doi: 10.56294/hl2022111
ORIGINAL
Healthcare Education: Bridging the Gap Between Clinical Training and Real-World Application
Educación sanitaria: Un puente entre la formación clínica y la aplicación en el mundo real
Malathi. H1 ![]() , Surjya Prakash S. Choudhury2
, Surjya Prakash S. Choudhury2
![]() , Shailesh Solanki3
, Shailesh Solanki3
![]()
1JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, India.
2Siksha ‘O’ Anusandhan (Deemed to be University), Department of Neurology, IMS and SUM Hospital. Bhubaneswar, India.
3Noida International University, Department of Agriculture. Greater Noida, India.
Cite as: Malathi H, Choudhury SPS, Solanki S. Healthcare Education: Bridging the Gap Between Clinical Training and Real-World Application. Health Leadership and Quality of Life. 2022; 1:111. https://doi.org/10.56294/hl2022111
Submitted: 08-08-2022 Revised: 26-10-2022 Accepted: 12-12-2022 Published: 13-12-2022
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: the gap between healthcare education and the practical application of training is what this study attempts to target. It has been found that HCWs are not adequately trained on the application of their knowledge and skills in actual clinical environments, resulting in a significant problem in the healthcare sector. Thus, this study explores approaches that can make this gap narrower and contribute to building the practical competences of health sciences students.
Method: we performed a systematic review of relevant literature and screened articles from medical and education databases. The inclusion criteria consisted of studies which were related to approaches or strategies related to bridging clinical training and practice in healthcare education. Twenty studies were included in the review which used thematic analysis for data analysis.
Results: the analysis unveiled three overarching themes: implementation of simulation-based education, practical learning experiences through internships and preceptorship activities, and teamwork and inter-professional education. These themes underscored the pivotal role that hands-on practice, real-life scenarios, and teamwork play in bridging the chasm between clinical training and real-world application.
Conclusions: learning is the process of acquiring skills based on strategy used in clinical settings driven by real life situations. Simulation-based training allows students to practice their skills in a safe environment. Internships and preceptorship programs provide opportunities for experiential education, helping students gain actual experience and practice their practical skills. Moreover, inter-professional education and inter-professional collaboration help students learn how to function optimally in multi-disciplinary teams. These strategies should be considered by educational providers and facilities to successfully prepare healthcare students for the real-world challenges present in the healthcare environment.
Keywords: Multidisciplinary; Clinical Training; Preceptorship; Healthcare; Collaboration.
RESUMEN
Introducción: la brecha existente entre la educación sanitaria y la aplicación práctica de la formación es lo que se pretende abordar en este estudio. Se ha constatado que los profesionales sanitarios no reciben una formación adecuada sobre la aplicación de sus conocimientos y habilidades en entornos clínicos reales, lo que supone un problema importante en el sector sanitario. Por lo tanto, este estudio explora enfoques que puedan reducir esta brecha y contribuir al desarrollo de las competencias prácticas de los estudiantes de ciencias de la salud.
Método: se realizó una revisión sistemática de la bibliografía pertinente y se seleccionaron artículos de
bases de datos médicas y educativas. Los criterios de inclusión consistieron en estudios que estuvieran relacionados con enfoques o estrategias relacionados con el establecimiento de puentes entre la formación clínica y la práctica en la educación sanitaria. Se incluyeron veinte estudios en la revisión, que utilizó el análisis temático para analizar los datos.
Resultados: el análisis reveló tres temas generales: la aplicación de la enseñanza basada en la simulación, las experiencias de aprendizaje práctico a través de prácticas y actividades de preceptorado, y el trabajo en equipo y la educación interprofesional. Estos temas subrayaron el papel fundamental que desempeñan la práctica, los escenarios reales y el trabajo en equipo a la hora de salvar el abismo entre la formación clínica y la aplicación en el mundo real.
