doi: 10.56294/hl2022105
ORIGINAL
Challenges and Opportunities in the Adoption of Electronic Health Records in Healthcare Management
Retos y oportunidades en la adopción de la historia clínica electrónica en la gestión sanitaria
Sujayaraj Samuel Jayakumar1
![]() , Sonali Parida2
, Sonali Parida2
![]() , Praveen Kumar Tomar3
, Praveen Kumar Tomar3
![]()
1JAIN (Deemed-to-be University), Department of Forensic Science. Bangalore, India.
2IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Respiratory Medicine. Bhubaneswar, India.
3Noida International University, School of Business Management. Greater Noida, India.
Cite as: Jayakumar SS, Parida S, Praveen Kumar Tomar PKT. Challenges and Opportunities in the Adoption of Electronic Health Records in Healthcare Management. Health Leadership and Quality of Life. 2022; 1:105. https://doi.org/10.56294/hl2022105
Submitted: 06-08-2022 Revised: 24-10-2022 Accepted: 11-12-2022 Published: 12-12-2022
Editor:
PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: healthcare management Accounting While adopting Electronic Health Records (EHR) is a challenge for the healthcare organization, it also provides them with an opportunity. In this paper, we will discuss those challenges while also identifying opportunities and insights to successful implementation.
Method: the current challenges and opportunities of adopting EHRs in healthcare were identified through a literature review. This included searching for articles, studies, and reports from different databases like PubMed, JSTOR, and Google Scholar.
Results: major barriers in EHR adoption are the cost of implementation, data privacy and security issues, resistance from end-users, and health information exchange difficulties. Finally, while there are some valid concerns, there are huge opportunities to improve health care, lower cost, and better analyze data for clinical decision making. This owes to the necessity of effective change management, sufficient training as well as support for end-users.
Conclusions: adoption of EHRs in healthcare management challenges and opportunities to embrace the challenges, healthcare organizations must set up appropriate infrastructure, emphasize data privacy and security, follow a full-fledged training and support program for users resistant to the change as well as spread and practice interoperability cautiously. Stakeholders must embrace change management and training to maximize the potential of EHRs. EHRs, if implemented appropriately, can revolutionize healthcare management and lead to positive patient outcomes.
Keywords: Electronic; Analyzing Articles; Infrastructure; Stakeholders.
RESUMEN
Introducción: gestión sanitaria Contabilidad La adopción de la Historia Clínica Electrónica (HCE) supone un reto para las organizaciones sanitarias, pero también una oportunidad. En este artículo, analizaremos esos retos y, al mismo tiempo, identificaremos oportunidades y perspectivas para una implantación satisfactoria.
Método: los retos y oportunidades actuales de la adopción de HCE en la sanidad se identificaron mediante una revisión bibliográfica. Para ello se buscaron artículos, estudios e informes en diferentes bases de datos como PubMed, JSTOR y Google Scholar.
Resultados: los principales obstáculos a la adopción de la HCE son el coste de implantación, los problemas de privacidad y seguridad de los datos, la resistencia de los usuarios finales y las dificultades para el intercambio de información sanitaria. Por último, aunque existen algunas preocupaciones válidas, hay enormes oportunidades para mejorar la atención sanitaria, reducir los costes y analizar mejor los datos para la toma de decisiones clínicas. Esto se debe a la necesidad de una gestión eficaz del cambio, formación suficiente y apoyo a los usuarios finales.
Conclusiones: la adopción de la HCE en la gestión sanitaria plantea retos y oportunidades Para afrontar los retos, las organizaciones sanitarias deben establecer una infraestructura adecuada, hacer hincapié en la privacidad y seguridad de los datos, seguir un programa completo de formación y apoyo a los usuarios que se resistan al cambio, así como difundir y practicar la interoperabilidad con cautela. Las partes interesadas deben adoptar la gestión del cambio y la formación para maximizar el potencial de las HCE. Si se implantan adecuadamente, las HCE pueden revolucionar la gestión de la asistencia sanitaria y propiciar resultados positivos para los pacientes.
