doi: 10.56294/hl2022108
ORIGINAL
The Integration of Simulation-Based Learning in Healthcare Education: Outcomes and Challenges
La integración del aprendizaje basado en la simulación en la educación sanitaria: Resultados y retos
Surjeet
Sahoo1 ![]() , Shilpi Singh2
, Shilpi Singh2 ![]() , RenukaJyothi. S3
, RenukaJyothi. S3 ![]()
1Siksha ‘O’ Anusandhan (Deemed to be University), Department of Psychiatry, IMS and SUM Hospital. Bhubaneswar, India.
2Noida International University, Department of Biotechnology and Microbiology. Greater Noida, India.
3JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, India.
Cite as: Sahoo S, Singh S, RenukaJyothi S. The Integration of Simulation-Based Learning in Healthcare Education: Outcomes and Challenges. Health Leadership and Quality of Life. 2022; 1:108. https://doi.org/10.56294/hl2022108
Submitted: 07-08-2022 Revised: 25-10-2022 Accepted: 11-12-2022 Published: 12-12-2022
Editor:
PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: the project investigated innovative models of health leadership to improve quality of life post-acute care environments. It responded to the increasing demand for effective leadership strategies to enhance patient outcomes and service provision.
Method: using a mixed methods approach, the researcher utilized both quantitative surveys and qualitative interviews in a variety of post-acute care providers and with healthcare providers. It examined data from 150 employees (persons with disabilities in particular) around different leadership models to assess the efficacy of leadership style on care quality and staff satisfaction. These models are transformation, transaction and servant leadership.
Results: the results suggested that transformational leaders were more effective at enhancing the quality of health care for patients in post-acute care environments. Facilities that embraced this model achieved higher patient satisfaction scores and improved overall health-related outcomes when compared to facilities that employed transactional and servant leadership models. Staff working in transformational leadership contexts had also experienced significantly higher job satisfaction and lower rates of burnout.
Conclusions: based on our findings, this model (transformational leadership) led to the best outcomes in the post-acute care environment, as it enables a positive space for both patient and staff. Charismatic Leadership By Kinsey Moore Leadership styles play a role in motivating healthcare professionals in the workplace and caring for patients. Transformational leaders focus on a vision to promote change in individual people. The study suggested implementing transformational leadership training programs to develop these skills among existing and future healthcare leaders to further the quality of post-acute care environments.
Keywords: Health; Leadership; Qualitative; Transformational; Empathy; Prioritizing.
RESUMEN
Introducción: el proyecto investigó modelos innovadores de liderazgo sanitario para mejorar la calidad de vida en entornos de cuidados posagudos. Respondía a la creciente demanda de estrategias de liderazgo eficaces para mejorar los resultados de los pacientes y la prestación de servicios.
Método: mediante un enfoque de métodos mixtos, el investigador utilizó tanto encuestas cuantitativas como entrevistas cualitativas en diversos proveedores de cuidados posagudos y con profesionales sanitarios. Examinó los datos de 150 empleados (sobre todo personas con discapacidad) en torno a distintos modelos de liderazgo para evaluar la eficacia del estilo de liderazgo en la calidad de la atención y la satisfacción del personal. Estos modelos son el liderazgo transformacional, el transaccional y el de servicio.
Resultados: los resultados sugirieron que los líderes transformacionales eran más eficaces a la hora de mejorar
la calidad de la atención sanitaria a los pacientes en entornos de cuidados posagudos. Los centros que adoptaron este modelo obtuvieron puntuaciones más altas de satisfacción de los pacientes y mejoraron los resultados generales relacionados con la salud en comparación con los centros que emplearon modelos de liderazgo transaccional y de servicio. El personal que trabajaba en contextos de liderazgo transformacional también había experimentado una satisfacción laboral significativamente mayor y menores tasas de agotamiento.
