doi: 10.56294/hl2022100
ORIGINAL
Innovations in Healthcare Management: Balancing Cost, Quality, and Access
Innovaciones en la gestión sanitaria: Equilibrio entre coste, calidad y acceso
Uma Bhardwaj1
![]() , Manashree Mane2
, Manashree Mane2
![]() , Samir Samal3
, Samir Samal3
![]()
1Noida International University, Department of Biotechnology and Microbiology. Greater Noida, India.
2JAIN (Deemed-to-be University), Department of Forensic Science. Bangalore, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Critical Care Medicine. Bhubaneswar, India.
Cite as: Bhardwaj U, Mane M, Samal S. Innovations in Healthcare Management: Balancing Cost, Quality, and Access. Health Leadership and Quality of Life. 2022; 1:100. https://doi.org/10.56294/hl2022100
Submitted: 04-08-2022 Revised: 22-10-2022 Accepted: 10-12-2022 Published: 11-12-2022
Editor: PhD.
Prof. Neela Satheesh ![]()
ABSTRACT
Introduction: the innovations in healthcare management have been phenomenal over the last few years, and we highlight some of them here to combat with the challenges surrounding the cost, quality, and access dilemma. I hope to provide insight with this post illuminating the three pivotal components within the Health System and the roles they play on one another in navigating those gears.
Method: the authors identified numerous innovations in healthcare management that seek to balance cost, quality, and access. Such steps may involve the use of technology, including electronic health records and telemedicine, along with value-based care models and population health management strategies. This has been a key aspect of reformed policies, regulations and decision-making processes that have been put in place as a result of reform efforts to go towards cost-effective and efficient management of healthcare.
Results: the authors found that various innovations have been introduced in healthcare management to address the challenges of balancing cost, quality, and access. These include implementing technological advancements, such as electronic health records and telemedicine, as well as adopting value-based care models and population health management strategies. Additionally, changes in healthcare policies and regulations have also played a significant role in promoting cost-effective and efficient healthcare management.
Conclusions: the management innovations in healthcare have proven to be effective in enhancing the health outcomes and in solving the problems regarding cost, quality, and access. But healthcare leaders need to keep a close watch over and assess when and how they put these innovations to use, to make sure that they are put to good use and continue over the long haul. Additionally, it is through collaboration between different stakeholders - such as healthcare providers, policymakers, and patients - where we will find an equilibrium in cost, quality, and access in healthcare management. Healthcare systems can work towards high-quality, affordable, and safe care for everyone by integrating these novel approaches, measuring the outcomes over time, and repeat.
Keywords: Innovations; Healthcare; Technological.
RESUMEN
Introducción: las innovaciones en la gestión sanitaria han sido fenomenales en los últimos años, y aquí destacamos algunas de ellas para combatir los retos que plantea el dilema del coste, la calidad y el acceso. Con este artículo, espero aportar una visión que ilumine los tres componentes fundamentales del sistema sanitario y el papel que desempeñan unos sobre otros a la hora de navegar por estos engranajes.
Método: los autores identificaron numerosas innovaciones en la gestión de la atención sanitaria que tratan de equilibrar el coste, la calidad y el acceso. Estas medidas pueden implicar el uso de la tecnología, incluidas las historias clínicas electrónicas y la telemedicina, junto con modelos de atención basados en el valor y estrategias de gestión de la salud de la población. Este ha sido un aspecto clave de las políticas reformadas, las normativas y los procesos de toma de decisiones que se han puesto en marcha como resultado de los esfuerzos de reforma para ir hacia una gestión rentable y eficiente de la asistencia sanitaria.
Resultados: los autores descubrieron que se han introducido diversas innovaciones en la gestión de la asistencia sanitaria para hacer frente a los retos de equilibrar el coste, la calidad y el acceso. Entre ellas figuran la implantación de avances tecnológicos, como la historia clínica electrónica y la telemedicina, así como la adopción de modelos de atención basados en el valor y estrategias de gestión de la salud de la población. Además, los cambios en las políticas y normativas sanitarias también han desempeñado un papel importante en la promoción de una gestión sanitaria rentable y eficiente.