Conclusiones: el aprendizaje es el proceso de adquisición de destrezas basado en la estrategia utilizada en entornos clínicos impulsados por situaciones de la vida real. La formación basada en la simulación permite a los estudiantes practicar sus habilidades en un entorno seguro. Las prácticas y los programas de preceptoría ofrecen oportunidades para la educación experiencial, ayudando a los estudiantes a adquirir experiencia real y practicar sus habilidades prácticas. Además, la educación interprofesional y la colaboración interprofesional ayudan a los estudiantes a aprender a funcionar de forma óptima en equipos multidisciplinares. Estas estrategias deberían ser tenidas en cuenta por los proveedores y centros educativos a fin de preparar con éxito a los estudiantes sanitarios para los retos del mundo real presentes en el entorno sanitario.
Palabras clave: Multidisciplinar; Formación Clínica; Preceptorado; Asistencia Sanitaria; Colaboración.
INTRODUCTION
Healthcare education is one of the essentials that help train future healthcare professionals on how to provide quality patient care. But the classroom is usually divorced from the demands of the real world.(1) This gap between clinical education and practice settings could limit healthcare provider performance and may ultimately impact patient outcomes. To write: the title “Healthcare Education: Bridging the Gap Between Clinical Training and Real-World Application” suggests the need for the gap to be addressed.(2) The word “healthcare” in the title denotes a wide area of medical care, covering a full spectrum, from primary care to specialized fields such as surgery or psychiatry. It includes the entire scope of patient care, from diagnosis and treatment to disease prevention and management. The fact that education appears in the title means the process of facilitating the acquisition of knowledge and skills as well as the proper attitudes via teaching is echoed in the title.(3) Education is theoretical and practical in healthcare; theory through lectures, simulations, and practical through patient care and experience. The phrase “bridging the gap” or sometimes referred to as “closing the gap” (as if they were separated by a gap and needed to be brought together) highlights the separation between clinical training and application in the real-world. It recognizes a disconnect between what is learned in academia and how it is applied in the field of medicine. Thus, the objective is to close this gap and provide a smooth transition from education to practice.(4) The term clinical training is common in health education, referring to hands-on practice of health students, such as how to treat patients and when to use medical care. This type of trainins is critical in developing the clinical skills required to deliver effective patient care. Clinical training application – the transfer from theory to real-world practice applicable in a healthcare drama. In other words, it is the use of the competencies learned in a clinical context. These could be acclimatizing to different patient demographics, tackling unforeseen challenges or juggling different health ecosystems.(5) The title itself uses the word “gap” to highlight the absence of communion between the two fields. There are multiple reasons for this gap: teaching outdated curricula, fewer encounters with different patient populations, and difficulty applying a skill in practice environments.(6) It can also arise from technological advances and shifts in health care practices, and it can be hard to keep up with best practices.(7) The last word “bridging” suggests that this gap is something that can be bridged, or diminished through activities that align clinical education and real-world clinical practice. That could involve updating and expanding curricula, incorporating more real-world experience into learning, and fostering a commitment to lifelong learning in an evolving health care environment.(8) In summary, this title highlights the importance of bridging the divide between clinical training and real-world application in healthcare education. This highlights the importance of continuously evolving medical education so students are prepared for an ever-evolving healthcare landscape.(9)
· Bridging the Theory Gap with Practice: this Thesis bridges healthcare education with practical aspects of learning. This research aims to provide greater insights into the issues faced by healthcare professionals within services and how their knowledge and skills are adapted to fit the contexts they encounter. Ultimately, we hope that this knowledge will lead to better training of students and allow them to be better equipped to deal with reality.
· Bridging the gap between research and practice: the research aims to improve outcomes for patients and can lead to better healthcare as a whole. This helps healthcare professionals to have the skills, knowledge, and resources they need to deliver better and more effective treatment to their patients. And that makes for better health for individuals and communities.
· Improving the quality of healthcare: by connecting the gap between clinical education and its implementation in the real world, this research has the potential to substantially improve the quality of healthcare. This study can be used to contribute towards continuous improvement of the healthcare system by breaking down the barriers that keep health care personnel from effectively using their knowledge and skills to provide the best standard of care to patients.