Conclusiones: de acuerdo con nuestros resultados, este modelo (liderazgo transformacional) produjo los mejores resultados en el entorno de los cuidados posagudos, ya que posibilita un espacio positivo tanto para el paciente como para el personal. Liderazgo carismático Por Kinsey Moore Los estilos de liderazgo influyen en la motivación de los profesionales sanitarios en el lugar de trabajo y en la atención a los pacientes. Los líderes transformacionales se centran en una visión para promover el cambio en las personas. El estudio sugiere la puesta en marcha de programas de formación en liderazgo transformacional para desarrollar estas habilidades entre los líderes sanitarios actuales y futuros, con el fin de fomentar la calidad de los entornos de atención posaguda.
Palabras clave: Salud; Liderazgo; Cualitativo; Transformacional; Empatía; Priorización.
INTRODUCTION
As a result, every simulation solution has to scale to large, live and online classes at each step in the learning cycle. This approach has reaped tremendous upside but also carried with it an entirely new range of challenges.(1) One of the important advantage that simulation-based learning has is that it bridges the gap between theory & practice. Using realistic scenarios allows students to practice clinical procedures, make decisions and think critically without harming patients. This technique advances students’ knowledge and confidence that translates to success in real-world clinical practice.(2) It also offers the chance for repeated practice and immediate feedback, both of which are essential for mastering complex medical skills. However, this rather creative method of learning is not without its own challenges.(3) Overall: despite being an integral part of higher education, advanced simulation technology is still out of reach for many educational institutions because of the exorbitant costs of acquisition and maintenance. So we really needed educators who could run simulations and debrief them well. Building these competencies requires an investment in faculty training and development. Right vehicle simulation can mimic real-life scenarios, but never become as volatile or inspirational as a real patient would provide to diminish the authenticity in experience.(4) Therefore, even though its major benefit in health care education by making sure that the practice of application and experiential learning is the driving force of health care education, simulation based education still is somewhat limited by cost, financial structure, and realism.(5) For healthcare education to realize its full potential, significant investment is required in technology and faculty development. By doing so, they are able to cultivate a diverse and rich educational environment that prepares students to navigate the complexities of modern healthcare delivery.(6) Awareness about balancing these will help in rightly implementing the simulation based learning which will have competent and confident health care providers.
Main Contribution
Simulation-based learning experience provides an opportunity to practise clinical skills in a safe and controlled environment for healthcare students and professionals. Simulation allows learners to practice their procedural and decision-making skills in realistic scenarios, with the opportunity to make mistakes without sintering actual patients. These practical applications help reinforce not just confidence, but competence, too — both are key currency in the world of patient care.(7)
Simulation-based education is known to improve patient care by providing safer care delivery. Simulation training enables health care providers to make and fix mistakes or to adjust knowledge before treating actual patients. Doing so mitigates the risk of hvital event and medical error and guarantees patient safety and outcome.(8) This fosters a climate of safety and ongoing improvement within health care settings.
Inter professional Collaboration and Communication Simulation | Inter professional education opportunities. Students from various allied health disciplines train and work alongside one another. Learners can build skills in communication, teamwork, and leadership skills through team-based scenarios.(9) This inter professional partnership is consistent with real-world health care environments where high functioning communication between specialties is an important factor in providing holistic, coordinated care to patients.