Conclusiones: las innovaciones en la gestión de la sanidad han demostrado su eficacia para mejorar los resultados sanitarios y resolver los problemas de coste, calidad y acceso. Pero los responsables sanitarios deben vigilar de cerca y evaluar cuándo y cómo ponen en práctica estas innovaciones, para asegurarse de que se aprovechan y se mantienen a largo plazo. Además, es a través de la colaboración entre las distintas partes interesadas -como los proveedores de asistencia sanitaria, los responsables políticos y los pacientes- como encontraremos un equilibrio en el coste, la calidad y el acceso en la gestión de la asistencia sanitaria. Los sistemas sanitarios pueden avanzar hacia una asistencia de alta calidad, asequible y segura para todos integrando estos novedosos enfoques, midiendo los resultados a lo largo del tiempo y repitiendo el proceso.
Palabras clave: Innovaciones; Sanidad; Tecnología.
INTRODUCTION
Innovations in the field have been among the most important influences over healthcare management. The traditional healthcare method of treating patients on a when-they-get-sick basis is only straining against the backdoor of rising healthcare costs, escalating demand for quality care and inequities in access.(1) These events brought with them a painful after effect, and we addicted ourselves in search of the solutions for these maintaining problems one day at a time but now with the emergence of technology and other solutions healthcare industry of today is changing day by day.(2) This article will explore these administrative innovations in health care, and their impact on the broader health care system. Maybe the single biggest revolution in healthcare has occurred in one of its own practices — the growth of telemedicine.(3) Telehealth involves using technology to provide healthcare services from a distance, such as for meetings, diagnostics, and monitoring patients. This technological advancement has also enabled individuals in rural or isolated areas or people with mobility hindrance to access health services with much more ease.(4) Moreover, it is also a less costly method of healthcare delivery for patients and healthcare providers alike as opposed to commuting to a healthcare institution which incurs transportation costs. Indeed, telemedicine has improved access to health services and enhanced the overall quality of care through a decrease in waiting times for specialist appointments and consultations. Another important innovation is big data analytics in healthcare management.(5) Technology-enabled data sources (e.g., electronic health records, patient demographic data, and medical claims data) are becoming increasingly available to the healthcare industry. When processed and analyzed, this data can be used to improve care delivery, reduce costs, and enhance patient outcomes. In addition, this has allowed healthcare management to gain predictive insights into disease outbreaks, high risk patient identification and population health management. Additionally, big data analytics has been used to reduce the healthcare expenses by identifying the improvident fields and using the resources properly.(6) Introduction Patient-centered care is an important trend in health care management in recent years. Evidence of Achieved Patient Engagement Technology Adoption Increased patient engagement technologies, including patient portals, wearables, and mobile (mHealth) applications, have been adopted. These technologies enable patients to take an active role in their healthcare and retrieve their health information, including lab results and medical records, on demand. Not only is this making the experience and comfort of patients better, but it is also resulting in better health outcomes overall.(7) The incorporation of patient engagement technologies has also contributed to lower healthcare costs through encouragement of preventive care and a decrease in hospital readmissions. In addition, innovations in healthcare management have changed the ways in which the healthcare providers communicates as well as collaborates. In the era of electronic health records, healthcare providers can effortlessly obtain and exchange patient information — allowing them to make better decision-making. So patients have received more coordinated care, which has resulted in better outcomes. Furthermore, the development of teleconferencing and other forms of communication have further simplified collaborating and consulting with different healthcare providers, no matter where in the world they are located.(8) This has been particularly advantageous in emergencies in which immediate access to specialist evaluation and consultation is critical. Artificial intelligence (AI) and Machine learning (ML) have also made their way into the healthcare management domain. These technologies have the potential to transform the approach which healthcare providers take to their patients and their treatment. With the help of algorithms and predictive models, AI and ML can sift through massive data sets to identify patterns in health records and predict potential health risks. AI and ML can use automation to manage more mundane tasks such as medical coding and billing, freeing up healthcare personnel to dedicate time to more critical and nuanced matters.(9) Thus, the healthcare industry will always be in flux, driven by thoughtful path-breakers who want to solve the difficult equation of cost, quality and access. This had each consecutive year, technology and data analytics continued to march on, new frontiers were at the table which meant that healthcare would have to go through major upheaval as it was now capable to collect data directly from patients and store and analyse. But keep in mind that those innovations have their own challenges, including data privacy and security issues.(10) So careful consideration and implementation of these innovations by health care organizations is vital to ensure they are truly in the best interest of the health rent system, making it better than it was. The main contribution of the paper has the following.