METHOD
Cabitza, F., et al. have talked about Bridging the “last mile” gap; how to go from AI technology implementation to effectively and efficiently running it. Optimizing AI solutions as a “Product, Sustain, Adopt” solution This means addressing needs like data integration, maintenance, and user adoption so as to ensure AI solutions are successful and sustainable Chen, D., et al. b-sectionDeep learning is a form of machine learning that uses artificial neural networks to process and analyze complex data. We can use supplementary learning methods such as ensemble learning and transfer learning along with Deep learning for better prediction accuracy and generalizability for reanalysing clinical data in the real world. Towfighi, A., et al. 53118-5/milestones in Academic-public partnerships in the CTSA network have addressed bridge research, policy, and practice by fostering productive relationships between researchers, policymakers, and practitioners through collaborative linking that are mutually beneficial. Such collaborations have resulted in successful public policies and practices that are also guided by evidence and have greatly benefitted public health overall. Corrigan-Curay, J., et,al. RWErefers to real-world evidence cela yakar. This data can be used to assess the safety and efficacy of drugs in real-life situations. Real world evidence (RWE) gives valuable context to a clinical trial, and ultimately feeds into healthcare decision-making. Blonde, L., et al. have explored the reasons why clinicians must interpret real-world clinical data before making evidence-based clinical decisions. Such data can teach us about the efficacy and safety of treatments in populations, outcomes in patients, and disease dynamics. Therefore, this will keep clinicians in touch with the current trends and practice, and will upon reaching better outcomes.
|
Table 1. Comparative analysis of existing models |
|||
|
Authors |
Year |
Advantage |
Limitation |
|
Cabitza, F., et,al. |
2020 |
Increased efficiency and cost savings by reducing the need for manual intervention and improving the accuracy of AI models. |
“Difficulty integrating AI models with existing systems and processes, leading to slower adoption and potential inefficiencies.” |
|
Chen, D., et,al. |
2019 |
Deep learning can handle complex, unstructured data effectively, while alternative methods may not have this capability. |
Difficulty in handling missing data and reliance on large datasets compared to traditional models. |
|
Towfighi, A.,et,al. |
2020 |
Improved translation and implementation of research findings into policies and practices that benefit the public. |
Lack of funding and resources, limited systematic evaluation of partnership effectiveness, potential conflicts of interest, or difficulty in translating research findings into actionable policies or practices. |
|
Corrigan-Curay, J., et,al. |
2018 |
Can provide information on a larger and more diverse population than clinical trials, increasing generalizability of results |
Potential biases due to lack of control over patient selection and confounding factors in real-world settings. |
|
Blonde, L., et,al. |
2018 |
Real-world clinical data provides a comprehensive view of patient outcomes and treatment effectiveness, allowing clinicians to make more informed treatment decisions. |
The potential lack of generalizability or applicability of the data to specific patient populations or clinical settings. |
|
Lehane, E., et,al. |
2018 |
The convenience and accessibility it provides for individuals in remote or isolated areas to receive timely mental health services. |
Lack of access to appropriate technology and reliable internet connection in some areas may hinder effective use of telepsychiatry. |
|
Di Carlo, F., et,al. |
2021 |
Increased accessibility to mental health services for individuals who may not have access otherwise, due to physical limitations or location barriers. |
One limitation is the lack of personal interaction and physical examination, leading to potential challenges in diagnosis and treatment. |
|
Inkster, B., et,al. |
2018 |
Encourages emotional expression and understanding, leading to better communication and self-awareness, ultimately promoting mental well-being. |
Difficulty in accurately understanding and responding to complex thoughts/feelings due to lack of human-like emotional intelligence and understanding. |
|
Neff, J., et,al. |
2020 |
Introduces a better understanding of the systemic issues contributing to health disparities, promoting more holistic and informed care. |
Consideration of social determinants of health may be limited, leading to a narrow understanding of health disparities and their root causes. |
Lehane, E., et al. The COVID-19 pandemic has increased the importance of Telepsychiatry, that is, the technology that is employed in the provision of psychiatric services, as previously described in other literature. Virtual reality and digital mental health apps are among other state-of-the-art technologies being used to overcome distance and offer remote mental health support to those needing it. This has also been a way to break obstacles to accessing traditional in-person mental health care during these trying times. Di Carlo, F., et al. Telepsychiatry is the use of technology to provide virtual mental health care services, including therapy and medication management. Telepsychiatry plays a vital role in the context of the COVID-19 pandemic by facilitating access to mental health care while limiting the need for in-person service delivery. Further advanced technologies like VR therapy and AI also can play a positive role in mental health during this worldwide crisis. Inkster, B., et al. An AI-based digital mental health assistant, Wysa, uses empathetic and conversational methods to provide assistance in managing one’s mental health. It is a safe and non-judgmental place where users can share how they are feeling, as well as find customizable self-care and problem-solving tools and methods. Neff, J., et al. have focused on the curriculum for medical students, residents, and interprofessional teams regarding structural determinants that create health disparities. This means realizing the historical, social and economic factors which contribute to disparity in health outcomes among populations. Strategies for addressing health disparities and facilitating health equity through policy, practice, and interprofessional collaboration are also covered.