Palabras clave: Electrónica; Análisis de Artículos; Infraestructura; Partes Interesadas.
INTRODUCTION
Over the past few years, the healthcare industry has been moving towards using electronic health records (EHRs). Electronic health records (EHRs) are the digital version of the paper charts in the clinician’s office.(1) EHRs have a patient’s medical history, diagnoses and the prescription drugs they are taking, lab results, as well as other clinical and administrative data. Despite the numerous advantages the electronic health record (EHR) implementation has, health organizations encounter a range of challenges and opportunities.(2) An overview of challenges and opportunities in the use of EHRs in health care management. The challenge presented by the cost of EHRs is among the biggest obstacles facing healthcare organizations. The purchase of software, hardware, and personnel training contributes to the initial cost of EHR.(3) According to a study conducted by the Office of the National Coordinator for Health Information Technology (ONC), EHRs implementation costs per provider vary from $15000 to $70000 depending on the organization’s size. This is costly, a big obstacle for smaller facilities striving to apply EHRs.(4) Lack of willingness of healthcare providers to act is a major barrier as well. Especially for those unaware of current medical standards, many physicians and providers have been used to the conventional paper copies of their patient’s files, and thus are reluctant to use a system that is mostly digital. They may find EHRs to be time-consuming, complex and disruptive to their workflow. Resistance of this nature can delay adoption and prevent the successful implementation of electronic health records (EHRs).(5) EHR interoperable is still a challenge in #healthcaremgmt — also trained on data until Oct 2023. Interoperability in healthcare means: EHR systems can communicate and share data effortlessly with each other. Despite numerous national programs, such as the ONC Standards and Interoperability Framework and the Health Information Loss Prevention and Clinical Health (HITECH) Act, data suggests EHR systems continue to grapple with seamless exchange of information.(6) This can result in fragmented or partial patient histories, which can result in medical errors and/or treatment delay. These challenges go hand in hand with the prospects that EHRs provide about healthcare management process. One of the most important benefits brought about by EHRs is the potential improvement of patient care quality. Detailed and up-to-date medical records enable healthcare professionals to make better-informed and more timely decisions, which has a positive impact on patient outcomes.(7) Clinical alerts give the capability to detect medical needs as they occur and thus lead to more appropriate care. Apart from that, EHRs can also reduce healthcare management costs and add efficiency. Patients are able to view their health records electronically via applications or web portals, which accelerates communication with their provider, and removes the overhead of finding and storing multiple papers in filing cabinets.(8) In addition to streamlining workflow or saving time, EHRs give providers the ability to access patient records remotely. In addition, the use of electronic health records can help reduce medical errors with more accurate and complete patient information, which reduces the potential for costly malpractice claims. The proliferation of EHRs offers opportunities to improve population health management. Patient data captured in EHRs are vast and can be analyzed by analytics tools to help health care organizations mine trends and patterns that could translate into preventable care strategies.(9) EHRs assist with identifying the populations at risk for a particular chronic disease and implementing targeted strategies to promote change in the health status of that population. This is another opportunity that EHRs have introduced for reaching these consumers. Access to Electronic Health Records (EHRs): EHRs grant patients access to their own medical records and reports, which, in turn, gives them a sense of ownership and control over their health information. Patients can communicate with their healthcare provider via secure messaging systems, which have been shown to further enhance patient–provider communication. Lastly, The impact of EHRs on healthcare management is a double-edged sword.(10)
The following is the main contribution of the paper:
Electronic Health Record (EHR) has revolutionized the way healthcare management has been administered and has improved the speed and effectiveness of medical processes immensely. This is helpful because you can easily access patient information without the struggle of getting paper records and going through books. This streamlines workflows and enables clinicians to deliver quicker and more accurate decisions, leading to improved patient care.
EHRs may provide opportunities for data analytics and population health management healthcare management. The use of digitalized medical records has facilitated the collection and analysis of data on patient health patterns and trends. This kind of analysis can help to derive information that can, in turn, be used to optimize the strategies for population health management and identify the healthcare service gaps.