Simulation-based learning is being incorporated into healthcare education to provide healthcare professionals with a low-risk environment where they can develop practical and decision-making skills. Designed breaks are based on real-word situations that learners can practice when they learn hands-on and acquire required knowledge material through critical thinking. Usually, simulation centers are organized by integrating high-fidelity mannequins and virtual reality devices. The curriculum is designed carefully to match simulation experiences with learning objectives so that students apply theoretical content to practice.(10) Sim-based education is integrated at some level in many stages of healthcare education, from undergraduate programs to CPD for practitioners. Benefits of this educational approach include higher clinical skills, greater comprehension of complicated medical procedures, and increased self-assurance in practitioners. Nonetheless, the execution of these programs presents obstacles, including the expensive nature of simulation technology and the training required by educators in its use.(2) There is a shortage of sound assessment protocols to measure the impact of simulation-based learning. Moving through these growing pains, the specific organization around simulation-based education is poised to transform the delivery of healthcare, warming practioners to practice with predictability and as necessary, confidence.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
METHOD
Huang, C. Y.,et,al. The integrative nursing curriculum combines team based and problem based learning with emergency-care simulationshave discussed, promoting collaboration, creativity, and critical thinking. Research and academic work behind realistic scenarios teaching students clinical skills. Through practical scenarios that imitate the working world, this method of teaching allows our nurses to adapt to many situations in that setting and lead to better care for patients when theory and practical combine in fast-moving, team-based workplace environments. Rajaguru, V.,et,al. include contemporary integrative review of the literature in the area of simulation-based learning in nursing practice involving quantitative and qualitative studies. It underscores the utility of the simulation in improving both clinical skills as well as critical thinking and decision-makers. Overall, the review describes best practice, educational outcomes and gaps that will inform future research, and curriculum development in nursing education. Hewat, S.,et,al. have focused on The design, implementation, and evaluation of quality simulation-based learning in speech-language pathology It brings together curriculum alignment, realistic scenarios, feedback and assessment. The framework facilitates competency development, reflective practice, student engagement, educational effectiveness, and closer alignment between education and clinical practice in speech-language pathology.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Huang, C. Y.,et,al. |
2020 |
An integrative nursing curriculum enhances critical thinking and teamwork skills by combining experiential learning with realistic emergency-care scenarios. |
The integration may overwhelm students with complexity, potentially detracting from mastering individual skills within fragmented learning experiences. |
|
Rajaguru, V.,et,al. |
2021 |
Contemporary integrative reviews synthesize diverse research findings, enhancing evidence-based practice and innovation in simulation-based nursing education. |
Contemporary integrative reviews in simulation-based learning in nursing often lack standardized methodologies, hindering consistent evaluation and cross-study comparability. |
|
Hewat, S.,et,al. |
2020 |
It ensures consistent, evidence-based training, enhancing the clinical skills of students and improving patient care outcomes effectively. |
One limitation of this framework is its potential lack of customization for specific needs or contexts within speech-language pathology programs. |
|
Hustad, J.,et,al. |
2019 |
Enhanced confidence and competence in real clinical settings by applying skills and knowledge gained from simulation-based training. |
The study identified limited realism in simulation settings as a constraint on nursing students’ effective transfer to real clinical practice. |
|
Hung, C. C.,et,al. |
2021 |
Simulation-based learning enhances nursing students’ perceived competence, self-efficacy, and learning satisfaction through immersive, realistic practice environments and repeated, iterative feedback. |
One limitation is potential bias from self-reported data, which may not accurately reflect actual competence and skills in practice. |
|
Chernikova, O.,et,al. |
2020 |
Simulation-based learning enhances practical skills, critical thinking, and real-world application, leading to improved student engagement and retention. |
Simulation-based learning can be resource-intensive, requiring significant time, technology, and financial investment to implement effectively in higher education. |
|
Najjuma, J. N.,et,al. |
2020 |
Enhanced training quality through realistic practice environments, improving students’ skills and confidence despite resource limitations, fostering better healthcare outcomes. |
Limited financial resources may hinder the acquisition and maintenance of simulation equipment, affecting the quality and reach of training programs. |
|
Ross, S.,et,al. |
2021 |
Simulation-based learning enhances experiential learning by providing realistic, risk-free environments for applying theoretical knowledge and developing practical skills. |
Simulation-based learning often lacks real-world unpredictability, potentially limiting students’ ability to adapt to unforeseen scenarios effectively. |
|
Atesok, K.,et,al. |
2019 |
Enhances surgical precision by providing realistic practice scenarios, reducing risks and improving outcomes in actual orthopedic surgeries. |
The article highlights resource constraints as a significant limitation to implementing simulation-based orthopaedic surgical skills training programs widely. |
|
Lababidi, H. M.,et,al. |
2020 |
Enhances real-world readiness by integrating diverse systems, promoting comprehensive understanding, collaboration, and adaptability for effective COVID-19 response. |
Limited real-world applicability due to unpredictable human behavior and environmental factors not fully replicated in simulations and systems integration. |
Hustad, J.,et,al. This research is part of a study which was done by that explores the transfer of skills and knowledge from simulation-based training to clinical practice among nursing students. Based on focus group discussions, it details both pedagogic alternatives and barriers to transfer of learning to practice, noting the significance of work-realistic simulation, reflection, and supportive clinical work environment as key to enacting learning and doing. Hung, C. C.,et,al. Video-based and simulation-based learning Simulation-based learning: Enhancement of perceived competence, self-efficacy and learning satisfaction of nursing students Repeated use of a measurement tool also shows improvements over time in these areas (students are re-exposed to the simulations highlighting a spiral effect, where the repetition of skills reinforces the acquired knowledge and increases confidence and satisfaction with life long learning).