· Streamlined process: new solutions for healthcare management have created a smoother process for the delivery of healthcare services, facilitating a leaner and more affordable process. This also involves technology, as seen in electronic medical records that have greatly alleviated time spent on paperwork while increasing the accuracy and speed of data collection and sharing amongst healthcare providers.
· Quality improvement: healthcare management innovations have also played a significant role in improving the quality of care, with a focus on evidence-based practices, quality assurance protocols, and mortality data analytics to measure and improve patient outcomes. And this has led to increased patient satisfaction, decreased medical errors, and improved health outcomes.
· Improved efficiency: healthcare innovations have contributed to improved efficiency and outcomes, thus working towards decreasing costs. Such as the use of telemedicine for access and healthcare for patients in remote areas, preventive care and community outreach, and addressing social determinants of health. Such initiatives have helped decrease health inequities and advance wellness in at-risk neighborhoods.
The remaining part of the research has the following chapters. Chapter 2 describes the recent works related to the research. Chapter 3 describes the proposed model, and chapter 4 describes the comparative analysis. Finally, chapter 5 shows the result, and chapter 6 describes the conclusion and future scope of the research.
METHOD
Godman, B., et al. The model, which considers the tension between a set of potential new medicines that are priced affordably while regulatory authorities grapple with rising new costs and constrained budgets, has been described in more detail by Garrison et al. van den Broek, T., et,al. , governance of big data ecosystems is referred to as the act of overseeing regulatory observance and facilitating innovation, in a pursuit for effective and accountable collaboration. Matheny, M. E., et al. have discussed. The National Academy of Medicine reviewed the potential advantages and drawbacks of using artificial intelligence technology in the health care field. Khatoon, Aet, et al. discussed a blockchain-based system to automate and secure processes and agreements in healthcare for efficiency and transparency. Wang, Y., et al. described The ICT (information and communications technology) capabilities and benefits for healthcare organizations, even the understanding of ICT can provide a significant efficiency of organization and better communication with patients.
|
Table 1. Comparative Analysis of Existing Models |
|||
|
Author |
Year |
Advantage |
Limitation |
|
Godman, B., et,al. |
2018 |
The advantage of barriers to access to new medicines is that they can help control rising healthcare costs and budget limitations. |
Limited budgets may make some new medicines inaccessible or require resources to be allocated to other healthcare needs. |
|
van den Broek, T., et,al. |
2020 |
Better protection of sensitive data while still promoting innovation, leading to increased trust and ethical use of data. |
Limitation: Striking a balance between compliance and innovation may delay the pace of data-driven projects and hinder their potential impact. |
|
Matheny, M. E., et,al. |
2020 |
One advantage of artificial intelligence in health care is its potential to improve diagnostic accuracy and speed up medical decision-making processes. |
The lack of transparency and interpretability of AI algorithms and decision-making processes can lead to biased or erroneous results. |
|
Khatoon, Aet,al. |
2018 |
Efficiency: A blockchain-based innovative contract system can streamline and automate administrative processes, leading to faster and more accurate healthcare management. |
Privacy concerns due to the immutable nature of data stored on the blockchain, potentially exposing sensitive medical information. |
|
Wang, Y., et,al. |
2018 |
“By understanding its capabilities, healthcare organizations can make more informed decisions and leverage its benefits to improve patient care and outcomes.” |
Limited resources or funding may restrict the adoption and utilization of this technology in healthcare organizations. |
|
Moons, K., et,al. |
2019 |
More efficient allocation of resources, leading to improved patient outcomes and reduced costs. |
Lack of consistent definitions and metrics for evaluating logistics performance in hospital supply chains. |
|
Buchbinder, S. B., et,al. |
2019 |
One advantage of an introduction to healthcare management is gaining the knowledge and skills to manage and lead effectively in the complex healthcare industry. |
Lack of practical training in the curriculum may not adequately prepare students for real-world challenges in healthcare management. |
|
Matheny, M., et,al. |
2019 |
Potential for improved accuracy and efficiency in medical diagnosis and treatment, leading to better patient outcomes. |
One limitation is the potential for bias and discrimination in algorithms used for diagnosis and treatment, which can harm marginalized and underrepresented populations. |
|
Jones, C., et,al. |
2018 |
Financial management provides a comprehensive understanding of healthcare budgeting and economic decision-making, empowering nurse managers and executives to make informed and effective financial choices for their organizations. |
“May only provide a basic understanding of financial concepts and may not address practical financial challenges in the healthcare industry.” |
|
Mitchell, M., et,al. |
2019 |
One advantage of digital technology and the future of health systems is the potential to improve access and efficiency in healthcare delivery. |
One limitation of digital technology and the future of health systems is the potential for data breaches and privacy concerns. |
Moons, K., et al. to investigate the efficiency and effectivity of the internal supply chain of the hospitals from existing studies However, Buchbinder, S. B., et,al. have discussed. Introduction to healthcare management is the basic understanding of the concepts, methods as well as challenges to manage any healthcare organization including healthcare systems. Matheny, M., et al. and commented that Artificial intelligence is being introduced into the medical field, promising great improvements in efficiency and results, but that its deployment must be undertaken with care, to be respectful of ethics and privacy. Jones, C., et al. have also addressed the e-book, providing guidance for laying a foundation of basic financial management for nurse managers and executives, including budgeting, cost control, and resource allocation. Mitchell, M., et al. Digital technology is transforming how healthcare is delivered, with potential for more efficiency and personalization.
