improved Health Outcomes
Telemedicine is a viable solution in rural healthcare settings and has demonstrated positive results in health outcomes. Telemedicine enables healthcare practitioners to remotely communicate with patients, diagnose and treat illness, monitor chronic conditions and deliver health education. Telemedicine outreach has improved access for patients in rural areas to access timely, quality, cost-effective health care, early detection, and management of diseases, reduced need for hospital readmissions, and much improve overall health outcomes.
|
Table 4. Comparison of Improved Health Outcomes |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
TEM |
APM |
MIM |
IRM |
Proposed Model |
|
|
8 |
46,1 |
48,3 |
45,7 |
47,8 |
49,2 |
|
16 |
48,7 |
47,3 |
45,6 |
49,0 |
46,8 |
|
24 |
47,2 |
49,5 |
46,4 |
48,1 |
45,9 |
|
32 |
49,8 |
46,6 |
48,9 |
47,0 |
45,5 |
|
40 |
48,4 |
46,0 |
49,7 |
47,1 |
45,3 |
This also allows the healthcare providers to consume their limited resources wisely and it can cover more population, especially the population residing in remote areas.
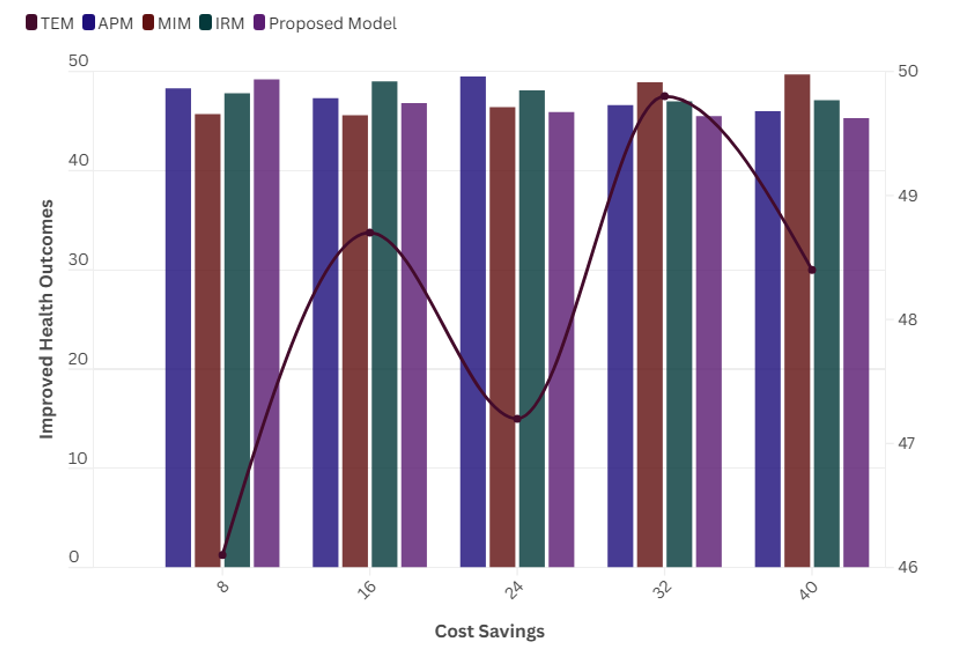
Figure 3. Healthcare Outcomes
As a result, by enabling remote patient monitoring, telemedicine is making it easier for healthcare providers to manage chronic diseases, and by allowing healthcare providers to care for patients not on loaded in the hospital, telemedicine is improving the delivery of healthcare services.
CONCLUSION
The administrative delivery and management of healthcare in a rural area is a boon is proved by telemedicine. The rise of remote consultations with healthcare providers has been an effective solution as it makes healthcare services easily available for patients living in rural areas, without having to travel that saves on cost as well. Telemedicine also assists rural area facilities connect to urban area and learn and gain specialized care that patients did not had. Both of these factors have ensured that telemedicine has enhanced the health outcomes of patients in remote areas by providing timely and accurate diagnosis and treatment. It has also lowered hospital readmissions and increased patient satisfaction. Telemedicine has helped in other areas as well, including overcoming the shortage of healthcare in rural areas through virtual consultations and virtual training. However, challenges still exist including access to technology and low internet availability in rural areas. There is still the need for more research and investment in telemedicine infrastructure to fully leverage its capabilities in regulating healthcare within remote locations. In general, telemedicine remains a valuable tool for meeting the healthcare demands in health care systems in rural communities and could have the impact in the future.
REFERENCES
1. Chen J, Amaize A, Barath D. Evaluating telehealth adoption and related barriers among hospitals located in rural and urban areas. J Rural Health. 2021;37(4):801-11.
2. Harkey LC, Jung SM, Newton ER, Patterson A. Patient satisfaction with telehealth in rural settings: a systematic review. Int J Telerehabil. 2020;12(2):53.
3. Kiberu VM, Scott RE, Mars M. Assessment of health provider readiness for telemedicine services in Uganda. Health Inf Manag J. 2019;48(1):33-41.
4. Gillespie SM, Moser AL, Gokula M, Edmondson T, Rees J, Nelson D, et al. Standards for the use of telemedicine for evaluation and management of resident change of condition in the nursing home. J Am Med Dir Assoc. 2019;20(2):115-22.
5. Muzammil S. Tele-Health: Is it only for the rural areas? A review on its wider use. Telehealth Med Today. 2020;5(1).
6. Mars M. Assessment of health provider readiness for telemedicine services in Uganda. Health Inf Manag J. 2019;48(1):33-41.
7. Chu C, Cram P, Pang A, Stamenova V, Tadrous M, Bhatia RS. Rural telemedicine use before and during the COVID-19 pandemic: repeated cross-sectional study. J Med Internet Res. 2021;23(4):e26960.
8. Mullen-Fortino M, Rising KL, Duckworth J, Gwynn V, Sites FD, Hollander JE. Presurgical assessment using telemedicine technology: impact on efficiency, effectiveness, and patient experience of care. Telemed e-Health. 2019;25(2):137-42.
9. Niznik JD, He H, Kane-Gill SL. Impact of clinical pharmacist services delivered via telemedicine in the outpatient or ambulatory care setting: a systematic review. Res Soc Adm Pharm. 2018;14(8):707-17.
10. Ruiz de Adana MS, Alhambra-Expósito MR, Muñoz-Garach A, Gonzalez-Molero I, Colomo N, Torres-Barea I, et al. Randomized study to evaluate the impact of telemedicine care in patients with type 1 diabetes with multiple doses of insulin and suboptimal HbA1c in Andalusia (Spain): PLATEDIAN study. Diabetes Care. 2020;43(2):337-42.
FINANCING
The authors did not receive financing for the development of this research. Thanks to Universidad Libre Colombia Seccional Cúcuta for the technical support provided.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Formal analysis: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Research: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Methodology: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Project management: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Resources: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Software: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Supervision: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Validation: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Display: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Writing - original draft: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.
Writing - proofreading and editing: Lulup Kumar Sahoo, Fazil Hasan, RenukaJyothi S.