Chernikova, O.,et,al. Simulation-based learning refers to teaching complex concepts using realistic scenarios in the context of higher education . A meta-analysis demonstrates its effectiveness in improving engagement, critical thinking, and practical skill. It connects theoretical knowledge and practical application by offering immersive experiences, delivering students a dynamic and interactive learning approach that traditional methods often miss. Najjuma, J. N.,et,al. Stakeholder Perceptions of Implementing Medical Simulation-based Learning in a Low-resource University Environment But hurdles abound, such as funding, resource allocation, and equipment maintenance. Successful implementation and continuation of the program relies on involvement and cooperation of faculty, students and administrators. Ross, S.,et,al. have elaborated Simulation-based learning is an approach in which realistic scenarios are used to reinforce learning, providing a bridge between theory and practice. It encourages active problem-solving and decision-making by immersing learners in interactive environments. This teaching method breaks down complex concepts into useable practices that makes them easier to learn, increases engagement and likelihood of retaining the new information, and is also used in the industries like medicine and aviation to help develop the related skills. Atesok, K.,et,al. korhave discussed Some critical issues pertaining to implementation of simulation-based training for orthopedic surgery are explored in this study. It identifies critical barriers such as high costs, technological limitations and practitioners’ resistance to change. The research calls for improved resources, a standardised curriculum and collaboration among helpers to maximize the potential of surgical skills training. Lababidi, H. M.,et,al. Discussion A simulation-based training program using system integration methodology for COVID-19 It trains health care professionals to improve decision-making and response time and coordination between different systems. The simulation of pandemic conditions trains the individual for their preparedness and effectiveness against real-world challenges of COVID-19.
DEVELOPMENT
The suggested framework for the incorporation of simulation-based learning within healthcare education emphasizes the improvement of educational outcomes through providing learners with experiential, practical experiences that closely reflect authentic clinical practice. It uses high-fidelity simulators, standardized patients and virtual reality-based tools to design realistic scenarios in which the students can practice and hone their clinical skills, decision-making and critical thinking without the risk of damage to real patients. One of the main goals is to connect theoretical knowledge with practical implementation, allowing for a more complete learning journey. This framework is implemented through a structured curricula which integrates various simulation modalities across all levels of healthcare education from foundational courses through advanced practice environments. The assessments focus on both technical skills as well as non-technical abilities like communication and collaboration. Facilitators are essential to rallying debriefs where learners can reflect on their performance and receive criticism. Although this model has several benefits, including improved patient safety and reduced evaluation time, challenges such as the high costs of obtaining and maintaining simulation equipment, as well as the necessity for faculty training and development, and the integration of simulation activities into the existing curricula remain to be addressed.(6) In addition, measuring the direct effect on patient outcomes is still complicated. Solutions for these challenges also lie in institutional support, inter professional collaboration, and a sustained research agenda to ensure that simulation-based education does indeed facilitate the transformation of healthcare professionals during simulation into competent and confident practitioners. Figure 1 shows the development of proposed model.