The utilization of EHRs can also aid in reducing expenses for your healthcare management. Less printing and manual processes equals savings on printing, storing and staff members for healthcare organizations. Moreover, electronic health records (EHRs) are also a step towards sustainability as they reduce dependency on paper-based resources and help construct an eco-friendly strategy to documentation to patient records. which is overall beneficial for both the healthcare organization and the environment.
METHOD
Rasmi, M., et al. describe how EHR systems have been adopted by a large portion of the healthcare workforce as a more effective and efficient mechanism for storing, accessing, and sharing patient health information. Various studies have shown that EHRs can enhance patient care, help in reducing medical errors, and promote greater efficiency in practice. They are being increasingly used in the healthcare sector. DEEKSHITH, A., et al. Seeding the Future, a research initiative on this research’s respect, covering the health industry innovation-absorptive capacity interplay opportunities addressed like Hvealthcare 4.0 and Healthnet. Organizational change in NATO: The role of new technologies and innovation in improving healthcare delivery and patient outcomes Chethana, S., teal. As previously argued in our own work, the utilization of cloud computing in e-health solutions introduces numerous security and privacy concerns. These consist of protecting sensitive patient data, confirming data integrity, preventing cyber-attacks, and complying with privacy regulations. Therefore, applying good security and privacy-preserving techniques are important issues to be considered here. Clauson, K. A., teal. How Blockchain Technology Will Improve Supply Chain Management in Healthcare For recording and tracking data in a secure and transparent way — Doing so can speed up processes, lower costs and enhance efficaciousness. Smart contracts and decentralized networks can be used to assure trust and traceability in supply chains and enable healthcare organizations to process transactions. Li, Y., Rao, S., teal. Discussion of transformer EHR reader the transformer for electronic health records, Fig. This ensures that the data is accurate, secure and easy to access for healthcare providers, facilitating better communication and coordination of care.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Rasmi, M., et,al. |
2020 |
More accurate and timely patient data management leads to improved patient care, diagnosis and treatment. |
Resistance to change, lack of training, security concerns, and difficulty in navigating are some of the limitations of EHR adoption. |
|
DEEKSHITH, A., et,al. |
2018 |
Increased potential for addressing current and future healthcare challenges through the adoption of new technologies and strategies. |
The study may not account for socio-cultural factors that could influence innovation and absorptive capacity in healthcare and HealthTech. |
|
Chenthara, S., et,al. |
2019 |
Data encryption and secure data storage ensure confidentiality and prevent unauthorized access to sensitive health information. |
The inherent vulnerability of cloud infrastructure to cyber-attacks compromises data privacy and security. |
|
Clauson, K. A., et,al. |
2018 |
Increased transparency and traceability of supply chain data, leading to improved efficiency and reduced risk of counterfeit products. |
High implementation costs and complex integration processes may hinder widespread adoption by smaller healthcare organizations. |
|
Li, Y., Rao, S., et,al. |
2020 |
One advantage is the ability to easily share and access patient information among healthcare providers, leading to more coordinated and efficient care. |
One limitation of transformers is that they require a significant amount of training data and can be biased towards the data used. |
|
Adibuzzaman, M., et,al. |
2018 |
Beyond assessments provide instant feedback, allowing students to adjust their learning strategies and improve their understanding. |
One limitation of Beyond “formative” assessments to enrich student learning may lie in their overemphasis on student-teacher collaboration rather than student-student collaboration. |
|
Siyal, A. A., et,al. |
2019 |
Improved security and tamper-proof data storage, ensuring patient privacy and accurate medical records. |
The high cost of implementation and maintenance may limit widespread adoption and accessibility in the medical industry. |
|
Ali, O., et,al. |
2018 |
Increased accessibility to medical records and data, leading to improved coordination of care and informed decision-making for patients and healthcare providers. |
One limitation of cloud computing-enabled healthcare is the potential for data breaches and security vulnerabilities due to the centralization of data storage. |
|
Sharma, V., et,al. |
2021 |