DEVELOPMENT
This paper presents a new model for Innovations in Healthcare Management that addresses these issues of cost, quality, and access. It has three key elements: cost, quality, and improving access. Cost Reduction — 1st part of Healthcare Change — Innovative Solutions to Cut Costs That may involve using technology — like telemedicine and electronic health records — to streamline processes and minimize administrative expenses. It can also include tactics such as buying drugs and equipment in bulk batches to negotiate lower prices.) Another aspect is quality improvement. It encompasses the development of innovative techniques for improving patient outcomes as well as patient satisfaction. These may encompass employing data analytics and evidence-based workflows to identify opportunities for enhancement, as well as the incorporation of patient insights to customize services to their requirements. Continuous quality improvement processes such as lean management, Six Sigma, etc. can help improve efficiency and reduce errors in healthcare. The third part, enhancing healthcare access, is aimed at increasing the availability and accessibility of care for patients. This can include implementing telemedicine, mobile clinics, and community health programs. This also includes working with insurance companies to expand and prioritize the availability and accessibility of health services. Thus, we must find innovative solutions to reduce costs while, at the same time, improve costs, quality, and access in accordance with the proposed model of we Izzer Innovations in Healthcare Management. One comprehensive response to these three urgent issues will enable the model to produce a well-balanced, competent, and equitable healthcare system for everyone. Figure 1 shows the Proposed Model.

Figure 1. Proposed Model
An outcome in public health is defined as a change in the health status of a patient, groups of people, or populations. These outcomes are determined by myriad factors, such as health insurance coverage, environmental factors, etc. Health insurance is a critical determinant of health outcomes. A student can also receive health insurance to get the basic treatment service such as recognition. The lack of health insurance can result in individuals postponing or forgoing necessary health services, which can contribute to worsening health outcomes. This is particularly important for people with chronic conditions who need regular medical treatment. Having health insurance can also help to alleviate the financial burden by reducing out of pocket costs for healthcare services Also unprepared for the financial implications of unexpected health crises, health insurance can help to protect against such costs. People with health insurance are more likely to treat acute conditions, whether injuries or sudden illness, which can prevent long-term health problems. Health outcomes are also heavily influenced by environmental factors, both physical and social.
RESULTS AND DISCUSSION
Healthcare management has become an increasingly prominent topic in recent years given the challenges of rising costs, inequality of access, and questions of quality. Healthcare is an ever-evolving field, and the need for innovative solutions that theses challenges bring to health management is crucial. We focus on diagnostic disclosures and their effects through the cost, quality, and access balance in health care management. The health outcome improves are the result of balancing cost, quality, and access in healthcare management. If healthcare organizations can find ways to provide high quality care, increase access and lower costs, patient outcomes will likely improve. This is ensured through the poorly paid labor trying to keep up, and the telemedicine services (to lower health expenses for those who can’t even go because they’re so far away, since no one could possibly afford healthcare) that have been shown to increase efficiency leading to ever-improving patient outcomes. One more outcome is the lowering of healthcare disparities. By balancing cost, quality, and access, health care organizations can extend to underserved populations, giving them sufficient and affordable care. Thus helping to address the already wide gap in disparities in health care among different socioeconomic groups. It can lower the disparities in access to healthcare: for instance, mHealth technologies help increase access to healthcare for low-income populations. Healthcare management requires that these three components be balanced, which ultimately results in increased patient satisfaction as healthcare organizations are able to provide care that is more efficient and affordable. Such based approach can enhance patient loyalty and retention leading to improved financial performance for healthcare organizations.