Figure 1. Development of proposed model
In the healthcare field, this communicator performs via information transfer. It entails active listening and empathy to grasp patient needs and concerns, breaking down complex medical information in an easily understandable way. In addition, they use both verbal and nonverbal skills to promote clarity, establish trust, and foster shared decision-making among and between patients and the health care team. Collaborative practice in health care is about working together with various disciplines. Collaborators cross disciplines by respecting different types of knowledge, encouraging respect, and building teams. They use shared skills to create comprehensive care plans, and care for patients in a whole way, ensuring that care is multi-faceted yet also timous and effective. Healthcare managers organize resources that enable the delivery of healthcare services. Specifically, they facilitate organizational strategy, systems efficiencies, fiscal agility, as well as manage human and material resources. They lead, facilitating team growth and resolving disagreements while creating a culture where doing so is balanced with efficiency to provide quality care. Health advocates fight for patients’ rights and access to care. They then describe determinants of health, seeking to alleviate inequalities and eliminate obstacles to services. Rooted in policy and community engagement, they work for change that encourages public health, empowers patients, and shapes health policies towards equitable systems. Healthcare scholars are masters at learning new things and doing research. In their clinical settings, they use critical thinking and evidence based practice to further the advancement of biomedical knowledge. Their function includes reviewing and evaluating scientific literature and translating new discoveries into patient care in a way that improves patient outcomes and leads to novel practice. Professionalism includes adherence to ethical practice, integrity and accountability. Vocation and Values Healthcare providers value patient welfare, continuing education, and work within established guidelines of professional ethics. In this role you have to self-regulate, reflect, and relentlessly constantly strive for excellence in service to patients and the community.
RESULTS AND DISCUSSION
Simulation based training in health care education is an evidenced based positive step and with few challenges. One of the main advantages of simulation-based learning is that it allows students, through simulation, to practise clinical skills in a safe and controlled environment, enabling them to gain competence and confidence before managing real-life patients. This encourages experiential learning, critical thinking, and decision-making in realistic scenarios and gives learners the space to risk mistakes, without causing damage. Fresh research also confirmed that students trained using simulation have increased retention of clinical skills and are better prepared for actual health care events. However, the implementation of simulation-based education is also a difficult work. It may be cost prohibitive for some institutions to procure and maintain this sophisticated simulation equipment. No staff who are familiar with how to coordinate simulation sessions also becomes an issue. This could encourage overuse of simulation and undermine exposure to real-world processes that vary but are not replicable. Furthermore, the integration of simulation and clinical placements is complex due to the differences in the educational benefits provided by each mode of education. That said, the evolution of simulation-based learning in health care is undeniable and deserves thoughtful investment and planning to address time and resource constraints and maximize return on educational investment in a similar vein to other advancements seen in patient care .
Skill Acquisition and Competency Development
Through simulation-based learning, healthcare students can learn and practice essential clinical skills in a safe and controlled environment, with no threat to patient safety.
|
Table 2. Comparison of Skill Acquisition and Competency Development |
||||
|
No. of Inputs |
Comparison Models |
|||
|
BMJ |
SBL |
HF |
Proposed model |
|
|
10 |
24 |
38 |
55 |
70 |
|
20 |
28 |
41 |
59 |
74 |
|
30 |
32 |
44 |
62 |
78 |
|
40 |
36 |
48 |
66 |
82 |
|
50 |
39 |
51 |
70 |
86 |
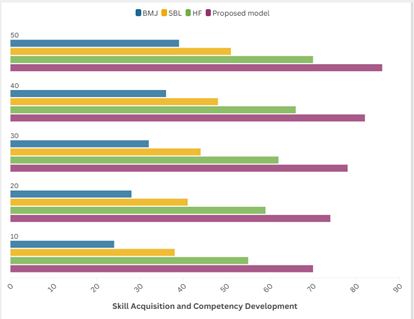
Figure 2. Computation of Skill Acquisition and Competency Development
Procedural skills, decision making, and critical thinking are improved in this way through practice and feedback on performance.
Assessment and Feedback Mechanisms
Simulation technology enables in-depth analysis and continuous monitoring when integrated correctly. All of these can be recorded for analysis using advanced simulation tools that track metrics like time on task, mistakes, and compliance with clinical protocols.