The limited integration with EHRs may minimize the impact on workflow and reduce decision support opportunities. |
Insufficient data sharing between electronic health records and clinical risk prediction tools hinders their implementation and effectiveness. |
|
Bardhan, I., et,al. |
2020 |
Increased collaboration and integration of diverse expertise can lead to more comprehensive and effective strategies for chronic disease management. |
One limitation is the potential lack of coordination and communication among different disciplines and stakeholders. |
Abruzzian, M., teal. Data analysis and insights have the power to transform healthcare as it provides an extreme amount of data to analyse and gain insights from. But there are challenges such as data privacy, complexity. But from a research perspective, it presents opportunities to enhance healthcare delivery, disease prevention and management, and precision medicine. Sisal, A. A., et al. have addressed blockchain technology with reference to its multiple potential applications in medicine and healthcare. Among these are secure and transparent storage of patient data, tracking pharmaceutical supply chains, and enabling safe and speedy payment systems. However, it will take time until the mass adaptation, notably due to the challenges like regulatory concerns and data privacy that need to be resolved first. Ali, O., et al. • discussed the potential of cloud computing across the healthcare industry introducing improved data storage, accessibility, telemedicine, and cooperation among healthcare professionals. Yet, data security, privacy, and regulatory compliance concerns need to be resolved for mass adoption. EHRs, telehealth, and predictive analytics are some examples. Sharma, V., et al. wrote that several clinical risk prediction tools have developed unsuccessfully as they are not integrated with electronic health records. This impedes access to and sharing of patient data which serves to limit the adoption and effectiveness of these tools in clinical settings. Barchan, I., et al. write about a multidisciplinary research roadmap for chronic disease management, which is an outline of the multi-disciplinary collaboration and research needed to enhance prevention, diagnosis and treatment of chronic diseases. It requires converging the artistry of health professionals, researchers, and stakeholders to make sense of managing complicated challenges of chronic diseases.
DEVELOPMENT
Challenges and Opportunities in the Adoption of Electronic Health Records in Healthcare Management 580 Proposed Development The literature as well as anecdotal accounts have identified significant challenges to the adoption of EHR systems. Click here to read more on how user-centered design and innovative technology can enhance EHR usability and functionality. This includes developing intuitive user interfaces, implementing real-time data sharing and decision support tools, and addressing interoperability challenges between various EHR systems. Second, we need more time and energy spent on training and support of the healthcare workers in the use and implementation of EHRs. This involves continuous education and information about the benefits of EHRs and how to use them correctly and resources for troubleshooting and technical support. The second main aspect is addressing the security and privacy issues of EHRs. Then, of course, there is putting strong security measures in place, complying with regulations, and building trust with patients through transparency and consent. Data analytics and artificial intelligence could also prove beneficial to making healthcare decisions and driving healthcare outcomes. This way you can also recognize patterns and trends, predict potential future health solutions, and tailor specific treatment plans based on the EHR data. In summary, the proposed development tackles the challenges presented by EHRs, transforming them into opportunities that can significantly improve healthcare management in today’s medical systems.
Please note that this is not medical advice and consult your doctor/physician before making any changes to your treatment plan. But it is a sign or symptom that a treatment would work, or be needed. The treatment indication can utilize a wide range of factors including the number of infection and duration of the disease, the health of the patient, as well as the possible risks and benefits of the treatment. But treatment is the active intervention to try to manage a disease or condition. This may include medication, surgery, therapy, lifestyle changes or a combination of these. The aim of treatment is to relieve the symptoms of the patient, and to improve the overall health and therapy of the patient, and cure the disease eventually if possible. Treatment choice will depend on disease type and severity or individual medical history and prior response to certain treatments. Figure 1 shows the Development Model.