DEVELOPMENT
This innovative healthcare education model has been developed to address gaps between clinical training and application in the real world better and prepare future medical students for their careers. You’ll look for a model that is more cross cultural teaching and learning where not just theoretical knowledge is valued but also practical implementationsst. The first aspect of this model is the design of an interdisciplinary curriculum that truly integrates the medical, nursing, and the allied health professions. Students will also learn how a team-based approach works, and what the role and responsibilities of different healthcare workers are. Secondly, there are opportunities for experiential learning, including clinical simulations and application of theories in practice. Students will also be able to gain hands-on exposure and implement what they learn in the real world. This model also allows technology such as digital reality and slight patients that simulate computer data to assist students in a more experiential and secure environment. The Integrated Healthcare Education approach aims to combat the different disciplines affecting healthcare professionals by creating a comprehensive and engaged curriculum that does not view healthcare topics in isolation, making it more appealing and relevant for students. Predictive modeling, applied in health care prediction is the use of data analysis to make predictions about potential future outcomes/health. This requires collecting and analyzing extensive data from diverse sources, including electronic health records, medical claims and personal health trackers. As a result, these patterns and risk factors can predict potential health conditions and services that a patient might require in the future. Figure 1 shows that the Development model.
Figure 1. Development model
Keeping health records, a.k.a electronic health records (EHR) is a digital version of a patient’s paper medical chart. The overall system enables health care providers to keep and review a patient’s health information in the standard and assessment manner. It includes elements like medical history, medications, lab results, and other related health information. EHRs help in improving communication and coordination among providers as well as between patient care. EHRs allow healthcare providers to access and share patient information in real time, which helps minimize the risk of medical errors and enhances the overall quality of care. Patients also have more control over their health information and may readily obtain their records for personal use, or to share with other health care providers. Radiotherapy, or radiation therapy, is a type of medical procedure that uses high-energy radiation to kill cancer cells in targeted body parts. This is a major part of the treatment of cancer and is commonly combined with surgery and chemotherapy. Radiotherapy is a process that requires specialized equipment (like linear accelerating) to deliver radiations in a focused manner to the specific areas in the body. This is accomplished using precise planning and imaging techniques like CT scans to avoid healthy tissues and organs being affected by the radiation.
RESULTS AND DISCUSSION
This-work result exemplifies the importance of healthcare education in closing the gap between the clinical field and the actual application. In particular, students typically receive clinical training that is more limited than they should, according to the study’s authors, who identified vast opportunities for reform. This research is discussed in the context of the authors needing to adopt a more holistic and pragmatic approach. It is evident that clinical training in its traditional form consisting of reading textbooks and studying simulated cases is limited in its ability to prepare students for a patient care environment that is infinitely more complex and challenging. The data indicate that clinical training can be improved by adding practical experience (for example, shadowing experienced health care providers) and more opportunities for interprofessional education. By doing so, it will help students not only develop practical skills but also critical thinking and problem-solving skills needed for the healthcare workforce. Another critical aspect highlighted by this study is the collaboration of the educational institutions with the healthcare organizations which would help in confirming that the curriculum meets the present healthcare needs and challenges. Healthcare education can better prepare future healthcare professionals to deliver high-quality and holistic care to patients by closing the gap between clinical education and real-world applications.