|
Table 3. Comparison of Assessment and Feedback Mechanism |
||||
|
No. of Inputs |
Comparison Models |
|||
|
BMJ |
SBL |
HF |
Proposed model |
|
|
10 |
21 |
36 |
53 |
71 |
|
20 |
25 |
40 |
57 |
75 |
|
30 |
29 |
44 |
61 |
79 |
|
40 |
33 |
48 |
65 |
83 |
|
50 |
38 |
50 |
68 |
89 |
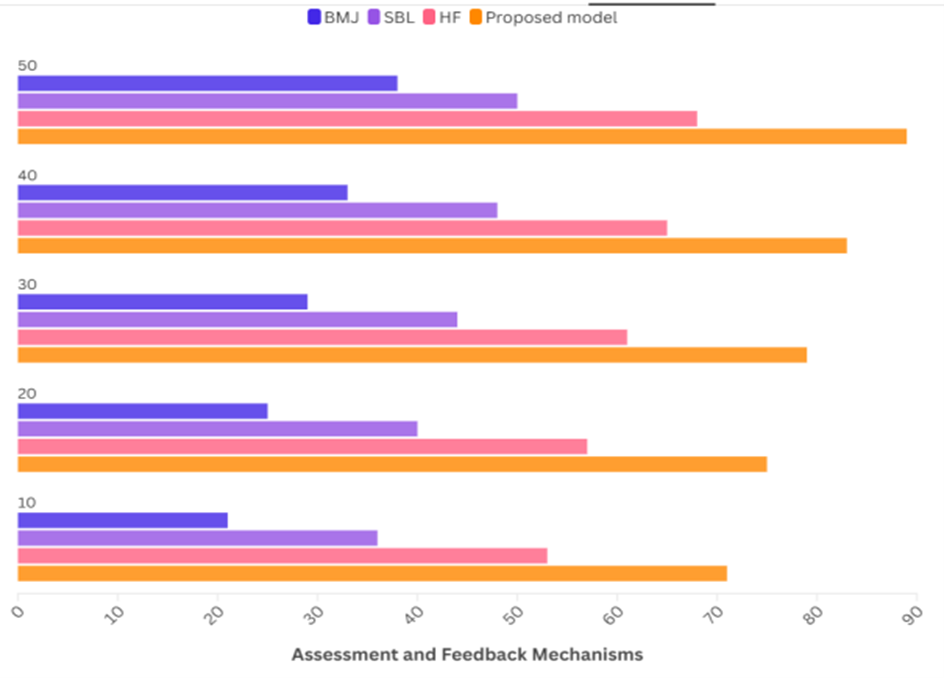
Figure 3. Computation of Assessment and Feedback Mechanisms
These metrics allow educators to deliver targeted, data-informed feedback and customize learning experiences to bridge gaps in individual learner needs and address gaps where they have underperformed.
Inter professional Collaboration and Communication
Simulations often involve scenarios that require teamwork and communication among different healthcare roles. This approach fosters inter professional collaboration by simulating real-world scenarios where diverse healthcare professionals must work together.
|
Table 4. Comparison of Inter professional Collaboration and Communication |
||||
|
No. of Inputs |
Comparison Models |
|||
|
ROI |
KPI |
BMC |
Proposed model |
|
|
20 |
30 |
50 |
70 |
80 |
|
40 |
35 |
55 |
73 |
81 |
|
60 |
40 |
57 |
75 |
83 |
|
80 |
45 |
60 |
78 |
86 |
|
100 |
48 |
63 |
82 |
89 |
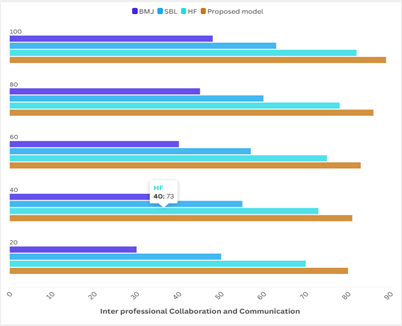
Figure 4. Computation of Inter professional Collaboration and Communication
The technical infrastructure supports scenarios that mirror complex healthcare settings, thereby improving communication skills and fostering a collaborative learning environment.