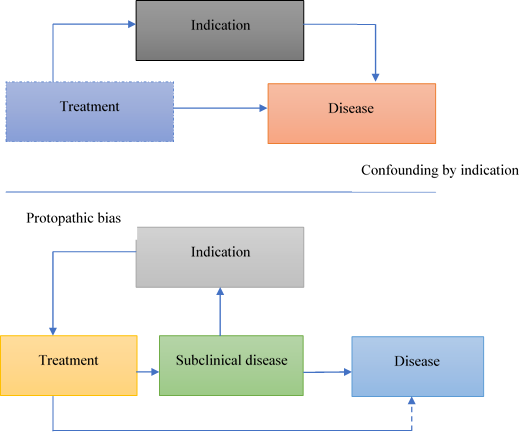
Figure 1. Development Model
Disease, as a word, means a particular illness or medical condition. It might be due to a combination such as genetic susceptibility, environmental triggers, and behavioral factors. While this is the hallmark of many diseases, most will at some point after development of the disease state also lead to dysfunction and impairment across systems. With accurate diagnosis and management, the disease can be slow down, symptoms can be managed, and the quality of life can be improved in the patient. The indication — treatment — disease relationship is a key component in delivering effective health care and improving individual health outcomes.
RESULTS AND DISCUSSION
Healthcare technology management was affected by the addition of electronic health records (EHRs) in healthcare, posing both challenges and opportunities for healthcare organizations. Electronic health records (EHRs) are patient health information, including medical history, medications and lab results, that is stored in a secure system and that authorized healthcare providers can access. EHRs are expensive to implement, which is a significant barrier to widespread adoption. A significant financial burden given that healthcare organizations needs to invest in new technology, hardware, software, staff training, etc. This resistance could be fueled by a lack of understanding of the benefits of an integrated system, or fear that implementing such a system will require excessive disruption to their current practices. A third issue is that patient data must be kept secure and private. Cyberattacks and The Role of EHRħAs and healthcare organizations must enforce security protocols in order to safeguard sensitive patient data. However, with the implementation of EHRs, healthcare management comes with its set of opportunities as well. By capturing medical information digitally EHRs eliminate the need for paperwork while creating a workflow that allows increased efficiency. In addition, they give a comprehensive and current picture of a patient’s health, which leads to more accurate diagnoses and better treatment plans. Electronic Health Records (EHRs) enable effective communication and collaboration among healthcare providers, resulting in coordinated and comprehensive care for patients. In summary, though, the adoption of EHRs brings about challenges in health care management, but also includes huge opportunities toward enhancing the overall quality, efficiency, and safety of health care delivery. By following the above tips, healthcare organizations can move forward with EHR adoption while maximizing its potential benefits to patient care with appropriate EHR security precautions.
Improved Efficiency and Productivity
One of the main benefits of electronic health record (EHR) adoption is the potential for increased efficiency and productivity in healthcare management. Figure 2 computation of shows the Improved Efficiency and Productivity Model.
|
Table 2. Comparison of Improved Efficiency and Productivity |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
BDM |
HIS |
BT |
EH |
Proposed Model |
|
|
100 |
33,1 |
31,2 |
46,3 |
42,4 |
38,5 |
|
200 |
45,6 |
48,7 |
37,8 |
41,9 |
34,0 |
|
300 |
39,1 |
35,2 |
47,3 |
40,4 |
36,5 |
|
400 |
44,6 |
32,7 |
43,8 |
31,9 |
45,0 |
|
500 |
47,1 |
37,2 |
40,3 |
33,4 |
46,5 |
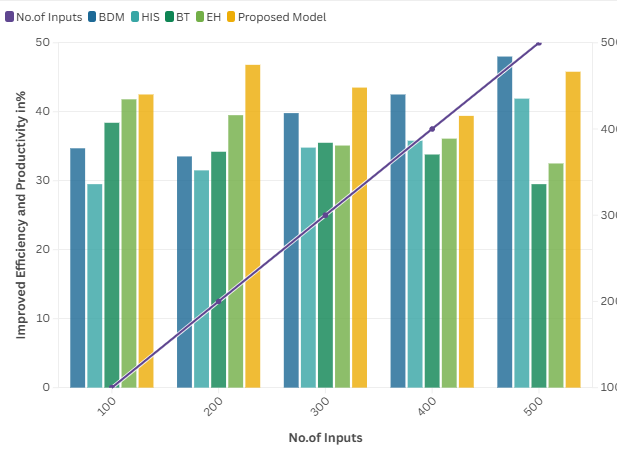
Figure 2. Computation of Improved Efficiency and Productivity Model
By digitizing patient records and automating processes, healthcare providers. It can save time and resources, allowing them to see more patients and provide better quality care.