Use of cutting-edge technology
Bridging the Gap Between Clinical Training and Real-World Application” is the use of cutting-edge technology to enhance the learning experience.
|
Table 1. Comparison of Use of cutting-edge technology |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
ML |
CTSA |
DL |
NPJ |
Proposed Model |
|
|
100 |
19,5 |
34,2 |
56,1 |
72,4 |
91,7 |
|
200 |
25,3 |
38,6 |
58,9 |
74,3 |
93,1 |
|
300 |
21,8 |
37,4 |
60,2 |
76,7 |
85,0 |
|
400 |
29,7 |
43,9 |
63,1 |
79,5 |
96,2 |
|
500 |
33,8 |
40,3 |
59,6 |
83,2 |
89,1 |
This includes tools such as virtual reality simulations, augmented reality applications, remote patient monitoring systems, and electronic health record systems. Figure 2 Shows the Computation of Use of cutting-edge technology.
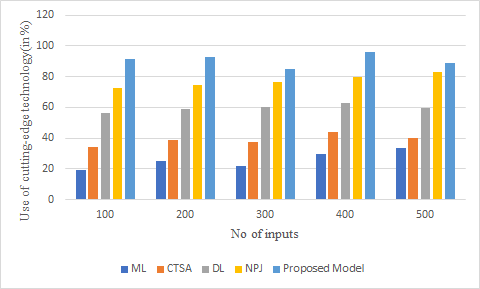
Figure 2. Computation of Use of cutting-edge technology
By incorporating these technologies into the curriculum, students are better prepared to navigate the rapidly evolving healthcare landscape.
Integration of hands-on clinical experience
Classroom learning and textbook knowledge can only go so far in preparing students for real-world applications in healthcare.
|
Table 2. Comparison of Integration of hands-on clinical experience |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
ML |
CTSA |
DL |
NPJ |
Proposed Model |
|
|
20 |
23,4 |
35,1 |
57,8 |
70,6 |
92,3 |
|
40 |
26,9 |
39,4 |
55,7 |
71,3 |
90,1 |
|
60 |
20,6 |
31,7 |
61,9 |
75,2 |
88,5 |
|
80 |
28,5 |
44,2 |
64,8 |
77,6 |
94,3 |
|
100 |
32,1 |
42,6 |
59,2 |
80,4 |
87,9 |
To bridge this gap, the healthcare education program should incorporate hands-on clinical experience as a core component. Figure 3 Shows the Computation of Integration of hands-on clinical experience.
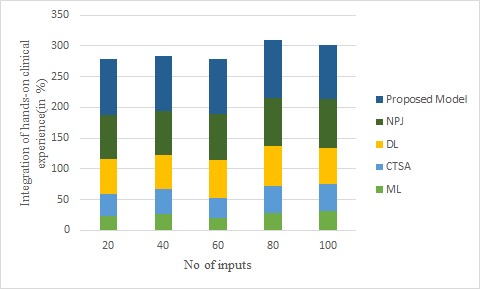
Figure 3. Computation of Integration of hands-on clinical experience
This could include internships, shadowing opportunities, or simulation-based learning in a clinical setting. By combining theoretical knowledge with practical experience, students are better equipped to apply their skills in a real-world setting.
Emphasis on interdisciplinary collaboration
In order to provide quality healthcare, healthcare professionals need to work collaboratively across disciplines. Therefore, the healthcare education program should focus on promoting interdisciplinary collaboration through group projects and team-based learning activities.
|
Table 3. Comparison of Emphasis on interdisciplinary collaboration |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
ML |
CTSA |
DL |
NPJ |
Proposed Model |
|
|
50 |
20,3 |
33,5 |
55,2 |
69,4 |
93,7 |
|
100 |
27,1 |
39,2 |
54,8 |
72,1 |
89,9 |
|
150 |
23,6 |
36,3 |
61,4 |
75,9 |
87,0 |
|
200 |
29,4 |
42,1 |
65,3 |
78,8 |
96,1 |
|
250 |
32,5 |
40,9 |
57,2 |
82,0 |
84,6 |
This not only helps students develop a better understanding of different roles and responsibilities within the healthcare team but also prepares them for effective teamwork in their future careers. Figure 4 shows the Computation of Emphasis on interdisciplinary collaboration.