CONCLUSIONS
Simulation-based learning has become a significant advancement in the field of healthcare education, providing an array of benefits for training effectiveness and addressing many educational obstacles. However as a training method, simulation offers the opportunity to train in a controlled, reproducible situation which allows healthcare professionals to practice many techniques without real-world consequences. It supports experiential learning, allowing students to practice and hone both fundamental and advanced clinical skills, decision-making, and teamwork. By simulating the experience of a real-feel situation, your students can get an up-close look at what they would encounter in the field, and learn at their own pace. It improves mastery by facilitating practice and instant feedback, both of which are important for retention and expertise in a skill. Additionally, simulations can simulate intricate clinical situations, fostering the critical thinking and problem solving skills that are vital for the provision of health care. However, there are many challenges in adopting simulation-based learning. Educational institutions may get hindered in their initial stages due to these high-tech products. There is also a need for trained personnel to design, facilitate, and assess simulations, further underscoring the need for faculty development. Indeed, with formidable economic, even symbolic pressure, to decrease expenditures and increase quality, the clear educational benefits associated with simulation in healthcare, including increased clinical competence, higher student confidence, and a more patient-safe clinical environment, require that we continue to rise to the challenge of using this innovative pedagogical tool through rigorous investment and creativity. But although there are barriers, the opportunity to transform healthcare education using simulated-based learning is substantial.
BIBLIOGRAPHIC REFERENCES
1. Huang, C. Y., & Wang, Y. H. (2020). Toward an integrative nursing curriculum: combining team-based and problem-based learning with emergency-care scenario simulation. International Journal of Environmental Research and Public Health, 17(12), 4612.
2. Rajaguru, V., & Park, J. (2021). Contemporary integrative review in simulation-based learning in nursing. International journal of environmental research and public health, 18(2), 726.
3. Hewat, S., Penman, A., Davidson, B., Baldac, S., Howells, S., Walters, J., ... & Hill, A. E. (2020). A framework to support the development of quality simulation‐based learning programmes in speech–language pathology. International journal of language & communication disorders, 55(2), 287-300.
4. Hustad, J., Johannesen, B., Fossum, M., & Hovland, O. J. (2019). Nursing students’ transfer of learning outcomes from simulation-based training to clinical practice: A focus-group study. BMC nursing, 18, 1-8.
5. Hung, C. C., Kao, H. F. S., Liu, H. C., Liang, H. F., Chu, T. P., & Lee, B. O. (2021). Effects of simulation-based learning on nursing students’ perceived competence, self-efficacy, and learning satisfaction: A repeat measurement method. Nurse Education Today, 97, 104725.
6. Chernikova, O., Heitzmann, N., Stadler, M., Holzberger, D., Seidel, T., & Fischer, F. (2020). Simulation-based learning in higher education: A meta-analysis. Review of educational research, 90(4), 499-541.
7. Najjuma, J. N., Bajunirwe, F., Twine, M., Namata, T., Kyakwera, C. K., Cherop, M., & Santorino, D. (2020). Stakeholder perceptions about the establishment of medical simulation-based learning at a university in a low resource setting: a qualitative study in Uganda. BMC medical education, 20, 1-10.
8. Ross, S. (2021). Simulation-based learning: from learning theory to pedagogical application. Internet Journal of Allied Health Sciences and Practice, 19(4), 15.
9. Atesok, K., Hurwitz, S., Anderson, D. D., Satava, R., Thomas, G. W., Tufescu, T., ... & Marsh, J. L. (2019). Advancing Simulation‐Based Orthopaedic Surgical Skills Training: An Analysis of the Challenges to Implementation. Advances in orthopedics, 2019(1), 2586034.
10. Lababidi, H. M., Alzoraigi, U., Almarshed, A. A., AlHarbi, W., AlAmar, M., Arab, A. A., ... & AlAwad, Y. I. (2020). Simulation-based training programme and preparedness testing for COVID-19 using system integration methodology. BMJ simulation & technology enhanced learning, 7(3), 126.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Surjeet Sahoo, Shilpi Singh, RenukaJyothi. S.
Methodology: Surjeet Sahoo, Shilpi Singh, RenukaJyothi. S.
Software: Surjeet Sahoo, Shilpi Singh, RenukaJyothi. S.
Drafting - original draft: Surjeet Sahoo, Shilpi Singh, RenukaJyothi. S.
Writing - proofreading and editing: Surjeet Sahoo, Shilpi Singh, RenukaJyothi. S.