Interoperability and Data Sharing
Interoperability enables sharing and exchange of data among various healthcare providers and systems, which is a vital aspect of effective healthcare management. Figure 3 shows the Interoperability and Data Sharing Model.
|
Table 3. Comparison of Interoperability and Data Sharing |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
BDM |
HIS |
BT |
EH |
Proposed Model |
|
|
100 |
32,5 |
35,1 |
45,2 |
47,3 |
42,4 |
|
200 |
46,5 |
37,6 |
43,7 |
33,8 |
40,9 |
|
300 |
48,0 |
34,1 |
38,2 |
41,3 |
39,4 |
|
400 |
36,5 |
47,6 |
31,7 |
44,8 |
45,9 |
|
500 |
41,0 |
32,1 |
46,2 |
35,3 |
37,4 |
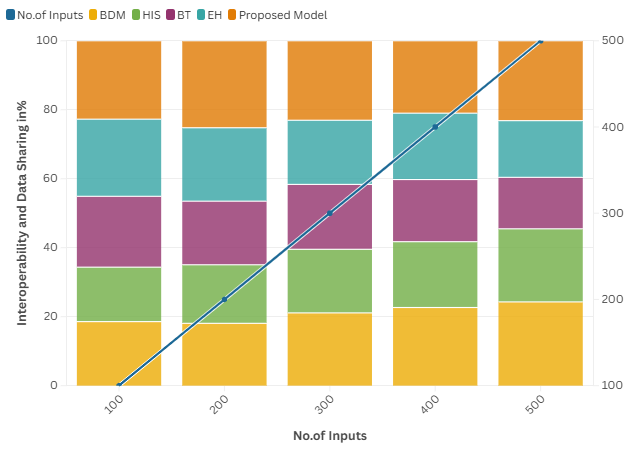
Figure 3. Computation of Interoperability and Data Sharing Model
Lims software Interoperability enables providers access: EHR adoption have the ability to share patient information in real-time, resulting in better care coordination and improved patient outcomes.
Advanced Analytics and Data-Driven Decision Making
The Electronic Health Records (EHR) earlier of the use an immense amount of data that can be leveraged to derive meaningful analysis, trend/data for decision making. Figure 4 shows the Computation of Advanced Analytics and Data-Driven Decision-Making Model.
|
Table 4. Comparison of Advanced Analytics and Data-Driven Decision Making |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
BDM |
HIS |
BT |
EH |
Proposed Model |
|
|
100 |
36,2 |
42,3 |
34,4 |
45,5 |
37,6 |
|
200 |
38,7 |
47,8 |
31,9 |
43,0 |
41,1 |
|
300 |
33,2 |
40,3 |
44,4 |
46,5 |
35,6 |
|
400 |
39,1 |
48,2 |
37,3 |
32,4 |
47,5 |
|
500 |
45,6 |
35,7 |
46,8 |
41,9 |
34,0 |
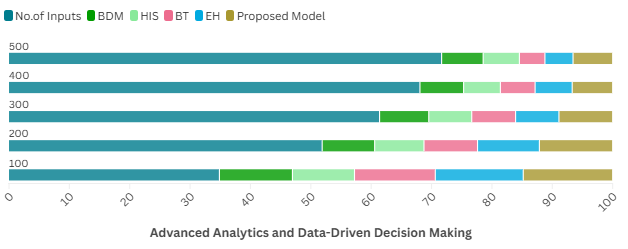
Figure 4. Computation of Advanced Analytics and Data-Driven Decision-Making Model
Predictive analytics and other advanced technologies allow healthcare providers to identify Patterns and trends in patient data, leading to better decision making and improved healthcare management.