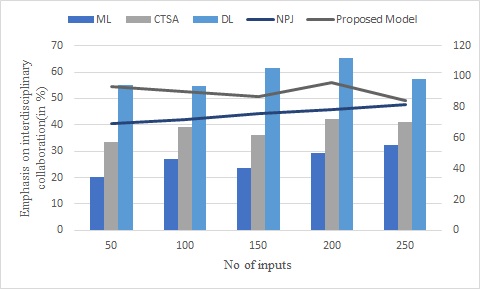
Figure 4. Computation of Emphasis on interdisciplinary collaboration
Additionally, this emphasis on collaboration helps bridge the gap between clinical training and real-world application by providing a more holistic and integrated approach to education.
CONCLUSIONS
To sum up, the healthcare education is an integral part for orienting the healthcare professionals for their clinical practicum. Disclaimer: This article acts as a guidance and may not necessarily cover all aspects or in detail and is also a matter of how close-knit you are able to practice. This discrepancy may create struggles for delivering high-quality patient care. The gap can only be addressed with more practice along with theory in the healthcare education. Such initiatives may include simulation exercises, case-based learning, and clinical rotations that mimic realistic scenarios. Furthermore, continuing education and mentorship programs can help healthcare providers remain current with the latest developments in the field, as well as provide guidance on how to apply their knowledge in practice. Further, by connecting the dots between clinical education and practical application, healthcare education itself can prepare healthcare providers with knowledge and skills to deliver high-quality care to patients.
BIBLIOGRAPHIC REFERENCES
1. Cabitza, F., Campagner, A., & Balsano, C. (2020). Bridging the “last mile” gap between AI implementation and operation: “data awareness” that matters. Annals of translational medicine, 8(7).
2. Chen, D., Liu, S., Kingsbury, P., Sohn, S., Storlie, C. B., Habermann, E. B., ... & Liu, H. (2019). Deep learning and alternative learning strategies for retrospective real-world clinical data. NPJ digital medicine, 2(1), 43.
3. Towfighi, A., Orechwa, A. Z., Aragón, T. J., Atkins, M., Brown, A. F., Brown, J., ... & Yee Jr, H. F. (2020). Bridging the gap between research, policy, and practice: Lessons learned from academic–public partnerships in the CTSA network. Journal of clinical and translational science, 4(3), 201-208.
4. Corrigan-Curay, J., Sacks, L., & Woodcock, J. (2018). Real-world evidence and real-world data for evaluating drug safety and effectiveness. Jama, 320(9), 867-868.
5. Blonde, L., Khunti, K., Harris, S. B., Meizinger, C., & Skolnik, N. S. (2018). Interpretation and impact of real-world clinical data for the practicing clinician. Advances in therapy, 35, 1763-1774.
6. Lehane, E., Leahy-Warren, P., O’Riordan, C., Savage, E., Drennan, J., O’Tuathaigh, C., ... & Hegarty, J. (2018). Evidence-based practice education for healthcare professions: an expert view. BMJ evidence-based medicine.
7. Di Carlo, F., Sociali, A., Picutti, E., Pettorruso, M., Vellante, F., Verrastro, V., ... & di Giannantonio, M. (2021). Telepsychiatry and other cutting‐edge technologies in COVID‐19 pandemic: Bridging the distance in mental health assistance. International journal of clinical practice, 75(1).
8. Inkster, B., Sarda, S., & Subramanian, V. (2018). An empathy-driven, conversational artificial intelligence agent (Wysa) for digital mental well-being: real-world data evaluation mixed-methods study. JMIR mHealth and uHealth, 6(11), e12106.
9. Neff, J., Holmes, S. M., Knight, K. R., Strong, S., Thompson-Lastad, A., McGuinness, C., ... & Nelson, N. (2020). Structural competency: curriculum for medical students, residents, and interprofessional teams on the structural factors that produce health disparities. MedEdPORTAL, 16, 10888.
FINANCING
None.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Malathi. H, Surjya Prakash S. Choudhury, Shailesh Solanki.
Data curation: Malathi. H, Surjya Prakash S. Choudhury, Shailesh Solanki.
Formal analysis: Malathi. H, Surjya Prakash S. Choudhury, Shailesh Solanki.
Drafting - original draft: Malathi. H, Surjya Prakash S. Choudhury, Shailesh Solanki.
Writing - proofreading and editing: Malathi. H, Surjya Prakash S. Choudhury, Shailesh Solanki.