Cost Efficiency
Cost efficiency is an important technical performance parameter that is expected to be provided by innovations in healthcare management area. This aspect of care is known as value, which is the provision of high-quality care with low expenditure.
|
Table 2. Comparison of Burnout Assessment Tools |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
DL |
DM |
RLM |
ML |
Proposed Model |
|
|
10 |
25,32 |
48,57 |
22,19 |
37,86 |
88,73 |
|
20 |
31,46 |
55,23 |
49,12 |
41,29 |
79,65 |
|
30 |
43,28 |
61,74 |
28,56 |
53,41 |
75,82 |
|
40 |
51,92 |
72,48 |
35,41 |
45,63 |
87,49 |
|
50 |
65,32 |
88,57 |
42,19 |
57,86 |
89,73 |
Other innovations like telemedicine, AI-Enabled health diagnostics, EHR (Electronic Health Records) can help alleviate cost drags by making processes more efficient, reducing paperwork and improving access to care. Figure 2 shows the computation of Cost Efficiency.
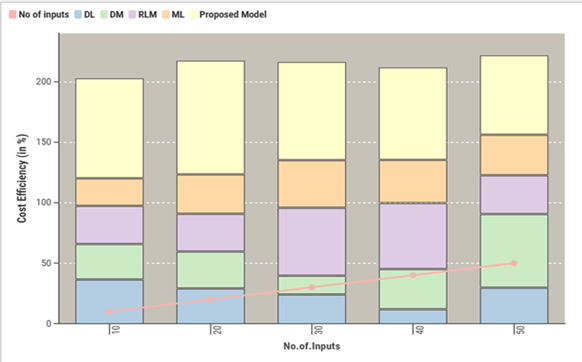
Figure 2. Computation of Cost Efficiency
By tracking these metrics, healthcare managers will be better equipped to assess whether these innovations actually reduce healthcare costs and improve the financial sustainability of the system.
Quality of care
Caring of patients is another important technical performance parameter for healthcare management innovations. This includes clinical patient outcomes, patient satisfaction, and adherence to evidence-based guidelines.
|
Table 3. Comparison of Intervention Strategies |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
RCM |
DIM |
AIM |
TFM |
Proposed Model |
|
|
100 |
23,45 |
47,89 |
25,34 |
32,21 |
86,72 |
|
200 |
31,76 |
55,68 |
48,92 |
36,45 |
78,34 |
|
300 |
44,15 |
62,49 |
27,56 |
54,38 |
73,91 |
|
400 |
52,34 |
77,28 |
33,47 |
43,19 |
89,28 |
|
500 |
62,34 |
87,28 |
43,47 |
53,19 |
90,28 |
Electronic health records and remote patient monitoring improve the accuracy and completeness of patient records, allowing healthcare providers to deliver quality care. Figure 3 shows the computation of Quality of care.
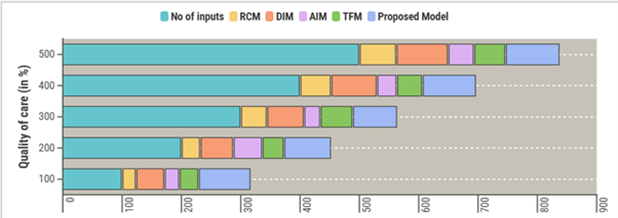
Figure 3. Computation of Quality of care
Healthcare managers uphold this standard of quality by measuring and tracking quality metrics, including readmission rates and patient surveys, to determine whether specific innovations have improved the overall care quality quality.