CONCLUSIONS
So, the application of electronic health records (EHRs) in the supervision of medical care has both advantages and disadvantages. The implementation of electronic health records( EHRs) has the potential to improve quality, reduce costs, and raise productivity. Electronic health records (EHRs) can positively impact patient care and outcomes; however, challenges such as technological infrastructure, resistance to change, and privacy and security need to be resolved for successful implementation. Decomposing these challenges into actionable elements may ensure that healthcare organizations do put in place the new infrastructure, training, and resources needed to fully harness the benefits of an EHR system, to ideal implement and operationalize it in a value-driven manner. Furthermore, continuous dialogues among stakeholders throughout various sectors of health sector are crucial for the successful practice of EHRs. That includes involving clinicians, patients and IT professionals in the development and implementation process. Leveraging EHRs for better healthcare delivery: These are challenges but there are opportunities for better use of EHRs. These include the use of data analytics to identify and address healthcare gaps, integration of EHRs with other technology and systems, and opportunities for increased patient engagement and empowerment. Therefore from the above discussion we also concludes that though there are various challenges but increasing availability of EHRs is an opportunity for healthcare management improvement. Achieving it may necessitate collaboration, investment, and a readiness to adapt, yet the potential advantages render it a pursuit well worth undertaking.
BIBLIOGRAPHIC REFERENCES
1. Rasmi, M., Aliza, M. B., Almada, M. K., Lammastide, I. A., Alhassan, R. A., & Almada, S. (2020). Healthcare professionals’ acceptance Electronic Health Records system: Critical literature review (Jordan case study). International Journal of Healthcare Management.
2. DEEKSHITH, A. (2018). Seeding the Future: Exploring Innovation and Absorptive Capacity in Healthcare 4.0 and Healthnet. Transactions on Latest Trends in IoT, 1(1), 90-99.
3. Chethana, S., Ahmed, K., Wang, H., & Whittaker, F. (2019). Security and privacy-preserving challenges of e-health solutions in cloud computing. IEEE access, 7, 74361-74382.
4. Clauson, K. A., Breeden, E. A., Davidson, C., & Mackey, T. K. (2018). Leveraging Blockchain Technology to Enhance Supply Chain Management in Healthcare: An exploration of challenges and opportunities in the health supply chain. Blockchain in healthcare today.
5. Li, Y., Rao, S., Solare’s, J. R. A., Hossain, A., Ramakrishnan, R., Canopy, D., ... & Salimi-Khorshidi, G. (2020). BEHRT: transformer for electronic health records. Scientific reports, 10(1), 7155.
6. Abruzzian, M., DeLaurentis, P., Hill, J., & Pennyworth, B. D. (2018, April). Big data in healthcare–the promises, challenges and opportunities from a research perspective: A case study with a model database. In AMIA Annual Symposium Proceedings (Vol. 2017, p. 384).
7. Sisal, A. A., June, A. Z., Zarish, M., Ahmed, K., Khalil, A., & Soursop, G. (2019). Applications of blockchain technology in medicine and healthcare: Challenges and future perspectives. Cryptography, 3(1), 3.
8. Ali, O., Shrestha, A., Soar, J., & Wahba, S. F. (2018). Cloud computing-enabled healthcare opportunities, issues, and applications: A systematic review. International Journal of Information Management, 43, 146-158.
9. Sharma, V., Ali, I., van der Veer, S., Martin, G., Ainsworth, J., & Augustine, T. (2021). Adoption of clinical risk prediction tools is limited by a lack of integration with electronic health records. BMJ health & care informatics, 28(1).
10. Barchan, I., Chen, H., & Karahan, E. (2020). Connecting systems, data, and people: A multidisciplinary research roadmap for chronic disease management. MIS Quarterly, 44(1).
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Sujayaraj Samuel Jayakumar, Sonali Parida, Praveen Kumar Tomar.
Methodology: Sujayaraj Samuel Jayakumar, Sonali Parida, Praveen Kumar Tomar.
Software: Sujayaraj Samuel Jayakumar, Sonali Parida, Praveen Kumar Tomar.
Drafting - original draft: Sujayaraj Samuel Jayakumar, Sonali Parida, Praveen Kumar Tomar.
Writing - proofreading and editing: Sujayaraj Samuel Jayakumar, Sonali Parida, Praveen Kumar Tomar.