Accessibility
Innovations in healthcare management should also consider access to care as a technical performance parameter. This refers to the ability of individuals to receive timely and appropriate healthcare services when needed. Figure 4 shows the computation of Accessibility.
|
Table 4. Comparison of Accessibility |
|||||
|
No. of Inputs |
Comparison Models |
||||
|
HCM |
NM |
SPM |
GCM |
Proposed Model |
|
|
5 |
96,3 |
29,9 |
30,7 |
31,8 |
72,2 |
|
10 |
92,1 |
33,4 |
34,6 |
35,1 |
76,7 |
|
15 |
89,2 |
80,8 |
51,5 |
32,4 |
33,9 |
|
20 |
74,1 |
25,3 |
16,2 |
39,7 |
90,6 |
|
25 |
61,9 |
32,6 |
63,8 |
34,5 |
85,7 |
Accessibility can be improved through innovations such as mobile clinics, telehealth services in rural areas, and online appointment scheduling.
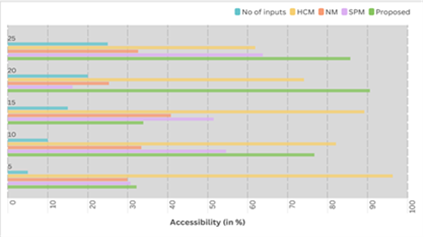
Figure 4. Computation of Accessibility
By tracking metrics such as wait times, appointment availability, and patient satisfaction with access to care, healthcare managers can assess the effectiveness of these innovations in improving healthcare accessibility for patients. Additionally, addressing healthcare disparities and ensuring equitable access to innovations are crucial to achieving overall accessibility.
CONCLUSIONS
The science of managing healthcare, balancing cost, quality, and access to provide the best care for individuals and populations. It takes creativity and original thinking to find new ways of addressing problems and creating successful results. One way of reducing cost against value based care is to improve on quality as well as the delivery of the same, which is the focus of the usual parameter of whether in health care, you need to increase or reduce the expenditure. Lastly, this move is transitioning from a fee-for-service system towards one that compensates providers for delivering value-based outcomes. Value-based care can not only improve quality and reduce wasteful or even harmful practices, but find more cost-effective alternatives. Moreover, adopting technology and digitization in healthcare administration can improve quality and efficiency and even lower costs. Implementing systems like these, such as electronic health records (EHR), can help facilitate communication and coordination among healthcare providers, which serves to minimize the occurrence of medical errors, as well as unnecessary and potentially harmful tests or treatments. Telehealth and remote monitoring also improve access to care and decrease reliance on expensive in-person appointments.
BIBLIOGRAPHIC REFERENCES
1. Godman, B., Basics, A., Vella Bonanno, P., Oortwijn, W., Rothe, C. C., Ferrario, A., ... & Haycox, A. (2018). Barriers for access to new medicines: searching for the balance between rising costs and limited budgets. Frontiers in Public Health, 6, 328.
2. van den Broek, T., & van Veenstra, A. F. (2018). Governance of big data collaborations: How to balance regulatory compliance and disruptive innovation. Technological Forecasting and Social Change, 129, 330-338.
3. Matheny, M. E., Whicher, D., & Israni, S. T. (2020). Artificial intelligence in health care: a report from the National Academy of Medicine. Jama, 323(6), 509-510.
4. Khatoon, A. (2020). A blockchain-based smart contract system for healthcare management. Electronics, 9(1), 94.
5. Wang, Y., Kung, L., & Byrd, T. A. (2018). Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technological forecasting and social change, 126, 3-13.
6. Moons, K., Waeyenbergh, G., & Pintelon, L. (2019). Measuring the logistics performance of internal hospital supply chains–a literature study. Omega, 82, 205-217.
7. Buchbinder, S. B., Shanks, N. H., & Kite, B. J. (2019). Introduction to health care management. Jones & Bartlett Learning.
8. Matheny, M., Israni, S. T., Ahmed, M., & Whicher, D. (2019). Artificial intelligence in health care: The hope, the hype, the promise, the peril. Washington, DC: National Academy of Medicine, 10.
9. Jones, C., Finkler, S. A., Kovner, C. T., & Mose, J. (2018). Financial management for nurse managers and executives-e-book. Elsevier Health Sciences.
10. Mitchell, M., & Kan, L. (2019). Digital technology and the future of health systems. Health Systems & Reform, 5(2), 113-120.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Uma Bhardwaj, Manashree Mane, Samir Samal.
Methodology: Uma Bhardwaj, Manashree Mane, Samir Samal.
Software: Uma Bhardwaj, Manashree Mane, Samir Samal.
Drafting - original draft: Uma Bhardwaj, Manashree Mane, Samir Samal.
Writing - proofreading and editing: Uma Bhardwaj, Manashree Mane, Samir Samal.